Abstract
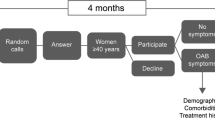
There is a continuing debate on the accurate prevalence estimates of overactive bladder (OAB) among different ethnicities and regions. The aims of our study were to determine the prevalence of OAB, associated risk factors, and the impact of OAB on the quality of life and sexual function of Iranian women. A total of 8748 women between 15 and 55 years of age enrolled in this cross-sectional study. The definition of the 2002 International Continence Society (ICS) was applied to assess the prevalence of OAB. All participants underwent a detailed history and physical examination that included an evaluation of quality of life, coping strategies and treatment-seeking behavior, laboratory tests, urinalysis and current or previous therapy. The degree of bother was quantified using s visual analog scale (VAS). The overall prevalence of OAB was found to be 18.2% and increased with age from 10.9% in adults aged 15–29 years to 26.2% in those aged >50 years old (test for trend, P = 0.001). A negative impact of OAB on sexual function was reported by 72.3% of the women. Frequency was the most commonly reported symptom (67% of women), followed by urgency (54%). Subjects with OAB had a higher prevalence of anxiety (28.2 vs. 8.8%; P = 0.001), depression (38.2 vs. 18.2%; P = 0.02) and tiredness (16.4 vs. 2.7%; P = 0.001), and they reported significant impairment in carrying out household chores (P = 0.01), physical activities (P = 0.01) and work-related activities (P = 0.01) as well as negative effects on education (P = 0.02), sleep (P = 0.001), relationships (P = 0.001) and annual income (P = 0.01). The prevalence of OAB in Iranian women is higher than that reported in many previous studies in developed and developing countries. Our results reveal that OAB is a highly prevalent condition among Iranian women and that is has a serious impact on quality of life and sexual function.



Similar content being viewed by others
References
Abrams P, Cardozo L, Fall M, Griffiths D et al (2002) Standardisation sub-committee of the International Continence Society. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn 21:167–178. doi:10.1002/nau.10052
Ian Milsom I, Irwin DE (2007) A cross-sectional, population-based, multinational study of the prevalence of overactive bladder and lower urinary tract symptoms: results from the EPIC study. Eur Urol Suppl 6:4–9. doi:10.1016/j.eursup. 2006.10.003
Teloken C, Caraver F, Weber FA et al (2006) Overactive bladder: prevalence and implications in Brazil. Eur Urol 49:1087–1092. doi:10.1016/j.eururo.2006.01.026
Temml C, Heidler S, Ponholzer A et al (2005) Prevalence of the overactive bladder syndrome by applying the International Continence Society definition. Eur Urol 48:622–627. doi:10.1016/j.eururo.2005.04.026
Milsom I, Abrams P, Cardozo L et al (2001) How widespread are the symptoms of an overactive bladder and how are they managed? A population-based prevalence study. BJU Int 87:760–766. doi:10.1046/j.1464-410x.2001.02228.x
Lapitan MC, Asia-Pacific Chye PL, Board Continence Advisory (2001) The epidemiology of overactive bladder among females in Asia: a questionnaire survey. Int Urogynecol J Pelvic Floor Dysfunct 12:226–231. doi:10.1007/s001920170043
Stewart WF, Van Rooyen JB, Cundiff GW et al (2003) Prevalence and burden of overactive bladder in the United States. World J Urol 20:327–336
Irwin DE, Milsom I, Hunskaar S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50:1306–1315. doi:10.1016/j.eururo.2006.09.019
Wein AJ (2000) Overactive bladder: defining the disease. Am J Manag Care 6:559–564
Hu TW, Wagner TH (2005) Health-related consequences of overactive bladder: an economic perspective. BJU Int 96[Suppl 1]:43–45. doi:10.1111/j.1464-410X.2005.05654.x
Laumann EO, Gagnon JH, Michael RT et al (1994) The social organization of sexuality: sexual practices in the United States. University of Chicago Press, Chicago
Jackson S, Donovan J, Brookes S et al (1996) The Bristol female lower urinary tract symptoms questionnaire: development and psychometric testing. Br J Urol 77:805–812
Teleman PM, Lidfeldt J, Nerbrand C et al (2004) WHILA study group. Overactive bladder: prevalence, risk factors and relation to stress incontinence in middle-aged women. Br J Obstet Gynaecol 111:600–604. doi:10.1111/j.1471-0528.2004.00137.x
Swithinbank LV, Donovan JL, du Heaume JC et al (1999) Urinary symptoms and incontinence in women: relationships between occurrence, age, and perceived impact. Br J Gen Pract 49:897–900
Chen GD, Lin TL, Hu SW et al (2003) Prevalence and correlation of urinary incontinence and overactive bladder in Taiwanese women. Neurourol Urodyn 22:109–117. doi:10.1002/nau.10010
Acknowledgments
Many physicians, coordinators, project managers, secretaries and data reviewers assisted in this study. The author appreciates their cooperation. The author also thanks the numerous colleagues in the different counties of Iran who participated voluntarily in the collection of data: the collection of data was only possible by the wholehearted collaboration of the 86 general practitioners. Many thanks for the nationwide financial support and administrative help of Iranian people. We used “Humanity Help” (donation without consideration) as funding source in each city and counties, which was provided by different people. Certainly, without this financial support, the realization of this study would never have been possible. Nayyer Shafiei reviewed the medical records, and Saba Safarinejad assisted in the preparation of the manuscript. The interpretation and reporting of these data are the responsibility of the author and in no way should be seen as an official policy or interpretation of the Iranian Government.
Author information
Authors and Affiliations
Corresponding author
Additional information
Mohammad Reza Safarinejad, Vice-Chancellor for Education and Research, Urology and Nephrology Research Center, Associate Professor of Urology, Director Department of Urology, Associate Editor of Urology Journal.
Appendix A
Appendix A
Answers in bold for the following five questions qualified as OAB:
-
1.
How often do you have urgency?
-
Always (all of the time)
-
Frequently (more than two-thirds of the time)
-
Occasionally (between one-third and two-thirds of the time)
-
Rarely (less than one-third of the time)
-
Never
-
-
2.
How often do you have frequency?
-
Every 4 hours or less frequently
-
Every 3 hours
-
Every 2 hours
-
Hourly
-
-
3.
How many times do you have nocturia?
-
Four or more times
-
Three times
-
Twice
-
Once
-
None
-
-
4.
How often do you have urge incontinence?
-
Permanent
-
Several times a day
-
Once a day
-
Two to three times per week
-
Once a week or less frequent
-
Never
-
-
5.
How often do you have stress incontinence?
-
Permanent
-
Several times a day
-
Once a day
-
Two to three times per week
-
Once a week or less frequent
-
Never
-
Impact of OAB on quality of life and sexual function was assessed by the following two questions:
-
1.
In general, how much is your quality of life affected by your voiding problems?
-
Severely
-
Moderately
-
A little
-
Not at all
-
-
2.
In general, how much is your sexual life affected by your voiding problems?
-
Severely
-
Moderately
-
A little
-
Not at all
-
The following question was asked for determining coping strategies:
How was your urinary symptoms treated?
A. Self-care strategies
-
Modifying fluid intake
-
Regular schedule for urination
-
Always knowing the location of the bathrooms
-
Use of absorbent products
-
Physiotherapy or pelvic floor exercises
-
Limiting travel
-
Defensive voiding
B. Pharmacological treatment
QAB was subdivided into dry OAB and wet OAB cases based on the urinary incontinence question.
A respondent was defined as having OAB experiencing at least one of the following symptom groups:
Dry OAB:
-
1.
Urgency + frequency
-
2.
Urgency + nocturia
-
3.
Urgency + nocturia + frequency
Wet OAB:
The subjects were categorized as having wet OAB, if they had at least the combination of urgency and urge or mixed incontinence.
Rights and permissions
About this article
Cite this article
Safarinejad, M.R. Prevalence of the overactive bladder among Iranian women based on the International Continence Society definition: a population-based study. Int Urol Nephrol 41, 35–45 (2009). https://doi.org/10.1007/s11255-008-9403-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-008-9403-2