Abstract
Purpose
To investigate the effect of scleral-fixated intraocular lens (IOL) tilt on visual outcomes.
Methods
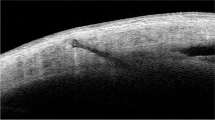
Ninety-four eyes of consecutive 94 patients who underwent scleral-fixated IOL implantation with Z-suture technique were included in this prospective study. The values of pre- and postoperative 12th month uncorrected visual acuity (UCVA), cylindrical refractive error, best-corrected visual acuity (BCVA) and corneal and lenticular astigmatism were recorded. The position of the implanted IOL was evaluated with anterior segment optical coherence tomography (AS-OCT). The relationships between the AS-OCT measurements and the visual acuity or refractive errors were investigated.
Results
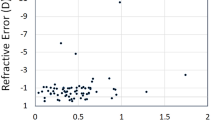
The IOL position was evaluated as tilted in 68 (72.3%) patients: 29 (30.8%) in both vertical + horizontal axes, 30 (31.9%) in the horizontal axis and 9 (9.6%) in the vertical axis. There were no significant differences between patients with and without tilt IOL position in terms of the UCVA, BCVA, cylindrical refractive error and lenticular astigmatism (p > 0.05, for each). The mean BCVA was significantly higher in the no-tilt group than in the both horizontal + vertical tilt and the vertical tilt groups (p = 0.03, p = 0.04, respectively). The mean lenticular astigmatism was significantly higher in the vertical tilt group than the other groups (p = 0.04).
Conclusion
Tilting in IOL position occurs commonly; however, IOLs with tilting on any of the axes do not have significantly worse outcomes when compared with IOLs with no tilt, in terms of visual results and refractive errors. On the other hand, tilting on the vertical axis is observed less commonly, yet is more effective on visual results and refractive errors, when compared with tilting on the horizontal axis.

Similar content being viewed by others
References
Theodore FH (1965) Complications after cataract surgery. Little, Brown&Co, Boston, pp 102–134
Steinert RF (1995) Cataract surgery: technique, complications and management. Saunders, Philadelphia, pp 270–313
Ercalik NY, Macin A, Cengiz O et al (2014) Comparison of results with secondary anterior chamber and secondary scleral fixated intraocular lens implantation in complicated phacoemulsification cases. Turk J Ophthalmol 44(2):102–107
Baykara M, Ertürk H, Avci R et al (2004) Intraocular lens implantation by scleral fixation. Turk J Ophthalmol 34(1):55–60
Leung CK, Li H, Weinreb RN et al (2008) Anterior chamber angle measurement with anterior segment optical coherence tomography: a comparison between slit lamp OCT and Visante OCT. Invest Ophthalmol Vis Sci 49(8):3469–3474
Li L, Wang K, Yan Y et al (2013) Research on calculation of the IOL tilt and decentration based on surface fitting. Comput Math Methods Med. https://doi.org/10.1155/2013/572530
Suto C, Hori S, Fukuyama E, Akura J (2003) Adjusting intraocular lens power for sulcus fixation. J Cataract Refract Surg 29(10):1913–1917
Dubey R, Birchall W, Grigg J (2012) Improved refractive outcome for ciliary sulcus-implanted intraocular lenses. Ophthalmology 119(2):261–265
Cavallini GM, Volante V, Maria M et al (2015) Long-term analysis of IOL stability of the Lewis technique for scleral fixation. Eur J Ophthalmol 25(6):525–528
Holladay JT, Cravy TV, Koch DD (1992) Calculating the surgically induced refractive change following ocular surgery. J Cataract Refract Surg 18(5):429–443
Holladay JT, Dudeja DR, Koch DD (1998) Evaluating and reporting astigmatism for individual and aggregate data. J Cataract Refract Surg 24(1):57–65
Loya N, Lichter H, Barash D et al (2001) Posterior chamber intra- ocular lens implantation after capsular tear: ultrasound bio- microscopy evaluation. J Cataract Refract Surg 27(9):1423–1427
Kumar DA, Agarwal A, Packialakshmi S et al (2013) In vivo analysis of glued intraocular lens position with ultrasound biomicroscopy. J Cataract Refract Surg 39(7):1017–1022
Yamane S, Inoue M, Arakawa A et al (2014) Sutureless 27-gauge needle–guided intrascleral intraocular lens implantation with lamellar scleral dissection. Ophthalmology 121(1):61–66
Kumar DA, Agarwal A, Agarval A et al (2015) Long-term assessment of tilt of glued intraocular lenses: an optical coherence tomography analysis 5 years after. Surg Ophthalmol 122(1):48–55
Kumar DA, Agarwal A, Prakash G et al (2011) Evaluation of intraocular lens tilt with anterior segment optical coherence tomography. Am J Ophthalmol 151(3):406–412
Akkin C, Ozler SA, Mentes J (1994) Tilt and decentration of bag-fixated intraocular lenses: a comparative study between capsulorrhexis and envelope techniques. Doc Ophthalmol 87(3):199–209
Hayashi K, Hayashi H, Nakao F et al (1999) Intraocular lens tilt and decentration, anterior chamber depth, and refractive error after trans-scleral suture fixation surgery. Ophthalmology 106(5):878–882
Durak I, Öner HF, Koçak N et al (2001) Tilt and decentration after primary and secondary transsclerally sutured posterior chamber intraocular lens implantation. J Cataract Refract Surg 27(2):227–232
Uozato H, Okada Y, Hirai H et al (1988) What are the tolerable limits of IOL tilt and decentration? Jpn Rev Clin Ophthalmol 82(1):2308–2311
Guyton DL, Uozato H, Wisnicki HJ (1990) Rapid determination of intraocular lens tilt and decentration through the undilated pupil. Ophthalmology 97(10):1259–1264
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors have no proprietary interest, and no financial support was received.
Electronic supplementary material
Below is the link to the electronic supplementary material.
10792_2019_1233_MOESM1_ESM.avi
Video-1: Scleral fixation surgery video with Z-suture technique applied to one of our patients. Firstly, dissection of conjunctiva and tenon and cauterization of superficial conjunctival vessels were performed. 10–0 polypropylene-looped suture with a long curved needle (PC-9; Alcon Surgical, Fort Worth, TX) was passed through the cartridge. The suture was tied to one of the haptics of the three-piece IOL. Anterior vitrectomy was performed before suturing the IOL, if vitreous prolapsus was present. The needle was passed through the ciliary sulcus, perforating the sclera at approximately 1.5 mm distance to the limbus. The IOL was injected into the anterior chamber using the cartridge, but the other haptic was not injected. The suture was tied to the other haptic, which was left outside. The needle was passed from the ciliary sulcus through the sclera about 1.5 mm to the limbus. The scleral fixation points were 180 degree diagonally apart (12–6 o’clock meridians). Then transscleral suturation was performed with the Z-suture technique. This patient has aphakic left eye due to complicated cataract surgery. The preoperative best-corrected visual acuity was 0.2. At postoperative 12th month, best-corrected visual acuity was 0.1 and IOL position was evaluated as ‘no tilt’ with anterior segment OCT (AVI 70,594 kb).
Rights and permissions
About this article
Cite this article
Kemer Atik, B., Altan, C., Agca, A. et al. The effect of intraocular lens tilt on visual outcomes in scleral-fixated intraocular lens implantation. Int Ophthalmol 40, 717–724 (2020). https://doi.org/10.1007/s10792-019-01233-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-019-01233-2