Abstract
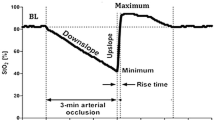
The aim of this study was to compare tissue oxygen saturation as measured by INVOS® and InSpectra™ during a vascular occlusion test (VOT) in the same subject. Twenty healthy adults were investigated. The INVOS® and InSpectra™ probes were placed randomly on the right and left thenar eminence in the same participant and monitoring of tissue oxygen saturation (SrO2 from INVOS® and StO2 from InSpectra™) were begun. Pneumatic cuffs placed around each upper arm were inflated simultaneously to 30 mmHg above the initial systolic blood pressure and maintained until the tissue oxygen saturation had decreased to 40 % or below. The cuff pressure was then released rapidly. The time to achieve initial stability, the baseline value, the time from the baseline value to 40 %, the rate of deoxygenation, the rate of reoxygenation, and the hyperemic area under the curve were calculated from SrO2 and StO2. The baseline value by INVOS® was lower than that by InSpectra™ (75.6 ± 8.2 vs. 81.8 ± 3.4 %, p < 0.01). The time to reach stable baseline value was significantly longer for SrO2 than for StO2 (249 ± 86 and 54 ± 40 s respectively; p < 0.01). SrO2 declined to 40 % more rapidly than did the StO2 (147 ± 38 vs. 199 ± 41 s, p < 0.01). The deoxygenation and reoxygenation rates were higher (p < 0.01) and the reactive hyperemic area was more extensive for INVOS® than for InSpectra™ (p = 0.015). In conclusion, the VOT on the thenar muscle using INVOS® was as clinically applicable as InSpectra™, but baseline values and dynamic changes of INVOS® differed from those of InSpectra™.




Similar content being viewed by others
References
Hanson SJ, Berens RJ, Havens PL, Kim MK, Hoffman GM. Effect of volume resuscitation on regional perfusion in dehydrated pediatric patients as measured by two-site near-infrared spectroscopy. Pediatr Emerg Care. 2009;25(3):150–3 Epub 2009/03/06.
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103(Suppl 1):i3–13 Epub 2009/12/17.
Mancini DM, Bolinger L, Li H, Kendrick K, Chance B, Wilson JR. Validation of near-infrared spectroscopy in humans. J Appl Physiol. 1994;77(6):2740–7 Epub 1994/12/01.
Scheeren TW, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26(4):279–87 Epub 2012/04/03.
Lipcsey M, Woinarski NC, Bellomo R. Near infrared spectroscopy (NIRS) of the thenar eminence in anesthesia and intensive care. Ann Intensive Care. 2012;2(1):11.
Boushel R, Piantadosi CA. Near-infrared spectroscopy for monitoring muscle oxygenation. Acta Physiol Scand. 2000;168(4):615–22 Epub 2000/04/12.
Creteur J. Muscle StO2 in critically ill patients. Curr Opin Crit Care. 2008;14(3):361–6 Epub 2008/05/10.
Creteur J, Carollo T, Soldati G, Buchele G, De Backer D, Vincent JL. The prognostic value of muscle StO2 in septic patients. Intensive Care Med. 2007;33(9):1549–56 Epub 2007/06/19.
Cohn SM, Nathens AB, Moore FA, et al. Tissue oxygen saturation predicts the development of organ dysfunction during traumatic shock resuscitation. J Trauma. 2007;62(1):44–54 discussion-5, Epub 2007/01/12.
Futier E, Christophe S, Robin E, et al. Use of near-infrared spectroscopy during a vascular occlusion test to assess the microcirculatory response during fluid challenge. Crit Care. 2011;15(5):R214.
Fellahi JL, Butin G, Zamparini G, Fischer MO, Gerard JL, Hanouz JL. Lower limb peripheral NIRS parameters during a vascular occlusion test: an experimental study in healthy volunteers. Ann Fr Anesth Reanim. 2014;33(1):27.
Fellahi JL, Butin G, Fischer MO, Zamparini G, Gerard JL, Hanouz JL. Dynamic evaluation of near-infrared peripheral oximetry in healthy volunteers: a comparison between INVOS and EQUANOX. J Crit Care. 2013;28(5):881 e1–6.
Bartels SA, Bezemer R, de Vries FJ, et al. Multi-site and multi-depth near-infrared spectroscopy in a model of simulated (central) hypovolemia: lower body negative pressure. Intensive Care Med. 2011;37(4):671–7.
Cohn SM, Pearl RG, Acosta SM, et al. A prospective randomized pilot study of near-infrared spectroscopy-directed restricted fluid therapy versus standard fluid therapy in patients undergoing elective colorectal surgery. Am Surg. 2010;76(12):1384–92.
Gomez H, Torres A, Polanco P, et al. Use of non-invasive NIRS during a vascular occlusion test to assess dynamic tissue O(2) saturation response. Intensive Care Med. 2008;34(9):1600–7 Epub 2008/06/05.
Lima A, van Bommel J, Sikorska K, et al. The relation of near-infrared spectroscopy with changes in peripheral circulation in critically ill patients. Crit Care Med. 2011;39(7):1649–54.
Lima A, van Bommel J, Jansen TC, Ince C, Bakker J. Low tissue oxygen saturation at the end of early goal-directed therapy is associated with worse outcome in critically ill patients. Crit Care. 2009;13(Suppl 5):S13.
Podbregar M, Mozina H. Skeletal muscle oxygen saturation does not estimate mixed venous oxygen saturation in patients with severe left heart failure and additional severe sepsis or septic shock. Crit Care. 2007;11(1):R6.
Mozina H, Podbregar M. Near-infrared spectroscopy during stagnant ischemia estimates central venous oxygen saturation and mixed venous oxygen saturation discrepancy in patients with severe left heart failure and additional sepsis/septic shock. Crit Care. 2010;14(2):R42.
Payen D, Luengo C, Heyer L, et al. Is thenar tissue hemoglobin oxygen saturation in septic shock related to macrohemodynamic variables and outcome? Crit Care. 2009;13(Suppl 5):S6.
Mayeur C, Campard S, Richard C, Teboul JL. Comparison of four different vascular occlusion tests for assessing reactive hyperemia using near-infrared spectroscopy. Crit Care Med. 2011;39(4):695–701.
De Blasi RA, Palmisani S, Alampi D, et al. Microvascular dysfunction and skeletal muscle oxygenation assessed by phase-modulation near-infrared spectroscopy in patients with septic shock. Intensive Care Med. 2005;31(12):1661–8.
Pareznik R, Knezevic R, Voga G, Podbregar M. Changes in muscle tissue oxygenation during stagnant ischemia in septic patients. Intensive Care Med. 2006;32(1):87–92.
Skarda DE, Mulier KE, Myers DE, Taylor JH, Beilman GJ. Dynamic near-infrared spectroscopy measurements in patients with severe sepsis. Shock. 2007;27(4):348–53.
Gomez H, Mesquida J, Simon P, et al. Characterization of tissue oxygen saturation and the vascular occlusion test: influence of measurement sites, probe sizes and deflation thresholds. Crit Care. 2009;13(Suppl 5):S3.
Bezemer R, Lima A, Myers D, et al. Assessment of tissue oxygen saturation during a vascular occlusion test using near-infrared spectroscopy: the role of probe spacing and measurement site studied in healthy volunteers. Crit Care. 2009;13(Suppl 5):S4.
Creteur J, Neves AP, Vincent JL. Near-infrared spectroscopy technique to evaluate the effects of red blood cell transfusion on tissue oxygenation. Crit Care. 2009;13(Suppl 5):S11.
Donati A, Romanelli M, Botticelli L, et al. Recombinant activated protein C treatment improves tissue perfusion and oxygenation in septic patients measured by near-infrared spectroscopy. Crit Care. 2009;13(Suppl 5):S12.
Lipcsey M, Eastwood GM, Woinarski NC, Bellomo R. Near-infrared spectroscopy of the thenar eminence: comparison of dynamic testing protocols. Crit Care Resusc. 2012;14(2):142–7 Epub 2012/06/16.
Hernandez G, Regueira T, Bruhn A, et al. Relationship of systemic, hepatosplanchnic, and microcirculatory perfusion parameters with 6-hour lactate clearance in hyperdynamic septic shock patients: an acute, clinical-physiological, pilot study. Ann Intensive Care. 2012;2(1):44.
Horvath R, Shore S, Schultz SE, Rosenkranz ER, Cousins M, Ricci M. Cerebral and somatic oxygen saturation decrease after delayed sternal closure in children after cardiac surgery. J Thorac Cardiovasc Surg. 2010;139(4):894–900 Epub 2009/08/08.
McNeill S, Gatenby JC, McElroy S, Engelhardt B. Normal cerebral, renal and abdominal regional oxygen saturations using near-infrared spectroscopy in preterm infants. J Perinatol. 2011;31(1):51–7 Epub 2010/06/12.
Muellner T, Nikolic A, Schramm W, Vecsei V. New instrument that uses near-infrared spectroscopy for the monitoring of human muscle oxygenation. J Trauma-Inj Infect Crit Care. 1999;46(6):1082–4.
Nygren A, Rennerfelt K, Zhang Q. Detection of changes in muscle oxygen saturation in the human leg: a comparison of two near-infrared spectroscopy devices. J Clin Monit Comput. 2014;28(1):57–62 Epub 2013/07/13.
Dix LM, van Bel F, Baerts W, Lemmers PM. Comparing near-infrared spectroscopy devices and their sensors for monitoring regional cerebral oxygen saturation in the neonate. Pediatr Res. 2013;74(5):557–63.
Lima A, Bakker J. Noninvasive monitoring of peripheral perfusion. Intensive Care Med. 2005;31(10):1316–26 Epub 2005/09/20.
Benaron DA, Kurth CD, Steven JM, Delivoria-Papadopoulos M, Chance B. Transcranial optical path length in infants by near-infrared phase-shift spectroscopy. J Clin Monit. 1995;11(2):109–17.
Duncan A, Meek JH, Clemence M, et al. Measurement of cranial optical path length as a function of age using phase resolved near infrared spectroscopy. Pediatr Res. 1996;39(5):889–94.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, JH., Park, YH., Kim, HS. et al. Comparison of two devices using near-infrared spectroscopy for the measurement of tissue oxygenation during a vascular occlusion test in healthy volunteers (INVOS® vs. InSpectra™). J Clin Monit Comput 29, 271–278 (2015). https://doi.org/10.1007/s10877-014-9595-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-014-9595-1