Abstract
Background
Limited data exist regarding the psychosocial aspects of gastroesophageal reflux disease (GERD). Some GERD subgroups, such as functional heartburn and hypersensitive esophagus, might show different psychiatric comorbidities than others.
Aim
We aimed to evaluate the psychiatric comorbidities of GERD subgroups using a cross-sectional design.
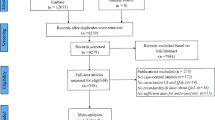
Methods
A group of GERD patients at a tertiary outpatient clinic were evaluated via upper GIS (gastrointestinal system) endoscopy, esophageal manometry, and 24-h impedance–pH monitoring. Thirty-nine patients diagnosed with erosive reflux disease, 44 with non-erosive reflux disease, 20 with functional heartburn, 11 with hypersensitive esophagus, and 44 healthy controls participated. Psychiatric diagnoses were made using the Structured Clinical Interview for Diagnostics and Statistical Manual of Mental Disorders IV. Psychometric measurements of the patients were performed using the Somatosensory Amplification Scale, Beck Depression Inventory, State-Trait Anxiety Inventory, and Short-Form 36. Healthy controls were evaluated with the same psychometric scales except for the Short-Form 36.
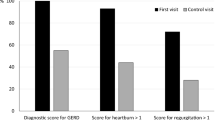
Results
All of the GERD subgroups were significantly more depressed than the control group. Depressive disorders were significantly more prevalent in the functional heartburn group than in the non-erosive reflux disease and erosive reflux disease groups. The trait anxiety level of the functional heartburn group was significantly higher than those of the control and non-erosive reflux disease groups. The quality of life scores of the GERD subgroups were significantly lower than the population standards.
Conclusions
Depressive disorders were frequently comorbid in the GERD subgroups studied (30–65 %). It is essential to consider the high prevalence rates of comorbid depression when managing GERD.


Similar content being viewed by others
References
Bor S, Mandiracioglu A, Kitapcioglu G, Caymaz-Bor C, Gilbert RJ. Gastroesophageal reflux disease in a low-income region in Turkey. Am J Gastroenterol. 2005;100:759–765.
Bor S, Lazebnik LB, Kitapcioglu G, Manannikof I, Vasiliev Y. Prevalence of gastroesophageal reflux disease in Moscow. Dis Esophagus. 2015;29:159–165.
Eslick GD, Talley NJ. Gastroesophageal reflux disease (GERD): risk factors, and impact on quality of life-a population-based study. J Clin Gastroenterol. 2009;43:111–117.
Boltin D, Boaz M, Aizic S, et al. Psychological distress is not associated with treatment failure in patients with gastroesophageal reflux disease. J Psychosom Res. 2013;75:462–466.
Granderath FA, Kamolz T. Pointner R Gastroesophageal Reflux Disease: Principles of Disease, Diagnosis, and Treatment. New York: Springer; 2006.
Wright CE, Ebrecht M, Mitchell R, Anggiansah A, Weinman J. The effect of psychological stress on symptom severity and perception in patients with gastro-oesophageal reflux. J Psychosom Res. 2005;59:415–424.
Naliboff BD, Mayer M, Fass R, et al. The effect of life stress on symptoms of heartburn. Psychosom Med. 2004;66:426–434.
Jansson C, Nordenstedt H, Wallander MA, et al. Severe gastro-oesophageal reflux symptoms in relation to anxiety, depression and coping in a population-based study. Aliment Pharmacol Ther. 2007;26:683–691.
Nunez-Rodriguez MH, Miranda Sivelo A. Psychological factors in gastroesophageal reflux disease measured by scl-90-R questionnaire. Dig Dis Sci. 2008;53:3071–3075.
Oh JH, Kim TS, Choi MG, et al. Relationship between psychological factors and quality of life in subtypes of gastroesophageal reflux disease. Gut Liver. 2009;3:259–265.
Rey E, Garcia-Alonso M, Moreno-Ortega M, Almansa C, Alvarez-Sanchez A, Diaz-Rubio M. Influence of psychological distress on characteristics of symptoms in patients with GERD: the role of IBS comorbidity. Dig Dis Sci. 2009;54:321–327.
Johnston B, Lewis S, Collins J, McFarland R, Love A. Acid perception in gastro-oesophageal reflux disease is dependent on psychosocial factors. Scand J Gastroenterol. 1995;30:1–5.
Shapiro M, Green C, Bautista JM, et al. Functional heartburn patients demonstrate traits of functional bowel disorder but lack a uniform increase of chemoreceptor sensitivity to acid. Am J Gastroenterol. 2006;101:1084–1091.
Wu JC, Cheung CM, Wong VW, Sung JJ. Distinct clinical characteristics between patients with nonerosive reflux disease and those with reflux esophagitis. Clin Gastroenterol Hepatol. 2007;5:690–695.
Tack J. Is there a unifying role for visceral hypersensitivity and irritable bowel syndrome in non-erosive reflux disease? Digestion. 2008;78:42–45.
Modlin IM, Hunt RH, Malfertheiner P, et al. Non-erosive reflux disease–defining the entity and delineating the management. Digestion. 2008;78:1–5.
First MBSR, Gibbon M, et al. Structured Clinical Interview for DSM IV Axis I Disorders (SCID I). Clinical Version. Washington, DC: American Psychiatric Press; 1997.
Ozkurkcugil A, Aydemir O, Yildiz M, EsenDanaci A, Koroglu E. Adaptation to Turkish and reliability study of Structured Clinical Interview for Axial I disorders. Ilac ve Tedavi Dergisi. 1999;12:233–236.
Beck AT. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571.
Hisli N. A study on the validity of Beck Depression Inventory. Turkish J Psychol. 1988;6:118–123.
Barsky AJ, Wyshak G, Klerman GL. The somatosensory amplification scale and its relationship to hypochondriasis. J Psychiatry Res. 1990;24:323–334.
Gulec H, Sayar K. Reliability and validity of the Turkish form of the Somatosensory Amplification Scale. Psychiatry Clin Neurosci. 2007;61:25–30.
Spielberger CDGR, Lushene RE. Manual for State-Trait Anxiety Inventory. California: Consulting Psychologist Press; 1970.
Oner N, Le Compte A. State-Trait Anxiety Inventory Hand Book. Istanbul: Bogazici University; 1985.
Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483.
Demiral Y, Ergor G, Unal B, et al. Normative data and discriminative properties of short form 36 (SF-36) in Turkish urban population. BMC Public Health. 2006;6:247.
Kocyigit H, Aydemir O, Fisek G, Olmez N, Memis A. Validity and reliability of Turkish version of Short form 36: a study of a patients with romatoid disorder (Turkish). İlac ve Tedavi Dergisi. 1999;12:102–106.
Gr Locke, Talley NJ, Fett SL, Zinsmeister AR, Melton Lr. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456.
Kitapcioglu G, Mandiracioglu A, Bor S. Psychometric and methodological characteristics of a culturally adjusted gastroesophageal reflux disease questionnaire. Diseases Esophagus. 2004;17:228–234.
Guz H, Ay M, Dilbaz N. Alexithymia, depression and anxiety levels in a group of dermatologic patients (Turkish). Dusunen Adam. 2000;13:161–165.
Gulec MYHÇ, Gokce M, Sayar K. Alexithymia, irritability and amplification of somatic symptoms in non-cardiac chest pain (Turkish). Anadolu Psikiyatri Dergisi. 2007;8:14–21.
Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180.
Kennedy BL, Schwab JJ, Morris RL, Beldia G. Assessment of state and trait anxiety in subjects with anxiety and depressive disorders. Psychiatry Q. 2001;72:263–276.
American Psychiatric Association. Desk Reference to the Diagnostic Criteria from DSM-5. Washington, DC: American Psychiatric Association; 2013.
Henningsen P, Zipfel S, Herzog W. Management of functional somatic syndromes. Lancet. 2007;369:946–955.
Simon GE, VonKorff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–1335.
Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: the HUNT-II study. Psychosom Med. 2004;66:845–851.
Haug TT, Mykletun A, Dahl AA. Are anxiety and depression related to gastrointestinal symptoms in the general population? Scand J Gastroenterol. 2002;37:294–298.
Choi JY, Jung HK, Song EM, Shim KN, Jung SA. Determinants of symptoms in gastroesophageal reflux disease: nonerosive reflux disease, symptomatic, and silent erosive reflux disease. Eur J Gastroenterol Hepatol. 2013;25:764–771.
Schey R, Fass R. Current perspectives on the diagnosis and treatment of functional esophageal disorders. Current GERD Reports. 2007;1:17–27.
Revicki DA, Wood M, Maton PN, Sorensen S. The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med. 1998;104:252–258.
Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377–1390.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Bilgi, M.M., Vardar, R., Yıldırım, E. et al. Prevalence of Psychiatric Comorbidity in Symptomatic Gastroesophageal Reflux Subgroups. Dig Dis Sci 62, 984–993 (2017). https://doi.org/10.1007/s10620-016-4273-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-016-4273-4