Abstract
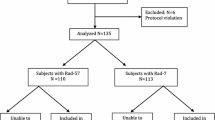
Early detection of hemorrhagic shock is required to facilitate prompt coordination of blood component therapy delivery to the bedside and to expedite performance of lifesaving interventions. Standard physical findings and vital signs are difficult to measure during the acute resuscitation stage, and these measures are often inaccurate until patients deteriorate to a state of decompensated shock. The aim of this study is to examine a severely injured trauma patient population to determine whether a noninvasive SpHb monitor can predict the need for urgent blood transfusion (universal donor or additional urgent blood transfusion) during the first 12 h of trauma patient resuscitation. We hypothesize that trends in continuous SpHb, combined with easily derived patient-specific factors, can identify the immediate need for transfusion in trauma patients. Subjects were enrolled if directly admitted to the trauma center, >17 years of age, and with a shock index (heart rate/systolic blood pressure) >0.62. Upon admission, a Masimo Radical-7 co-oximeter sensor (Masimo Corporation, Irvine, CA) was applied, providing measurement of continuous non-invasive hemoglobin (SpHb) levels. Blood was drawn and hemoglobin concentration analyzed and conventional pulse oximetry photopletysmograph signals were continuously recorded. Demographic information and both prehospital and admission vital signs were collected. The primary outcome was transfusion of at least one unit of packed red blood cells within 24 h of admission. Eight regression models (C1–C8) were evaluated for the prediction of blood use by comparing area under receiver operating curve (AUROC) at different time intervals after admission. 711 subjects had continuous vital signs waveforms available, to include heart rate (HR), SpHb and SpO2 trends. When SpHb was monitored for 15 min, SpHb did not increase AUROC for prediction of transfusion. The highest ROC was recorded for model C8 (age, sex, prehospital shock index, admission HR, SpHb and SpO2) for the prediction of blood products within the first 3 h of admission. When data from 15 min of continuous monitoring were analyzed, significant improvement in AUROC occurred as more variables were added to the model; however, the addition of SpHb to any of the models did not improve AUROC significantly for prediction of blood use within the first 3 h of admission in comparison to analysis of conventional oximetry features. The results demonstrate that SpHb monitoring, accompanied by continuous vital signs data and adjusted for age and sex, has good accuracy for the prediction of need for transfusion; however, as an independent variable, SpHb did not enhance predictive models in comparison to use of features extracted from conventional pulse oximetry. Nor was shock index better than conventional oximetry at discriminating hemorrhaging and prediction of casualties receiving blood. In this population of trauma patients, noninvasive SpHb monitoring, including both trends and absolute values, did not enhance the ability to predict the need for blood transfusion.



Similar content being viewed by others
References
World Health Organization. Injuries and violence: the facts. Geneva, World Health Organization, 2010.
Corso P, Finkelstein E, Miller T, Flebelkorn I, Zaloshnja E. Incidence and lifetime costs of injuries in the United States. Inj Prev. 2006;12:212–8.
Holcomb J. Optimal use of blood products in severely injured trauma patients. Hematol Am Soc Hematol Educ Prog. 2010;2010:465–9. doi:10.1182/asheducation-2010.1.465.
Allen J. Photoplethysmography and its application in clinical physiological assessment. Physiol Meas. 2007;28:R1–39.
Deaths and Mortality. Centers for disease control and prevention, 2010. http://www.cdc.gov/nchs/fastats/deaths.htm. Accessed 6 Feb 2014.
Guyette F, Gomez H, Suffoletto B, et al. Preshospital dynamic tissue saturation response predicts in-hospital lifesaving interventions in trauma patients. J Trauma Acute Care Surg. 2012;72:930–5.
McGee S, Abernethy WI, Simel D. The rational clinical examination: is this patient hypovolemic. JAMA. 1999;281:1022–9.
Gehring H, Hornberger C, Dibbelt L, et al. Accuracy of point-of-care-testing (POCT) for determining hemoglobin concentration. Acta Anaesthesiol Scand. 2002;46:980–6.
Kim SH, Lilot M, Murphy LSK, et al. Accuracy of continuous noninvasive hemoglobin monitoring: a systematic review and meta-analysis. Anesth Analg. 2014;119:332–46.
Patino M, Schultz L, Hossain M, Moeller J, Mahmoud M, Gunter J, Kurth CD. Trending and accuracy of noninvasive hemoglobin monitoring in pediatric perioperative patients. Anesth Analg. 2014;119(4):920–5.
de Biasi A, Stansbury L, Dutton R, Stein D, Scalea T, Hess JR. Blood product use in trauma resuscitation: plasma deficitversus plasma ratio as predictors of mortality in trauma. Transfusion. 2011;51:1925–32.
Mackenzie CF, Gao C, Hu PF, Anazodo A, Chen H, Dinardo T, Imle PC, Hartsky L, Stephens C, Menaker J, Fouche Y, Murdock K, Galvagno S, Alcorta R, Shackelford S, ONPOINT Study Group. Comparison of decision-assist and clinical judgment of experts for prediction of life saving interventions. Shock. 2014. doi:10.1097/SHK.0000000000000288.
Como J, Dutton R, Scalea T, Edeleman B, Hess J. Blood transfusion rates in the care of acute trauma. Transfusion. 2004;44:809–13.
Shackelford SA, Colton K, Stansbury LG, Galvagno SM Jr, Anazodo AN, DuBose JJ, Hess JR, Mackenzie CF. Early identification of uncontrolled hemorrhage after trauma: current status and future direction. J Trauma Acute Care Surg. 2014;77(3 Suppl 2):S222–7.
Vandromme M, Griffin R, Kerby J, McGwin G, Rue L, Weinberg J. Identifying risk for massive transfusion in the relatively normotensive patient: utility of the prehospital shock index. J Trauma Acute Care Surg. 2011;70:384–8.
DeLong E, DeLong D, Clarke-Pearson D. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44:837–45.
Stone M. Cross-validatory choice and assessment of statistical predictions (with discussion). J R Stat Soc B. 1974;36:111–47.
Mackenzie C, Wang Y, Hu P, et al. Automated prediction of early blood transfusion and mortality in trauma patients. J Trauma Acute Care Surg. 2014;76:1379–85.
Ogura T, Nakamura Y, Nakano M, et al. Predicting the need for massive transfusion in trauma patients: the Traumatic Bleeding Severity Score. J Trauma Acute Care Surg. 2014;76:1243–50.
Acknowledgments
This work was funded by the Department of Defense (USAF 8650-11-6142). The views represent those of the authors not USAF or the Department of Defense. Masimo (Masimo Corporation, Irvine, CA) provided the SpHb monitors, but had no role in the design, execution, or analysis of this research.
Conflict of interest
Other than the abovementioned funding, none of the authors have any conflicts of interest to report.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Galvagno, S.M., Hu, P., Yang, S. et al. Accuracy of continuous noninvasive hemoglobin monitoring for the prediction of blood transfusions in trauma patients. J Clin Monit Comput 29, 815–821 (2015). https://doi.org/10.1007/s10877-015-9671-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-015-9671-1