Abstract
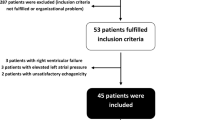
Predicting fluid responsiveness is crucial for adequate fluid management. Respiratory variations in pulse oximetry plethysmographic waveform amplitude (ΔPOP) are used to predict fluid responsiveness, but show inconsistent results when used for children. Contacting force between the measurement site and sensor can affect the ΔPOP value, thereby hindering its reliability as an indicator. We studied the influence of contacting force on the efficacy of ΔPOP as a fluid responsiveness indicator in children. In total, 43 mechanically ventilated children aged 1 month–5 years were studied. After anesthetic induction, mechanical ventilation began with a tidal volume of 10 ml/kg. ΔPOP was calculated for five different contacting force groups (0–0.3N, 0.3–0.6N, 0.6–0.9N, 0.9–1.2N, and 1.2–1.5N) and individually adjusted contacting force. Pulse pressure variation (PPV), and ΔVpeak were recorded before and after volume expansion. Subjects were considered as fluid responders if volume expansion increased the stroke volume index (SVI) by > 15%. Data from 38 patients were finally analyzed. A significant difference between the responders and non-responders was found only in ΔPOPs at 0.9–1.2N contacting force (P = 0.002) and individually adjusted contacting force (P < 0.000), while other contacting force groups did not show significant differences. ΔVpeak predicted a 15% increase in SVI (P = 0.008), whereas PPV did not. The ability of ΔPOP to predict fluid responsiveness depends on the contacting force in mechanically ventilated children. When contacting force is controlled to an adequate degree, the ability of ΔPOP to predict fluid responsiveness can be improved.



Similar content being viewed by others
References
Wakeling HG, McFall MR, Jenkins CS, Woods WG, Miles WF, Barclay GR, Fleming SC. Intraoperative oesophageal Doppler guided fluid management shortens postoperative hospital stay after major bowel surgery. Br J Anaesth. 2005;95(5):634–42. https://doi.org/10.1093/bja/aei223.
Gan TJ, Soppitt A, Maroof M, el-Moalem H, Robertson KM, Moretti E, Dwane P, Glass PS. Goal-directed intraoperative fluid administration reduces length of hospital stay after major surgery. Anesthesiology. 2002;97(4):820–6.
Poeze M, Greve JW, Ramsay G. Meta-analysis of hemodynamic optimization: relationship to methodological quality. Crit Care (London England). 2005;9(6):R771–9. https://doi.org/10.1186/cc3902.
Tavernier B, Makhotine O, Lebuffe G, Dupont J, Scherpereel P. Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology. 1998;89(6):1313–21.
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121(6):2000–8.
Cannesson M, Attof Y, Rosamel P, Desebbe O, Joseph P, Metton O, Bastien O, Lehot JJ. Respiratory variations in pulse oximetry plethysmographic waveform amplitude to predict fluid responsiveness in the operating room. Anesthesiology. 2007;106(6):1105–11. https://doi.org/10.1097/01.anes.0000267593.72744.20.
Feissel M, Michard F, Mangin I, Ruyer O, Faller JP, Teboul JL. Respiratory changes in aortic blood velocity as an indicator of fluid responsiveness in ventilated patients with septic shock. Chest. 2001;119(3):867–73.
Berkenstadt H, Margalit N, Hadani M, Friedman Z, Segal E, Villa Y, Perel A. Stroke volume variation as a predictor of fluid responsiveness in patients undergoing brain surgery. Anesth Analg. 2001;92(4):984–9.
Wiesenack C, Fiegl C, Keyser A, Prasser C, Keyl C. Assessment of fluid responsiveness in mechanically ventilated cardiac surgical patients. Eur J Anaesthesiol. 2005;22(9):658–65.
Feissel M, Michard F, Faller JP, Teboul JL. The respiratory variation in inferior vena cava diameter as a guide to fluid therapy. Intensive Care Med. 2004;30(9):1834–7. https://doi.org/10.1007/s00134-004-2233-5.
Natalini G, Rosano A, Taranto M, Faggian B, Vittorielli E, Bernardini A. Arterial versus plethysmographic dynamic indices to test responsiveness for testing fluid administration in hypotensive patients: a clinical trial. Anesth Analg. 2006;103(6):1478–84. https://doi.org/10.1213/01.ane.0000246811.88524.75.
Bendjelid K. The pulse oximetry plethysmographic curve revisited. Curr Opin Crit Care. 2008;14(3):348–53.
Cannesson M, Desebbe O, Rosamel P, Delannoy B, Robin J, Bastien O, Lehot JJ. Pleth variability index to monitor the respiratory variations in the pulse oximeter plethysmographic waveform amplitude and predict fluid responsiveness in the operating theatre. Br J Anaesth. 2008;101(2):200–6. https://doi.org/10.1093/bja/aen133.
Pereira de Souza Neto E, Grousson S, Duflo F, Ducreux C, Joly H, Convert J, Mottolese C, Dailler F, Cannesson M. Predicting fluid responsiveness in mechanically ventilated children under general anaesthesia using dynamic parameters and transthoracic echocardiography. Br J Anaesth. 2011;106(6):856–64. https://doi.org/10.1093/bja/aer090.
Renner J, Broch O, Gruenewald M, Scheewe J, Francksen H, Jung O, Steinfath M, Bein B. Non-invasive prediction of fluid responsiveness in infants using pleth variability index. Anaesthesia. 2011;66(7):582–9. https://doi.org/10.1111/j.1365-2044.2011.06715.x.
Byon HJ, Lim CW, Lee JH, Park YH, Kim HS, Kim CS, Kim JT. Prediction of fluid responsiveness in mechanically ventilated children undergoing neurosurgery. Br J Anaesth. 2013;110(4):586–91. https://doi.org/10.1093/bja/aes467.
Allen J, Murray A. Age-related changes in the characteristics of the photoplethysmographic pulse shape at various body sites. Physiol Meas. 2003;24(2):297–307.
Bergmann I, Gohner A, Crozier TA, Hesjedal B, Wiese CH, Popov AF, Bauer M, Hinz JM. Surgical pleth index-guided remifentanil administration reduces remifentanil and propofol consumption and shortens recovery times in outpatient anaesthesia. Br J Anaesth. 2013;110(4):622–8. https://doi.org/10.1093/bja/aes426.
Hickey M, Phillips JP, Kyriacou PA. The effect of vascular changes on the photoplethysmographic signal at different hand elevations. Physiol Meas. 2015;36(3):425–40. https://doi.org/10.1088/0967-3334/36/3/425.
Hickey M, Phillips JP, Kyriacou PA. Investigation of peripheral photoplethysmographic morphology changes induced during a hand-elevation study. J Clin Monit Comput. 2016;30(5):727–36. https://doi.org/10.1007/s10877-015-9761-0.
Teng XF, Zhang YT. The effect of contacting force on photoplethysmographic signals. Physiol Meas. 2004;25(5):1323–35.
Gaies MG, Gurney JG, Yen AH, Napoli ML, Gajarski RJ, Ohye RG, Charpie JR, Hirsch JC Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 2010;11(2):234–238. https://doi.org/10.1097/PCC.0b013e3181b806fc.
Hajian-Tilaki K. Sample size estimation in diagnostic test studies of biomedical informatics. J Biomed Inform. 2014;48:193–204. https://doi.org/10.1016/j.jbi.2014.02.013.
Cannesson M, Le Manach Y, Hofer CK, Goarin JP, Lehot J-J, Vallet B, Tavernier B. Assessing the diagnostic accuracy of pulse pressure variations for the prediction of fluid responsiveness a “Gray Zone” approach. Anesthesiology. 2011;115(2):231–41.
Reisner A, Shaltis PA, McCombie D, Asada HH. Utility of the photoplethysmogram in circulatory monitoring. J Am Soc Anesthesiol. 2008;108(5):950–8.
Broch O, Bein B, Gruenewald M, Höcker J, Schöttler J, Meybohm P, Steinfath M, Renner J. Accuracy of the pleth variability index to predict fluid responsiveness depends on the perfusion index. Acta Anaesthesiol Scand. 2011;55(6):686–93.
Marik PE. Hemodynamic parameters to guide fluid therapy. Transfus Altern Transfus Med. 2010;11(3):102–12.
Lee JH, Song IK, Kim EH, Kim HS, Kim JT. Prediction of fluid responsiveness based on liver compression-induced blood pressure changes in children after cardiac surgery. Minerva Anestesiol. 2017;83(9):939–46. https://doi.org/10.23736/s0375-9393.17.11544-0.
Acknowledgements
This study was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF), funded by the Korean government (MSIP & MOHW) (No. 2016M3A9F1939646).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Park, J., Yang, S., Lee, JH. et al. The importance of sensor contacting force for predicting fluid responsiveness in children using respiratory variations in pulse oximetry plethysmographic waveform. J Clin Monit Comput 33, 393–401 (2019). https://doi.org/10.1007/s10877-018-0183-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0183-7