Abstract
Purpose
Plication is a muscle-strengthening procedure in which a muscle is not dissected from its point of insertion. The purpose of this study was to compare the results of plication–recession (PR) with those of resection–recession (RR) in adult patients with intermittent exotropia (XT).
Methods
Patients with XT who underwent either PR or RR with a minimum postoperative follow-up of 12 months were retrospectively reviewed. Postoperative mean distance deviation and surgical outcomes were compared at 1 week and at 1, 3, 6, and 12 months, and at the final follow-up. A successful outcome was defined as esophoria or esotropia ≤5 PD (prism diopters) to exophoria or exotropia ≤10 PD.
Results
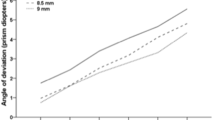
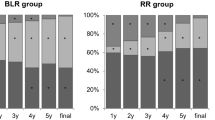
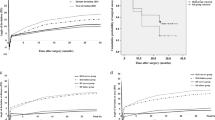
Forty-five patients underwent PR and 43 underwent RR. The mean preoperative distance deviation was 40.1 ± 12.9 PD in the PR group and 40.0 ± 14.9 PD in the RR group (P = 0.96). Mean follow-up was 21.0 ± 7.6 months for PR and 24.0 ± 8.6 months for RR (P = 0.08). The mean postoperative distance deviation at 12 months was 8.3 ± 7.4 PD for PR and 9.9 ± 9.6 PD for RR (P = 0.38). PR had a significantly better outcome than RR at 1 week (PR 89%; RR 72%; P = 0.04), but there was no difference between PR and RR at 12 months (PR 67%; RR 60%; P = 0.50).
Conclusion
PR and RR achieved comparable distance deviation and success rates at 12 months. PR had a better short-term success rate, and might prevent postoperative diplopia caused by overcorrection.


Similar content being viewed by others
References
von Noorden GK, Campos EC. Binocular vision and ocular motility: theory and management of strabismus, vol 6. St Louis: Mosby, Inc; 2002. pp. 356–76.
Nusz KJ, Mohney BG, Diehl NN. The course of intermittent exotropia in a population-based cohort. Ophthalmology. 2006;113:1154–8.
Yu CB, Fan DS, Wong VW, Wong CY, Lam DS. Changing patterns of strabismus: a decade of experience in Hong Kong. Br J Ophthalmol. 2002;86:854–6.
Jeoung JW, Lee MJ, Hwang JM. Bilateral lateral rectus recession versus unilateral recess–resect procedure for exotropia with a dominant eye. Am J Ophthalmol. 2006;141:683–8.
Suh SY, Choi J, Kim SJ. Comparative study of lateral rectus recession versus recession–resection in unilateral surgery for intermittent exotropia. J AAPOS. 2015;19:507–11.
Wang L, Wu Q, Kong X, Li Z. Comparison of bilateral lateral rectus recession and unilateral recession resection for basic type intermittent exotropia in children. Br J Ophthalmol. 2013;97:870–3.
Kim KE, Yang HK, Hwang JM. Comparison of long-term surgical outcomes of 2-muscle surgery in children with large-angle exotropia: bilateral vs unilateral. Am J Ophthalmol. 2014;157:1214–20.
Lee S, Lee YC. Relationship between motor alignment at postoperative day 1 and at year 1 after symmetric and asymmetric surgery in intermittent exotropia. Jpn J Ophthalmol. 2001;45:167–71.
Kushner BJ. Selective surgery for intermittent exotropia based on distance/near differences. Arch Ophthalmol. 1998;116:324–8.
Asjes-Tydeman WL, Groenewoud H, van der Wilt GJ. Timing of surgery for primary exotropia in children. Strabismus. 2006;14:191–7.
Chia A, Seenyen L, Long QB. Surgical experiences with two-muscle surgery for the treatment of intermittent exotropia. J AAPOS. 2006;10:206–11.
Choi J, Kim SJ, Yu YS. Initial postoperative deviation as a predictor of long-term outcome after surgery for intermittent exotropia. J AAPOS. 2011;15:224–9.
Hamtil LW. A study in tucking extraocular muscles to correct strabismus. Ann Ophthalmol. 1983;15:136–7.
Wright KW. Color atlas of strabismus surgery. 3rd ed. New York: Springer; 2007. pp. 149–52.
Mojon DS. Comparison of a new, minimally invasive strabismus surgery technique with the usual limbal approach for rectus muscle recession and plication. Br J Ophthalmol. 2007;91:76–82.
Chaudhuri Z, Demer JL. Surgical outcomes following rectus muscle plication: a potentially reversible, vessel-sparing alternative to resection. JAMA Ophthalmol. 2014;132:579–85.
Wright KW, Lanier AB. Effect of a modified rectus tuck on anterior segment circulation in monkeys. J Pediatr Ophthalmol Strabismus. 1991;28:77–81.
Oltra EZ, Pineles SL, Demer JL, Quan AV, Velez FG. The effect of rectus muscle recession, resection and plication on anterior segment circulation in humans. Br J Ophthalmol. 2015;99:556–60.
Choi J, Chang JW, Kim SJ, Yu YS. The long-term survival analysis of bilateral lateral rectus recession versus unilateral recession–resection for intermittent exotropia. Am J Ophthalmol. 2012;153:343–51.
Park H, Kim WJ, Kim MM. The stabilization of postoperative exo-drift in intermittent exotropia after surgical treatment. Korean J Ophthalmol. 2016;30:60–5.
Jung JW, Lee SY. A comparison of the clinical characteristics of intermittent exotropia in children and adults. Korean J Ophthalmol. 2010;24:96–100.
Oh JY, Hwang JM. Survival analysis of 365 patients with exotropia after surgery. Eye. 2006;20:1268–72.
Pineles SL, Deitz LW, Velez FG. Postoperative outcomes of patients initially overcorrected for intermittent exotropia. J AAPOS. 2011;15:527–31.
Cho YA, Kim SH. Postoperative minimal overcorrection in the surgical management of intermittent exotropia. Br J Ophthalmol. 2013;97:866–9.
Morrison D, McSwain W, Donahue S. Comparison of sensory outcomes in patients with monofixation versus bifoveal fusion after surgery for intermittent exotropia. J AAPOS. 2010;14:47–51.
Conflicts of interest
Y. Kimura, None; T. Kimura, None.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kimura, Y., Kimura, T. Comparative study of plication–recession versus resection–recession in unilateral surgery for intermittent exotropia. Jpn J Ophthalmol 61, 286–291 (2017). https://doi.org/10.1007/s10384-017-0501-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10384-017-0501-5