Abstract
Objective
Intravascular volume loading is used to optimize cardiac output in children following weaning from cardiopulmonary bypass. Central venous pressure (CVP) is frequently used to titrate fluid administration but it is often misleading in predicting fluid responsiveness. Variation in the arterial pressure waveform is exaggerated in patients with deficient intravascular volume and has been shown to be a good predictor of fluid responsiveness in adults following cardiac surgery. The aim of this study was to compare the measures of variation in blood pressure as a guide to volume loading in children following cardiopulmonary bypass.
Methods
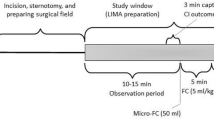
After ethical approval, we collected continuous real-time measurements from 25 children during volume loading after cardiopulmonary bypass. Subjects with moderate or severe tricuspid incompetence␣or␣who did not require volume loading during weaning from cardiopulmonary bypass were excluded from the study. Unstable readings were excluded from analysis. Systolic Pressure Variation (SPV), Pulse Pressure Variation (PPV) and Systolic Volume Variation (SVV) were retrospectively calculated before and after␣each bolus of fluid. Fluid responsiveness was classified as␣a␣change in blood pressure of ≥80 mmHg/L/m2.
Results
Forty-four boluses were analyzed from the 25 children. Respiratory variables were similar. CVP was a poor predictor of fluid responsiveness and a negative relationship between change in blood pressure and ΔDown was observed. Performance in predicting fluid responsiveness as measured by the areas under the ROC curves were CVP (0.58), PPV (0.67), SPV (0.74) and SVV (0.74).
Conclusions
Variation in blood pressure was a better guide to volume loading in children than CVP. Δdown was not useful in predicting fluid responsiveness in children with open chests following bypass surgery. SPV and SVV require further testing in prospective clinical trials.
Similar content being viewed by others
References
Pizov R, Segal E, Kaplan L, Floman Y, Perel A (1990). The use of systolic pressure variation in hemodynamic monitoring during deliberate hypotension in spine surgery. J Clin Anesth 2:96–100
Gunn S, Pinsky M (2001). Implications of arterial pressure variation in patients in the intensive care unit. Curr Opin Crit Care 7:212–217
Perel A (1998). Assessing fluid responsiveness by the systolic pressure variation in mechanically ventilated patients: Systolic pressure variation as a guide to fluid therapy in patients with sepsis-induced hypotension. Anesthesiology 89:1309–1310
Schwid H, Rooke A (2000). Systolic blood pressure at end-expiration measured by the automated systolic pressure variation monitor is equivalent to systolic blood pressure during apnea. J Clin Monit 16:115–120
Michard F, Chemla D, Richard C et al. (1999). Clinical use of respiratory changes in arterial pulse pressure to monitor the hemodynamic effects of PEEP. Am J Respir Crit Care Med 159:935–939
Reuter BDA, Felbinger TW, Schmidt C, Lamm P, Goetz AE (2002). Stroke volume variation for assessment of cardiac responsiveness to volume loading in mechanically ventilated patients after cardiac surgery. Intens Care Med 28: 192–198
Jacobson AL (2001) Auto-threshold peak detection in physiological signals. EMBS 3:2194–2195
Kleiber M (1961) The fire of life: An introduction to animal energetics. New York, Wiley
Bendjelid K, Romand J (2003). Fluid responsiveness in mechanically ventilated patients: a review of indices used in intensive care. Intens Care Med 29:352–360
Pinsky M, Desmet J, Vincent J (1992). Effect of positive end-expiratory pressure on right ventricular function in humans. Am Rev Respir Dis 146:681–687
Magder S (2004) Clinical usefulness of respiratory variations in arterial pressure. Am J Respir Crit Care Med 169:151–155
Michard F (2005) Changes in arterial pressure during mechanical ventilation. Anesthesiology 103:419–428
Szold A, Pizov R, Segal E, Perel A (1989). The effect of tidal volume and intravascular volume state on systolic pressure variation in ventilated dogs. Intens Care Med 15(6):368–371
Vedrinne J, Duperret S, Decaillot F, Gratadour P, Motin J (1997) Haemodynamic changes induced by two I:E ratios: a transoesophageal echocardiographic study. Can J Anesth 44: 354–359
Pizov R, Cohen M, Weiss Y, Segal E, Cotev S, Perel A (1996). Positive end-expiratory pressure-induced hemodynamic changes are reflected in the arterial pressure waveform. Crit Care Med 24(8):1381–1387
Reuter D, Kirchner A, Felbinger T, Weis F, Kilger E, Lamm P, Goetz A (2003). Usefulness of left ventricular stroke volume variation to assess fluid responsiveness in patients with reduced cardiac function. Crit Care Med 31(5):1399–1404
Acknowledgments
Presented in part at the Society for Technology in Anesthesia Meeting in 2006. HT supported by the Natural Sciences and␣Engineering Research Council of Canada and JMA by a Canadian Anesthesiologists’ Society Career Scientist Award. We would like to thank the faculty of the Department of Anesthesia at British Columbia Children’s Hospital and all the staff in the cardiac operating room for assistance with data collection. Thanks to Natasha McCartney for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Henry T, Froese N,Dumont G, Lim J, Ansermino JM. Variation in blood pressure as a guide to volume loading in children following cardiopulmonary bypass.
Rights and permissions
About this article
Cite this article
Tran, H., Froese, N., Dumont, G. et al. Variation in Blood Pressure as a Guide to Volume Loading in Children Following Cardiopulmonary Bypass. J Clin Monit Comput 21, 1–6 (2007). https://doi.org/10.1007/s10877-006-9051-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-006-9051-y