Abstract
Purpose
To identify the risk factors leading to new brain metastases (BM) following brain-directed treatment for initial BM resulting from breast cancer (BC).
Methods
In this multi-institutional study, 538 BC patients with available follow-up imaging after brain-directed treatment for initial BM were analyzed. Tumor molecular subtypes were classified as follows: hormone receptor-positive/human epidermal growth factor receptor 2-negative (HR+/HER2−, n = 136), HER2-positive (HER2+, n = 253), or triple-negative BC (TNBC, n = 149).
Results
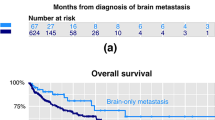
In 37.4% of patients, new BM emerged at a median of 10.5 months after brain-directed treatment for initial BM. The 1-year actuarial rate of new BM for HR+/HER2−, HER2+, and TNBC were 51.9%, 44.0%, and 69.6%, respectively (p = 0.008). Initial whole-brain radiotherapy (WBRT) reduced new BM rates (22.5% reduction at 1 year, p < 0.001) according to molecular subtype (HR+/HER2−, 42% reduction at 1 year, p < 0.001; HER2+, 18.5%, p = 0.004; TNBC, 16.9%, p = 0.071). Multivariate analysis revealed an increased risk of new BM for the following factors: shorter intervals between primary BC diagnoses and BM (p = 0.031); TNBC (relative to HR+/HER2−) (p = 0.016); presence of extracranial metastases (p = 0.019); number of BM (>4) (p < 0.001); and BM in both tentorial regions (p = 0.045). Anti-HER2 therapy in HER2+ patients (p = 0.013) and initial use of WBRT (p < 0.001) significantly lowered new BM development.
Conclusions
Tumor molecular subtypes were associated with both rates of new BM development and the effectiveness of initial WBRT. Anti-HER2 therapy in HER2+ patients significantly lowered new BM occurrence.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Tabouret E, Chinot O, Metellus P et al (2012) Recent trends in epidemiology of brain metastases: an overview. Anticancer Res 32(11):4655–4662
Leyland-Jones B (2009) Human epidermal growth factor receptor 2-positive breast cancer and central nervous system metastases. J Clin Oncol 27(31):5278–5286
Lin NU, Claus E, Sohl J et al (2008) Sites of distant recurrence and clinical outcomes in patients with metastatic triple-negative breast cancer: high incidence of central nervous system metastases. Cancer 113(10):2638–2645
Muldoon LL, Soussain C, Jahnke K et al (2007) Chemotherapy delivery issues in central nervous system malignancy: a reality check. J Clin Oncol 25(16):2295–2305
Witzel I, Oliveira-Ferrer L, Pantel K et al (2016) Breast cancer brain metastases: biology and new clinical perspectives. Breast Cancer Res 18(1):1–9
Jeon W, Jang BS, Jeon SH et al (2018) Analysis of survival outcomes based on molecular subtypes in breast cancer brain metastases: a single institutional cohort. Breast J 24(6):920–926
Sperduto PW, Kased N, Roberge D et al (2012) Effect of tumor subtype on survival and the graded prognostic assessment for patients with breast cancer and brain metastases. Int J Radiat Oncol Biol Phys 82(5):2111–2117
National Comprehensive Cancer Network (2020) Breast Cancer Version 4.2020. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 31 May 2020
National Comprehensive Cancer Network (2020) Central Nervous System Cancers Version 2.2020, https://www.nccn.org/professionals/physician_gls/pdf/cns.pdf. Accessed 31 May 2020
Aoyama H (2011) Radiation therapy for brain metastases in breast cancer patients. Breast Cancer 18(4):244–251
Brown PD, Jaeckle K, Ballman KV et al (2016) Effect of radiosurgery alone vs radiosurgery with whole brain radiation therapy on cognitive function in patients with 1 to 3 brain metastases a randomized clinical trial. JAMA 316(4):401–409
Chong JU, Ahn SG, Lee HM et al (2015) Local control of brain metastasis: treatment outcome of focal brain treatments in relation to subtypes. J Breast Cancer 18(1):29–35
Kuba S, Ishida M, Nakamura Y et al (2014) Treatment and prognosis of breast cancer patients with brain metastases according to intrinsic subtype. Jpn J Clin Oncol 44(11):1025–1031
Cagney DN, Lamba N, Montoya S et al (2019) Breast cancer subtype and intracranial recurrence patterns after brain-directed radiation for brain metastases. Breast Cancer Res Treat 176(1):171–179
Kim JS, Kim K, Jung W et al (2020) Survival outcomes of breast cancer patients with brain metastases: a multicenter retrospective study in Korea (KROG 16-12). Breast 49:41–47
El Shafie RA, Celik A, Weber D et al (2020) A matched-pair analysis comparing stereotactic radiosurgery with whole-brain radiotherapy for patients with multiple brain metastases. J Neurooncol 147(3):607–618
Kim JS, Kim IA (2020) Evolving treatment strategies of brain metastases from breast cancer: current status and future direction. Ther Adv Med Oncol 12:1758835920936117
Miller JA, Kotecha R, Ahluwalia MS et al (2017) Overall survival and the response to radiotherapy among molecular subtypes of breast cancer brain metastases treated with targeted therapies. Cancer 123(12):2283–2293
Peereboom DM, Winter KA, Kim IA et al (2019) RTOG 1119: phase II randomized study of whole brain radiotherapy with concurrent lapatinib in patients with brain metastasis from HER2-positive breast cancer—a collaborative study of RTOG and KROG (NCT01622868). J Clin Oncol 32(15_suppl):TPS664–TPS664
Regitnig P, Schippinger W, Lindbauer M et al (2004) Change of HER-2/neu status in a subset of distant metastases from breast carcinomas. J Pathol 203(4):918–926
Thomson AH, Mcgrane J, Mathew J et al (2016) Changing molecular profile of brain metastases compared with matched breast primary cancers and impact on clinical outcomes. Br J Cancer 114(7):793–800
Priedigkeit N, Hartmaier RJ, Chen Y et al (2017) Intrinsic subtype switching and acquired ERBB2/HER2 amplifications and mutations in breast cancer brain metastases. JAMA Oncol 3(5):666–671
Hulsbergen AFC, Claes A, Kavouridis VK et al (2020) Subtype switching in breast cancer brain metastases: a multicenter analysis. Neuro-Oncology 22(8):1173–1181
Jang BS, Han W, Kim IA (2019) Tumor mutation burden, immune checkpoint crosstalk and radiosensitivity in single-cell RNA sequencing data of breast cancer. Radiother Oncol 142:202–209
Funding
This work was supported by grants from the Ministry of Science and Information & Communication Technology (NRF #2017M2A2A7A01018438) and SNUBH Research Fund (#14–2919-0310) to In Ah Kim. The funding sources had no involvement in the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the institutional review board of each institution. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Because of the retrospective design of the analysis, requirement for obtaining informed consent of participants included in the study was exempted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, J.S., Kim, K., Jung, W. et al. New brain metastases after whole-brain radiotherapy of initial brain metastases in breast cancer patients: the significance of molecular subtypes (KROG 16-12). Breast Cancer Res Treat 186, 453–462 (2021). https://doi.org/10.1007/s10549-020-06043-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06043-0