Abstract
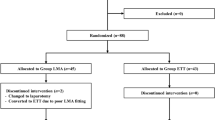
Elderly patients undergoing urological surgery in the lithotomy position may be vulnerable to perioperative hypoxemia. Positive end-expiratory pressure (PEEP) can improve arterial oxygenation. Although laryngeal mask airway (LMA) is widely utilized in urological surgery, it is not known how PEEP affects arterial oxygenation in these patients. We, therefore, evaluated the effect of PEEP on arterial oxygen partial pressure (PaO2) in elderly patients using LMA during urological surgery in the lithotomy position. Patients randomly received zero end-expiratory pressure (group Z, n = 34) or PEEP of 7 cmH2O (group P, n = 33). Ventilatory, respiratory, and haemodynamic variables were measured at 5 min (T0), 30 min (T1), and 60 min (T2) after LMA Supreme™ (sLMA) insertion. The primary outcome was the difference of PaO2 at T2 between the two groups. Atelectasis score, the incidence of a significant leak, and complications associated with sLMA insertion were also evaluated. PaO2 at T2 was significantly higher in group P than in group Z (20.0 ± 4.9 vs. 14.7 ± 3.7 kPa, P < 0.001). Atelectasis score at T2 was lower in group P than in group Z (5.3 ± 1.7 vs. 8.4 ± 2.3, P < 0.001). However, the incidence of a significant leak and complications associated with LMA insertion did not significantly differ between the two groups. PEEP can improve arterial oxygenation and reduce atelectasis in elderly patients using sLMA during urological surgery in the lithotomy position, suggesting that PEEP may be useful for elderly patients with an increased risk of perioperative hypoxemia when using sLMA.



Similar content being viewed by others
References
Froehner M, Brausi MA, Herr HW, Muto G, Studer UE. Complications following radical cystectomy for bladder cancer in the elderly. Eur Urol. 2009;56(3):443–54.
Güldner A, Kiss T, Neto AS, Hemmes SN, Canet J, Spieth PM, et al. Intraoperative protective mechanical ventilation for prevention of postoperative pulmonary complicationsa comprehensive review of the role of tidal volume, positive end-expiratory pressure, and lung recruitment maneuvers. Anesthesiology. 2015;123(3):692–713.
Navajas D, Farre R, Rotger MM, Milic-Emili J, Sanchis J. Effect of body posture on respiratory impedance. J Appl Physiol (1985). 1988;64(1):194–9.
Butterworth JF, Mackey DC, Wasnick JD. Morgan and Mikhail’s clinical anesthesiology. New York: McGraw-Hill Education; 2013. p.P 673–4.
Ball L, Pelosi P. Intraoperative ventilation and postoperative respiratory assistance. BJA Educ. 2017;17(11):357–62.
Wetterslev J, Hansen E, Roikjaer O, Kanstrup I, Heslet L. Optimizing peroperative compliance with PEEP during upper abdominal surgery: effects on perioperative oxygenation and complications in patients without preoperative cardiopulmonary dysfunction. Eur J Anaesthesiol. 2001;18(6):358–65.
Fredman B, Sheffer O, Zohar E, Paruta I, Richter S, Jedeikin R, et al. Fast-track eligibility of geriatric patients undergoing short urologic surgery procedures. Anesth Analg. 2002;94(3):560–4. table of contents.
Gong Y-H, Yi J, Zhang Q, Xu L. Effect of low dose rocuronium in preventing ventilation leak for flexible laryngeal mask airway during radical mastectomy. Int J Clin Exp Med. 2015;8(8):13616–21.
Futier E, Constantin J-M, Petit A, Jung B, Kwiatkowski F, Duclos M, et al. Positive end-expiratory pressure improves end-expiratory lung volume but not oxygenation after induction of anaesthesia. Eur J Anaesthesiol. 2010;27(6):508–13.
Habre W, Peták F. Perioperative use of oxygen: variabilities across age. Br J Anaesth. 2014;113(Suppl 2(suppl_2):ii26–36.
Zhao X, Huang S, Wang Z, Chen L, Li S. Relationship between respiratory dynamics and body mass index in patients undergoing general anesthesia with laryngeal mask airway (LMA) and comparison between lithotomy and supine positions. medical science monitor. Int Med J Exp Clin Res. 2016;22:2706–13.
SupremeTM TL. Instruction manual. Maidenhead: Intavent Orthofix Ltd; 2007.
Teoh W, Lee K, Suhitharan T, Yahaya Z, Teo M, Sia A. Comparison of the LMA Supreme vs the i-gel™ in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia. 2010;65(12):1173–9.
Bergmann I, Crozier TA, Roessler M, Schotola H, Mansur A, Büttner B, et al. The effect of changing the sequence of cuff inflation and device fixation with the LMA-Supreme® on device position, ventilatory complications, and airway morbidity: a clinical and fiberscopic study. BMC Anesthesiol. 2014;14(1):2.
Cook T, Gatward J, Handel J, Hardy R, Thompson C, Srivastava R, et al. Evaluation of the LMA Supreme™ in 100 non-paralysed patients. Anaesthesia. 2009;64(5):555–62.
Futier E, Constantin JM, Paugam-Burtz C, Pascal J, Eurin M, Neuschwander A, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–37.
Monastesse A, Girard F, Massicotte N, Chartrand-Lefebvre C, Girard M. Lung ultrasonography for the assessment of perioperative atelectasis: a pilot feasibility study. Anesth Analg. 2017;124(2):494–504.
Kim YB, Chang YJ, Jung WS, Byen SH, Jo YY. Application of PEEP using the i-gel during volume-controlled ventilation in anesthetized, paralyzed patients. J Anesth. 2013;27(6):827–31.
Latorre F, Eberle B, Weiler N, Mienert R, Stanek A, Goedecke R, et al. Laryngeal mask airway position and the risk of gastric insufflation. Anesth Analg. 1998;86(4):867–71.
Weiler N, Latorre F, Eberle B, Goedecke R, Heinrichs W. Respiratory mechanics, gastric insufflation pressure, and air leakage of the laryngeal mask airway. Anesth Analg. 1997;84(5):1025–8.
Von Goedecke A, Brimacombe J, Keller C, Hoermann C. Positive pressure versus pressure support ventilation at different levels of PEEP using the proseal (TM) laryngeal mask airway. Anaesth Intensive Care. 2004;32(6):804.
Bouvet L, Miquel A, Chassard D, Boselli E, Allaouchiche B, Benhamou D. Could a single standardized ultrasonographic measurement of antral area be of interest for assessing gastric contents? A preliminary report. Eur J Anaesthesiol. 2009;26(12):1015–9.
Bouvet L, Albert M-L, Augris C, Boselli E, Ecochard R, Rabilloud M, et al. Real-time detection of gastric insufflation related to facemask pressure–controlled ventilation using ultrasonography of the antrum and epigastric auscultation in nonparalyzed patientsa prospective, randomized, double-blind study. Anesthesiology. 2014;120(2):326–34.
Guimaraes MM, El Dib R, Smith AF, et al. Incentive spirometry for prevention of postoperative pulmonary complications in upper abdominal surgery. Cochrane Database Syst Rev. 2009;3:CD006058.
Hosten T, Gurkan Y, Ozdamar D, Tekin M, Toker K, Solak M. A new supraglottic airway device: LMA-Supreme™, comparison with LMA-Proseal™. Acta Anaesthesiol Scand. 2009;53(7):852–7.
Smetana GW, Lawrence VA, Cornell JE. Preoperative pulmonary risk stratification for noncardiothoracic surgery: systematic review for the American College of Physicians. Ann Intern Med. 2006;144(8):581–95.
Tran D, Rajwani K, Berlin DA. Pulmonary effects of aging. Curr Opin Anesthesiol. 2018;31(1):19–23.
Coppola S, Froio S, Chiumello D. Protective lung ventilation during general anesthesia: is there any evidence? Crit Care. 2014;18(2):210.
Redfors B, Bragadottir G, Sellgren J, Swärd K, Ricksten S-E. Acute renal failure is NOT an “acute renal success”—a clinical study on the renal oxygen supply/demand relationship in acute kidney injury. Crit Care Med. 2010;38(8):1695–701.
Ni C, Xu T, Li N, Tian Y, Han Y, Xue Q, et al. Cerebral oxygen saturation after multiple perioperative influential factors predicts the occurrence of postoperative cognitive dysfunction. BMC Anesthesiol. 2015;15(1):156.
Devereaux P, Goldman L, Cook DJ, Gilbert K, Leslie K, Guyatt GH. Perioperative cardiac events in patients undergoing noncardiac surgery: a review of the magnitude of the problem, the pathophysiology of the events and methods to estimate and communicate risk. CMAJ. 2005;173(6):627–34.
Extermann M, Overcash J, Lyman GH, Parr J, Balducci L. Comorbidity and functional status are independent in older cancer patients. J Clin Oncol. 1998;16(4):1582–7.
Daizoh Satoh S, Kurosawa W, Kirino T, Wagatsuma Y, Ejima A, Yoshida, et al. Impact of changes of positive end-expiratory pressure on functional residual capacity at low tidal volume ventilation during general anesthesia. J Anesth. 2012;26(5):664–9.
Spadaro S, Karbing DS, Mauri T, Marangoni E, Mojoli F, Valpiani G, et al. Effect of positive end-expiratory pressure on pulmonary shunt and dynamic compliance during abdominal surgery. Br J Anaesth. 2016;116(6):855–61.
Vargas M, Sutherasan Y, Gregoretti C, Pelosi P. PEEP role in ICU and operating room: from pathophysiology to clinical practice. Sci World J. 2014;2014:852356.
Goldmann K, Gerlach M, Bornträger C. ProSeal™ laryngeal mask in normal weight and obese patients: oxygenation under pressure-controlled ventilation and different end-expiratory pressures. Anaesthesist. 2011;60(10):908–15.
Goldmann K, Roettger C, Wulf H. Use of the ProSeal™ laryngeal mask airway for pressure-controlled ventilation with and without positive end-expiratory pressure in paediatric patients: a randomized, controlled study. Br J Anaesth. 2005;95(6):831–4.
Tusman G, Böhm SH, Tempra A, Melkun F, García E, Turchetto E, et al. Effects of recruitment maneuver on atelectasis in anesthetized children. Anesthesiology. 2003;98(1):14–22.
Eichenberger A-S, Proietti S, Wicky S, Frascarolo P, Suter M, Spahn D, et al. Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg. 2002;95(6):1788–92.
Iizuka T, Ishii N. The efficacy of the laryngeal mask airway during positive-pressure ventilation under general anesthesia. Anesth Analg. 1997;84:S240.
Acosta CM, Maidana GA, Jacovitti D, Belaunzarán A, Cereceda S, Rae E, et al. Accuracy of transthoracic lung ultrasound for diagnosing anesthesia-induced atelectasis in children. Anesthesiology. 2014;120(6):1370–9.
Xirouchaki N, Magkanas E, Vaporidi K, Kondili E, Plataki M, Patrianakos A, et al. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med. 2011;37(9):1488–93.
Hess DR. Respiratory mechanics in mechanically ventilated patients. Respir Care. 2014;59(11):1773–94.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Research Involving Human Participants and/or Animals
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kim, DH., Park, JY., Yu, J. et al. Positive end-expiratory pressure increases arterial oxygenation in elderly patients undergoing urological surgery using laryngeal mask airway in lithotomy position. J Clin Monit Comput 34, 161–169 (2020). https://doi.org/10.1007/s10877-019-00281-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-019-00281-4