Abstract
Purpose
The effect of human epidermal growth factor receptor 2 (HER2) status on mucinous carcinoma (MC) of the breast is unknown due to the rarity of HER2-positive cases. We evaluated the prognostic value of HER2 status and the efficacy of anti-HER2 therapy in patients with hormone receptor (HR)-positive MC.
Methods
From the data of 154,661 patients recorded in the Korean Breast Cancer Registry between January 1990 and August 2016, 3076 (2.0%) were diagnosed with MC. Overall survival (OS) according to HER2 status and anti-HER2 therapy was analyzed using Kaplan–Meier estimates. Multivariate analysis was performed using the Cox proportional hazards model to estimate the adjusted hazards ratio (HR) for clinicopathologic factors.
Results
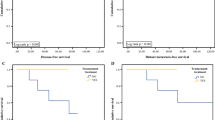
A total of 2716 HR-positive MC patients were enrolled and followed up for a median 100.1 months. Of these, 2094 (77.1%) were HER2-negative and 228 (8.4%) were HER2-positive. HR-positive, HER2-positive MC patients had more advanced pathologic tumor stages (T3 or T4) (p = 0.001), more axillary lymph node involvement (p < 0.001), higher nuclear grade (p < 0.001), and more lymphovascular invasion (p = 0.012) than HER2-negative patients. Subgroup analysis of HR-positive, node-positive MC showed that HER2-positive MC was an independent prognostic factor for OS (HR = 2.657; 95% CI, 1.665–4.241; p < 0.001). HR-positive, node-positive, and HER2-negative MC had significantly longer OS than HER2-positive MBC (p = 0.017). The node-positive subgroup that received anti-HER2 therapy had increased OS, although not significantly (p = 0.224).
Conclusion
Our nationwide database study revealed that HER2-positive status was associated with worse prognosis in HR-positive and node-positive MC. Anti-HER2 therapy might be beneficial in HR-positive, node-positive, and HER2-positive MC.


Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- HR:
-
Hormone receptor
- IDC:
-
Invasive duct carcinoma
- KBCR:
-
Korean Breast Cancer Registry
- MC:
-
Mucinous carcinoma
- OS:
-
Overall survival
- PR:
-
Progesterone receptor
References
Azzopardi JG, Ahmed A, Millis RR (1979) Problems in breast pathology. Major Probl Pathol 11(i-xvi):1–466
Fentiman IS, Millis RR, Smith P, Ellul JP, Lampejo O (1997) Mucoid breast carcinomas: histology and prognosis. Br J Cancer 75(7):1061–1065
Komaki K, Sakamoto G, Sugano H, Morimoto T, Monden Y (1988) Mucinous carcinoma of the breast in Japan: a prognostic analysis based on morphologic features. Cancer 61(5):989–996
Gallager HS (1984) Pathologic types of breast-cancer—their prognoses. Cancer 53(3):623–629. https://doi.org/10.1002/1097-0142(19840201)53:3+%3c623:Aid-Cncr2820531307%3e3.0.Co;2-Z
Lacroix-Triki M, Suarez PH, MacKay A, Lambros MB, Natrajan R, Savage K, Geyer FC, Weigelt B, Ashworth A, Reis-Filho JS (2010) Mucinous carcinoma of the breast is genomically distinct from invasive ductal carcinomas of no special type. J Pathol 222(3):282–298. https://doi.org/10.1002/path.2763
Bae SY, Choi MY, Cho DH, Lee JE, Nam SJ, Yang JH (2011) Mucinous carcinoma of the breast in comparison with invasive ductal carcinoma: clinicopathologic characteristics and prognosis. J Breast Cancer 14(4):308–313. https://doi.org/10.4048/jbc.2011.14.4.308
Rasmussen BB, Rose C, Christensen IB (1987) Prognostic factors in primary mucinous breast carcinoma. Am J Clin Pathol 87(2):155–160
Avisar E, Khan MA, Axelrod D, Oza K (1998) Pure mucinous carcinoma of the breast: a clinicopathologic correlation study. Ann Surg Oncol 5(5):447–451
Ranade A, Batra R, Sandhu G, Chitale RA, Balderacchi J (2010) Clinicopathological evaluation of 100 cases of mucinous carcinoma of breast with emphasis on axillary staging and special reference to a micropapillary pattern. J Clin Pathol 63(12):1043–1047. https://doi.org/10.1136/jcp.2010.082495
Cao AY, He M, Liu ZB, Di GH, Wu J, Lu JS, Liu GY, Shen ZZ, Shao ZM (2012) Outcome of pure mucinous breast carcinoma compared to infiltrating ductal carcinoma: a population-based study from China. Ann Surg Oncol 19(9):3019–3027. https://doi.org/10.1245/s10434-012-2322-6
Di Saverio S, Gutierrez J, Avisar E (2008) A retrospective review with long term follow up of 11,400 cases of pure mucinous breast carcinoma. Breast Cancer Res Treat 111(3):541–547. https://doi.org/10.1007/s10549-007-9809-z
Goetz MP, Gradishar WJ, Anderson BO, Abraham J, Aft R, Allison KH, Blair SL, Burstein HJ, Dang C, Elias AD, Farrar WB, Giordano SH, Goldstein LJ, Isakoff SJ, Lyons J, Marcom PK, Mayer IA, Moran MS, Mortimer J, O'Regan RM, Patel SA, Pierce LJ, Reed EC, Rugo HS, Sitapati A, Smith KL, Smith ML, Soliman H, Telli ML, Ward JH, Young JS, Shead DA, Kumar R (2019) NCCN guidelines insights: breast cancer, version 3.2018. J Natl Compr Canc Netw 17(2):118–126. https://doi.org/10.6004/jnccn.2019.0009
Fu J, Wu L, Jiang M, Li D, Jiang T, Hong Z, Wang F, Li S (2016) Clinical nomogram for predicting survival outcomes in early mucinous breast cancer. PLoS ONE 11(10):e016492. https://doi.org/10.1371/journal.pone.0164921
Slamon DJ, Clark GM, Wong SG, Levin WJ, Ullrich A, Mcguire WL (1987) Human-breast cancer—correlation of relapse and survival with amplification of the Her-2 neu oncogene. Science 235(4785):177–182. https://doi.org/10.1126/science.3798106
Gonzalez-Angulo AM, Litton JK, Broglio KR, Meric-Bernstam F, Rakkhit R, Cardoso F, Peintinger F, Hanrahan EO, Sahin A, Guray M, Larsimont D, Feoli F, Stranzl H, Buchholz TA, Valero V, Theriault R, Piccart-Gebhart M, Ravdin PM, Berry DA, Hortobagyi GN (2009) High risk of recurrence for patients with breast cancer who have human epidermal growth factor receptor 2-positive, node-negative tumors 1 cm or smaller. J Clin Oncol 27(34):5700–5706. https://doi.org/10.1200/Jco.2009.23.2025
Elston CW, Ellis IO (2002) Pathological prognostic factors in breast cancer. I: the value of histological grade in breast cancer: experience from a large study with long-term follow-up. Histopathology 41(3A):154–161
Park EH, Min SY, Kim Z, Yoon CS, Jung KW, Nam SJ, Oh SJ, Lee S, Park BW, Lim W, Hur MH, Korean Korean Breast Cancer S (2017) Basic facts of breast cancer in Korea in 2014: the 10-year overall survival progress. J Breast Cancer 20(1):1–11. https://doi.org/10.4048/jbc.2017.20.1.1
Kang SY, Kim YS, Kim Z, Kim HY, Lee SK, Jung KW, Youn HJ, Soc KBC (2018) Basic findings regarding breast cancer in Korea in 2015: data from a breast cancer registry. J Breast Cancer 21(1):1–10. https://doi.org/10.4048/jbc.2018.21.1.1
Hammond MEH, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, Hicks DG, Lester S, Love R, Mangu PB, McShane L, Miller K, Osborne CK, Paik S, Perlmutter J, Rhodes A, Sasano H, Schwartz JN, Sweep FCG, Taube S, Torlakovic EE, Valenstein P, Viale G, Visscher D, Wheeler T, Williams RB, Wittliff JL, Wolff AC (2010) American society of clinical oncology/college of American pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. Arch Pathol Lab Med 134(6):907–922
Diab SG, Clark GM, Osborne CK, Libby A, Allred DC, Elledge RM (1999) Tumor characteristics and clinical outcome of tubular and mucinous breast carcinomas. J Clin Oncol 17(5):1442–1448. https://doi.org/10.1200/JCO.1999.17.5.1442
Northridge ME, Rhoads GG, Wartenberg D, Koffman D (1997) The importance of histologic type on breast cancer survival. J Clin Epidemiol 50(3):283–290
Lei L, Yu X, Chen B, Chen Z, Wang X (2016) Clinicopathological characteristics of mucinous breast cancer: a retrospective analysis of a 10-year study. PLoS ONE 11(5):e0155132. https://doi.org/10.1371/journal.pone.0155132
Wei YN, Liu S, Zhang ML, Ke XX, Chen M, Wei B (2019) Clinicopathologic characteristics of HER2-positive pure mucinous breast carcinoma: a systematic investigation into an unusual tumor. Int J Clin Exp Patho 12(5):1666–1677
Rasmussen BB (1985) Human mucinous breast carcinomas and their lymph-node metastases—a histological review of 247 cases. Pathol Res Pract 180(4):377–382
Baretta Z, Guindalini RS, Khramtsova G, Olopade OI (2013) Resistance to trastuzumab in HER2-positive mucinous invasive ductal breast carcinoma. Clin Breast Cancer 13(2):156–158. https://doi.org/10.1016/j.clbc.2012.11.007
Hernandez IG, Marcos MC, Montemayor MG, Sotomayor DL, Ochoa DP, Macias GSG (2018) Her-2 positive mucinous carcinoma breast cancer, case report. Int J Surg Case Rep 42:242–246. https://doi.org/10.1016/j.ijscr.2017.12.025
Jang Y, Cho EY, Cho SY (2019) Human epidermal growth factor receptor 2-positive mucinous carcinoma with signet ring cell differentiation, which showed complete response after neoadjuvant chemotherapy. J Breast Cancer 22(2):336–340. https://doi.org/10.4048/jbc.2019.22.e17
Acknowledgements
This work was supported the Basic Science Research Program of the National Research Foundation funded by the Ministry of Education (2017R1D1A1B03033486).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kim, H.S., Yoo, T.K., Park, W.C. et al. The prognostic value of HER2 status and efficacy of anti-HER2 therapy in patients with HR-positive mucinous breast cancer: a nationwide study from the Korean Breast Cancer Society. Breast Cancer Res Treat 180, 461–470 (2020). https://doi.org/10.1007/s10549-020-05550-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05550-4