Abstract
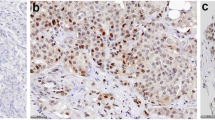
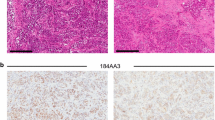
A majority of breast cancers are estrogen receptor (ER) positive and have a luminal epithelial phenotype. However, these ER+ tumors often contain heterogeneous subpopulations of ER− tumor cells. We previously identified a population of cytokeratin 5 (CK5) positive cells within ER+ and progesterone receptor positive (PR+) tumors that is both ER−PR− and CD44+, a marker of breast tumor-initiating cells (TICs). These CK5+ cells have properties of TICs in luminal tumor xenografts, and we speculated that they are more resistant to chemo- and anti-ER-targeted therapies than their ER+ neighbors. To test this, we used ER+PR+ T47D and MCF7 breast cancer cells. CK5+ cells had lower proliferative indices than CK5− cells, were less sensitive to 5-fluorouracil and docetaxel, and cultures became enriched for CK5+ cells after treatments. CK5+ cells were less prone to drug-induced apoptosis than CK5− cells. In cells treated with 17β-estradiol (E) plus anti-estrogens tamoxifen or fulvestrant, ER protein levels decreased, and CK5 protein levels increased, compared to controls treated with E alone. In ER+ tumors from patients treated with neoadjuvant endocrine therapies ER gene expression decreased, and CK5 gene expression increased in post compared to pre-treatment tumors. The number of CK5+ cells in tumors also increased in post- compared to pre-treatment tumors. We conclude that an ER−PR−CK5+ subpopulation found in many luminal tumors is resistant to standard endocrine and chemotherapies, relative to the majority ER+PR+CK5− cells. Compounds that effectively target these cells are needed to improve outcome in luminal breast cancers.






Similar content being viewed by others
Abbreviations
- AI:
-
Aromatase inhibitor
- ALDH1:
-
Aldehyde dehydrogenase 1
- BrdU:
-
5-Bromo-2-deoxyuridine
- CK:
-
Cytokeratin
- 2D:
-
Two-dimensional
- 3D:
-
Three dimensional
- DAPI:
-
4′,6-Diamidino-2-phenylindole
- Dx:
-
Docetaxel
- EGFR:
-
Epidermal growth factor receptor
- ER:
-
Estrogen receptor
- E:
-
17β-estradiol
- ESA:
-
Epithelial specific antigen
- EWD:
-
Estrogen withdrawal
- FBS:
-
Fetal bovine serum
- 5-FU:
-
5-Fluorouracil
- HER2:
-
Human epidermal growth factor receptor 2
- ICC:
-
Immunocytochemistry
- IHC:
-
Immunohistochemistry
- Lin:
-
Lineage
- MPA:
-
Medroxyprogesterone acetate
- PR:
-
Progesterone receptor
- SOC:
-
Sodium deoxycholate
- Tam:
-
4-Hydroxytamoxifen
- TIC:
-
Tumor initiating cell
- TNP:
-
Triple negative phenotype
References
Cui X, Schiff R, Arpino G et al (2005) Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol 23:7721–7735. doi:10.1200/JCO.2005.09.004
Perou CM, Sorlie T, Eisen MB et al (2000) Molecular portraits of human breast tumours. Nature 406:747–752. doi:10.1038/35021093
Paik S, Tang G, Shak S et al (2006) Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol 24:3726–3734. doi:10.1200/JCO.2005.04.7985
Osborne CK, Schiff R (2005) Estrogen-receptor biology: continuing progress and therapeutic implications. J Clin Oncol 23:1616–1622
Dean M, Fojo T, Bates S (2005) Tumour stem cells and drug resistance. Nat Rev Cancer 5:275–284. doi:10.1038/nrc1590
Diehn M, Cho RW, Lobo NA et al (2009) Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature 458:780–783. doi:10.1038/nature07733
Al-Hajj M, Wicha MS, Benito-Hernandez A et al (2003) Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA 100:3983–3988. doi:10.1073/pnas.0530291100
Fillmore CM, Kuperwasser C (2008) Human breast cancer cell lines contain stem-like cells that self-renew, give rise to phenotypically diverse progeny and survive chemotherapy. Breast Cancer Res 10:R25. doi:10.1186/bcr1982
Li X, Lewis MT, Huang J et al (2008) Intrinsic resistance of tumorigenic breast cancer cells to chemotherapy. J Natl Cancer Inst 100:672–679. doi:10.1093/jnci/djn123
Phillips TM, McBride WH, Pajonk F (2006) The response of cd24(-/low)/cd44+ breast cancer-initiating cells to radiation. J Natl Cancer Inst 98:1777–1785
Liu R, Wang X, Chen GY et al (2007) The prognostic role of a gene signature from tumorigenic breast-cancer cells. N Engl J Med 356:217–226. doi:10.1056/NEJMoa063994
Shipitsin M, Campbell LL, Argani P et al (2007) Molecular definition of breast tumor heterogeneity. Cancer Cell 11:259–273. doi:10.1016/j.ccr.2007.01.013
Abraham BK, Fritz P, McClellan M et al (2005) Prevalence of cd44+/cd24−/low cells in breast cancer may not be associated with clinical outcome but may favor distant metastasis. Clin Cancer Res 11:1154–1159
Honeth G, Bendahl PO, Ringner M et al (2008) The cd44+/cd24− phenotype is enriched in basal-like breast tumors. Breast Cancer Res 10:R53. doi:10.1186/bcr2108
Ginestier C, Hur MH, Charafe-Jauffret E et al (2007) Aldh1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell 1:555–567. doi:10.1016/j.stem.2007.08.014
Charafe-Jauffret E, Ginestier C, Iovino F et al (2009) Breast cancer cell lines contain functional cancer stem cells with metastatic capacity and a distinct molecular signature. Cancer Res 69:1302–1313. doi:10.1158/0008-5472.CAN-08-2741
O’Brien CS, Howell SJ, Farnie G et al (2009) Resistance to endocrine therapy: are breast cancer stem cells the culprits? J Mammary Gland Biol Neoplasia 14:45–54. doi:10.1007/s10911-009-9115-y
Horwitz KB, Dye WW, Harrell JC et al (2008) Rare steroid receptor-negative basal-like tumorigenic cells in luminal subtype human breast cancer xenografts. Proc Natl Acad Sci USA 105:5774–5779. doi:10.1073/pnas.0706216105
Lim E, Vaillant F, Wu D et al (2009) Aberrant luminal progenitors as the candidate target population for basal tumor development in BRCA1 mutation carriers. Nat Med 15:907–913. doi:10.1038/nm.2000
Boecker W, Buerger H (2003) Evidence of progenitor cells of glandular and myoepithelial cell lineages in the human adult female breast epithelium: a new progenitor (adult stem) cell concept. Cell Prolif 36(Suppl 1):73–84
Boecker W, Moll R, Poremba C et al (2002) Common adult stem cells in the human breast give rise to glandular and myoepithelial cell lineages: a new cell biological concept. Lab Investig 82:737–746. doi:0.1002/path.1241
Keydar I, Chen L, Karby S et al (1979) Establishment and characterization of a cell line of human breast carcinoma origin. Eur J Cancer 15:659–670
Sartorius CA, Harvell DM, Shen T et al (2005) Progestins initiate a luminal to myoepithelial switch in estrogen-dependent human breast tumors without altering growth. Cancer Res 65:9779–9788. doi:10.1158/0008-5472.CAN-05-0505
Harvell DM, Spoelstra NS, Singh M et al (2008) Molecular signatures of neoadjuvant endocrine therapy for breast cancer: characteristics of response or intrinsic resistance. Breast Cancer Res Treat 112:475–488. doi:10.1007/s10549-008-9897-4
Cheang MC, Voduc D, Bajdik C et al (2008) Basal-like breast cancer defined by five biomarkers has superior prognostic value than triple-negative phenotype. Clin Cancer Res 14:1368–1376. doi:10.1158/1078-0432.CCR-07-1658
Hugh J, Hanson J, Cheang MC et al (2009) Breast cancer subtypes and response to docetaxel in node-positive breast cancer: use of an immunohistochemical definition in the bcirg 001 trial. J Clin Oncol 27:1168–1176. doi:10.1200/JCO.2008.18.1024
Abd El-Rehim DM, Pinder SE, Paish CE et al (2004) Expression of luminal and basal cytokeratins in human breast carcinoma. J Pathol 203:661–671. doi:10.1002/path.1559
Malzahn K, Mitze M, Thoenes M et al (1998) Biological and prognostic significance of stratified epithelial cytokeratins in infiltrating ductal breast carcinomas. Virchows Arch 433:119–129
van de Rijn M, Perou CM, Tibshirani R et al (2002) Expression of cytokeratins 17 and 5 identifies a group of breast carcinomas with poor clinical outcome. Am J Pathol 161:1991–1996
Kuukasjarvi T, Kononen J, Helin H et al (1996) Loss of estrogen receptor in recurrent breast cancer is associated with poor response to endocrine therapy. J Clin Oncol 14:2584–2589
Spataro V, Price K, Goldhirsch A et al (1992) Sequential estrogen receptor determinations from primary breast cancer and at relapse: prognostic and therapeutic relevance. The international breast cancer study group (formerly Ludwig group). Ann Oncol 3:733–740
Creighton CJ, Li X, Landis M et al (2009) Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci USA 106:13820–13825. doi:10.1073/pnas.0905718106
Creighton CJ, Massarweh S, Huang S et al (2008) Development of resistance to targeted therapies transforms the clinically associated molecular profile subtype of breast tumor xenografts. Cancer Res 68:7493–7501. doi:10.1158/0008-5472.CAN-08-1404
Massarweh S, Osborne CK, Creighton CJ et al (2008) Tamoxifen resistance in breast tumors is driven by growth factor receptor signaling with repression of classic estrogen receptor genomic function. Cancer Res 68:826–833. doi:10.1158/0008-5472.CAN-07-2707
Clarke RB, Howell A, Potten CS et al (1997) Dissociation between steroid receptor expression and cell proliferation in the human breast. Cancer Res 57:4987–4991
Liedtke C, Broglio K, Moulder S et al (2009) Prognostic impact of discordance between triple-receptor measurements in primary and recurrent breast cancer. Ann Oncol 20:1953–1958. doi:10.1093/annonc/mdp263
Guarneri V, Giovannelli S, Ficarra G et al (2008) Comparison of her-2 and hormone receptor expression in primary breast cancers and asynchronous paired metastases: impact on patient management. Oncologist 13:838–844. doi:10.1634/theoncologist.2008-0048
Gupta PB, Onder TT, Jiang G et al (2009) Identification of selective inhibitors of cancer stem cells by high-throughput screening. Cell 138:645–659. doi:10.1016/j.cell.2009.06.034
Acknowledgments
This work was supported by grants from the American Society of Clinical Oncology YIA-PN200810-161 (P. Kabos), National Institutes of Health 1 F32 CA142096-01 (J.M. Haughian), Martha Cannon Dear Professorship (A. Elias), National Institutes of Health R01 CA26869 (K.B. Horwitz), Breast Cancer Research Foundation (K.B. Horwitz), the National Foundation for Cancer Research (K.B. Horwitz), The Avon Foundation (K.B. Horwitz), The Avon Foundation (C.A. Sartorius), and the University of Colorado Cancer Center (C.A. Sartorius).
Conflicts of interest
The authors have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kabos, P., Haughian, J.M., Wang, X. et al. Cytokeratin 5 positive cells represent a steroid receptor negative and therapy resistant subpopulation in luminal breast cancers. Breast Cancer Res Treat 128, 45–55 (2011). https://doi.org/10.1007/s10549-010-1078-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-010-1078-6