Abstract
During surgeries in the upper cerebellopontine angle (CPA), the superior petrosal veins (SPVs) often act as obstacles; and their sectioning sometimes causes serious complications. In this study, we introduced a classification system for the SPVs wherein their tributaries were classified into four groups on the basis of their courses and draining areas. We furthermore explained the detailed anatomy of the vein of the cerebellopontine fissure, which is the largest tributary. In surgeries of petrous apex meningioma, the knowledge of the displacement pattern of the vein is very helpful for avoiding major venous complications. Therefore, we elucidated its anatomical situation in relation to the original portion of the meningioma and the natural draining point of the vein into the superior petrosal sinus (SPS) in each patient. In addition, we described the methods and techniques used to expose and manage the vein of the cerebellopontine fissure during surgery using the lateral suboccipital retrosigmoid approach. Presenting two illustrative cases, we recommend that the initial exposure of the tumor should be performed through the infratentorial lateral supracerebellar route and that the suprafloccular cistern is the best area to find the vein of the cerebellopontine fissure. We emphasized the importance of the preservation of the vein of the cerebellopontine fissure and also proposed the order for exposure of SPV tributaries during upper CPA surgery using the retrosigmoid approach.








Similar content being viewed by others
References
Bambakidis NC, Kakarla UK, Kim LJ, Nakaji P, Porter RW, Daspit CP, Spetzler RF (2007) Evolution of surgical approaches in the treatment of petroclival meningiomas: a retrospective review. Neurosurgery 61(ONS Suppl 2):ONS202–ONS211
BarkerII FG, Jannetta PJ, Bissonette DJ, Larkins MV, Jho HD (1996) The long-term outcome of microvascular decompression for trigeminal neuralgia. N Engl J Med 334:1077–1083
Bricolo AP, Turazzi S, Talacchi A, Cristofori L (1992) Microsurgical removal of petroclival meningiomas: a report of 33 patients. Neurosurgery 31:813–828
Chen LF, Yu XG, Bu B, Xu BN, Zhou DB (2011) The retrosigmoid approach to petroclival meningioma surgery. J Clin Neurosci 18:656–1661
Choudhari KA (2007) Superior petrosal vein in trigeminal neuralgia. Br J Neurosurg 21:288–292
Dandy WE (1929) An operation for the cure of tic douloureux. Partial section of the sensory root at the pons. Arch Surg 18:687–734
Distelmaier P (1976) Complications of the operative neurosurgical treatment of trigeminal neuralgia. Zentralbl Neurochir 37:119–125
Ebner FH, Roser F, Shiozawa T, Ruetschlin S, Kirschniak A, Koerbel A, Tatagiba M (2009) Petrosal vein occlusion in cerebello-pontine angle tumour surgery: an anatomical study of alternative draining pathways. Eur J Surg Oncol 35:552–556
Fujimaki T, Kirino T (2000) Combined transhorizontal-supracerebellar approach for microvascular decompression of trigeminal neuralgia. Br J Neurosurg 14:531–534
Goel A, Muzumdar D (2004) Conventional posterior fossa approach for surgery on petroclival meningiomas: a report on an experience with 28 cases. Surg Neurol 62:332–340
Huang YP, Wolf BS (1968) The vein of the posterior fossa–anterior or petrosal draining group. Am J Roentgenol Radium Ther Nucl Med 104:36–56
Inamasu J, Shiobara R, Kawase T, Kanzaki J (2002) Haemorrhagic venous infarction following the posterior petrosal approach for acoustic neurinoma surgery: a report of two cases. Eur Arch Otorhinolaryngol 259:162–165
Kaku S, Miyahara K, Fujitsu K, Hataoka S, Tanino S, Okada T, Ichikawa T (2012) Drainage pathway of the superior petrosal vein evaluated by CT-venography in petroclival meningioma surgery. J Neurol Surg B 73:316–320
Kawamata T, Katayama Y (2006) Lateral supracerebellar transtentorial approach for petroclival lesions. No Shinkei Geka 34:567–575 (in Japanese with English abstract)
Koerbel A, Gharabaghi A, Safavi-Abbasi S, Samii A, Ebner FH, Samii M, Tatagiba M (2009) Venous complications following petrosal vein sectioning in surgery of petrous apex meningiomas. Eur J Surg Oncol 35:773–779
Masuoka J, Matsushima T, Hikita T, Inoue E (2009) Cerebellar swelling after sacrifice of the superior petrosal vein during microvascular decompression for trigeminal neuralgia. J Clin Neurosci 16:1342–1344
Matsushima T (2006) Microneurosurgical anatomy and surgeries of the posterior fossa. Scimed Publications, Tokyo (in Japanese)
Matsushima T, Fukui M, Suzuki S, Rhoton AL Jr (1989) The microsurgical anatomy of the infratentorial lateral supracerebellar approach to the trigeminal nerve for tic doulourex. Neurosurgery 24:890–895
Matsushima T, Masuoka J, Kawashima M, Inoue K, Mineta T (2008) Petroclival region tumor surgery and the related veins. Jpn J Neurosurg (Tokyo) 17:761–772 (in Japanese with English abstract)
Matsushima T, Rhoton AL Jr, de Oliveira E, Peace D (1983) Microsurgical anatomy of the veins of the posterior fossa. J Neurosurg 59:63–105
Nakase H, Shin Y, Nakagawa I, Kimura R, Sakaki T (2005) Clinical features of postoperative cerebral venous infarction. Acta Neurochir (Wein) 147:621–626, discussion 626
Ryu H, Yamamoto S, Sugiyama K, Yokota N, Tanaka T (1999) Neurovascular decompression for trigeminal neuralgia in elderly patients. Neurol Med Chir (Tokyo) 39:226–229, discussion 229–230
Samii M, Gerganov VM (2010) Petroclival meningiomas: suboccipital retrosigmoid approach. In: Pamir MN, Black PM, Fahlbusch R (eds) Meningiomas: a comprehensive text. Saunders, Pennsylvania, pp 503–510
Samii M, Tatagiba M, Carvalho GA (1999) Resection of large petroclival meningiomas by the simple retrosigmoid route. J Clin Neurosci 6:27–30
Schweder P, Kaye AH (2010) The surgical management of cerebellopontine angle meningiomas. In: Pamir MN, Black PM, Fahlbusch R (eds) Meningiomas: a comprehensive text. Saunders, Pennsylvania, pp 529–534
Singh D, Jagetia A, Sinha S (2006) Brain stem infarction: a complication of microvascular decompression for trigeminal neuralgia. Neurol India 54:325–326
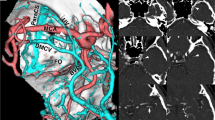
Takao T, Kouguchi M, Nakahara Y, Kawashima M, Matsushima T (2011) Three-dimensional images of petrosal veins for preoperative evaluation: four case reports. No Shinkei Geka 39:1175–1181 (in Japanese with English abstract)
Takusagawa Y (2008) Microvascular decompression for trigeminal neuralgia: how to obtain sufficiently large operative working space. Jpn J Neurosurg (Tokyo) 17:199–204 (in Japanese with English abstract)
Tanriover N, Abe H, Rhoton AL, Kawashima M, Sanus GZ, Akar Z (2007) Microsurgical anatomy of the superior petrosal venous complex: new classifications and implications for subtemporal transtentorial and retrosigmoid suprameatal approaches. J Neurosurg 106:1041–1050
Tsukamoto H, Matsushima T, Fujiwara S, Fukui M (1993) Peduncular hallucinosis following microvascular decompression for trigeminal neuralgia: case report. Surg Neurol 40:31–34
Ward C, Corns R, Offa-Jones B, Cheserem JB, Hardwidge C (2012) Cerebellar infarction following division of Dandy’s vein in microvascular decompression for trigeminal neuralgia. J Neurol Surg B73:A380
Watanabe T, Katayama Y, Fukushima T, Kawamata T (2011) Lateral supracerebellar transtentorial approach for petroclival meningiomas: operative technique and outcome. J Neurosurg 115:49–54
Zhong J, Li ST, Xu SQ, Wan L, Wang X (2008) Management of petrosal veins during microvascular decompression for trigeminal neuralgia. Neurol Res 30:697–700
Acknowledgments
We would like to express our gratitude to Prof. Rhoton, University of Florida, for giving us the opportunity to study the microsurgical anatomy of the veins of the posterior fossa. We also thank Ms. Takako Shiga and Ms. Sumiko Matsushima for assisting in preparing this manuscript and illustrations.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Andrei Koerbel, Joinville, Brazil
This manuscript provides an interesting review on the petrosal vein drainage pathways, their relationship with petrous apex meningiomas and the risks of sacrificing these veins. The topic is very important, since the risks of sacrificing the petrosal veins have been underestimated by many neurosurgeons. The most usual relationships of petrous apex tumors with petrosal vein complexes should be known by neurosurgeons that treat these lesions. Thus, these interconnections should be taken in consideration to choose the safest surgical strategy.
Some intraoperative maneuvers may increase the rates of petrosal vein preservation in petrous apex meningiomas. In my experience, the intraoperative management of the spatula for cerebellar retraction is the most important issue. When the spatula is positioned on the cerebellar surface, the direction of the retraction is essential. The cerebellar retraction may cause a vein rupture, mainly if the traction is applied on the superolateral cerebellar surface to the inferior or medial direction. If the traction is applied on the inferolateral cerebellar surface to medial-superior direction, tension on the superior petrosal veins is avoided. This procedure allows exposing the petrous apex without stretching the superior petrosal vein complex. The other maneuvers described by the authors are meaningful and may be used according to specific situations. However, in most cases, the safest strategy is to avoid stretching the superior petrosal veins during cerebellar retraction.
ᅟ
Feng Xu and Nicholas Bambakidis, Cleveland, USA
The venous drainage system of the superior petrosal vein (SPVs) has received increasing attention during surgery in the upper cerebellopontine angle. Preservation of the SPVs should be attempted whenever possible to minimize the risk of venous complications such as cerebellar and brainstem edema and hemorrhagic infarction. The authors depict the anatomy of SPVs tributaries and the impact of surgical manipulation during petrous epex meningioma resection using the lateral subocciptal retrosigmoid approach. The authors nicely demonstrated the suprafollicular cistern as a landmark to identify the vein of cerebellopontine fissure in the infratentorial lateral supracerebellar route. We agree that the angioarchitecture of cerebellopontine-cerebellomedullary veins described in petrous meningioma surgery is more complex compared to anatomy of microvascular decompression, as there are no major venous channel displacements (depending on the origin, axis or direction of tumor growth and effect of local vascularity of tumor mass itself) in the latter. The vein of cerebellomesencphalic fissure and the common stem of SPVs should be preserved, whereas the tributaries of the tentorial cerebellar surface draining group might be sacrificed under certain circumstances.
The infratentorial lateral supracerebellar approach described in the article is best suited for petroclival miningiomas located mainly in the posterior fossa with less extension into the middle fossa. In the lateral supracerebellar transtentorial approach, the tentorial medial to the trigeminal nerve is incised toward the free edge, which improves exposure to the petroclival area and permits free access to the middle fossa. When the tumor has a larger supratentorial extension, one stage tumor remover through the transpetrosal approach or a two-stage surgery combining retrosigmoid suprameatal and frontotemporal approaches might be selected.
We find that in such cases (large tumors medial to the internal auditory canal with both middle and posterior fossa extension) that a combined transpetrosal approach is best considered. In these cases, splitting of the tentorium to access the middle fossa tumor component necessitates division of the SPV. Careful attention to the overall venous pattern of drainage is thus required during preoperative surgical assessment.
References
1. Xu F, Karampelas I, Megerian CA, Selman WR, Bambakidis NC. Petroclival meningiomas—an update on surgical approaches, decision making, and treatment results. Neurosurg Focus 2013 Dec;35(6):E11
ᅟ
Tiit Mathiesen, Stockholm, Sweden
A group of very experienced surgeons extended the meningioma society meetings with meetings “on the cerebral venous system”. With time, I think I have realized why this was realized by renowed, experienced microsurgeons. Unexpected and uncommon complications are the most common remaing complications, when skill and experience has done away with “beginners mistakes”—and venous complications can be very treacherous and unpredictable.
The cerebellar drainage system has a fair degree of variability, and routine sacrifice of major draining veins such as the superior petrosal vein, vermian veins and tentorial draining veins can frequently—but not always—be done with impunity. Experienced surgeons cite complications from ssacrifice of the petrosal vein; we recently published a nearly fatal cerebellar venous infarct from sacrifice of one (!) cerebellar draining vein. Sacrifice of normal structures to improve exposure is one way to increase safety, but knowledge of risk with such maneuvers is indispensable unless we are prepare to accept a random risk of serious venous complications. Professor Matsushima has devoted a large part of his professional carreer to the meticulous study of surgical anatomy, especially of the posterior fossa. I am grateful for this opportunity to get a more profound understanding of his surgical concepts, that are firmly rooted in the respect of normal anatomy and strive for excellent outcomes.
Rights and permissions
About this article
Cite this article
Matsushima, T., Kawashima, M., Inoue, K. et al. Anatomy of the superior petrosal veins and their exposure and management during petrous apex meningioma surgery using the lateral suboccipital retrosigmoid approach. Neurosurg Rev 37, 535–546 (2014). https://doi.org/10.1007/s10143-014-0548-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-014-0548-4