Abstract
Objective
To evaluate long-term results after one-, two-, and three-level anterior cervical discectomy and fusion (ACDF) with stand-alone empty polyetheretherketone (PEEK) cages.
Methods
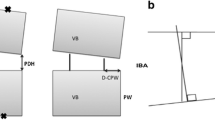
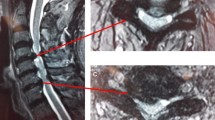
We performed a retrospective review of a consecutive patient cohort that underwent ACDF with stand-alone empty PEEK cages between 2007 and 2010 with a minimum follow-up of 12 months. Radiographic follow-up included static and flexion/extension radiographs. Changes in the operated segments were measured and compared to radiographs directly after surgery. Clinical outcome was evaluated by a physical examination, pain visual analog scale (VAS), and health-related quality of life (HRQL) using the EuroQOL questionnaire (EQ-5D). Analysis of associations between fusion, subsidence, cervical alignment, and clinical outcome parameters were performed.
Results
Of 407 consecutive cases, 318 met all inclusion criteria. Follow-up data were obtained from 265 (83 %) cases. The mean age at presentation was 55 years and 139 patients were male (52 %). In the sample, 127, 125, and 13 patients had one-, two-, and three-level surgeries, respectively; 132 (49 %) presented with spondylotic cervical myelopathy and 133 (50 %) with cervical radiculopathy. Fusion was achieved in 85, 95, and 94 % of segments in one-, two-, and three-level surgeries, respectively. Non-fusion was associated with higher VAS pain levels. Radiographic adjacent segment disease (ASD) was observed in 20, 29, and 15 % in one-, two-, and three-level surgeries, respectively. ASD was associated with lower HRQL. Subsidence was observed in 25, 27, and 15 % of segments in one-, two-, and three-level surgeries, respectively. However, this had no influence on clinical outcome. Follow-up operations for symptomatic adjacent disc disease and implant failure at index level were needed in 16 (6 %) and four (1.5 %) cases, respectively. Younger age was associated with better clinical outcome. Multilevel surgery favored better myelopathy outcomes and fusion reduced overall pain. ASD worsened EuroQOL-Index values. Worsening of the cervical alignment induced arm pain.
Conclusions
One- and two-level ACDF with stand-alone empty PEEK cages achieved very high fusion rates and a low rate of follow-up operations. The rate of good clinical outcome is highly satisfactory. Younger age was the single most influential factor associated with better clinical outcome.



Similar content being viewed by others
References
Anderson PA, Subach BR, Riew KD (2009) Predictors of outcome after anterior cervical discectomy and fusion: a multivariate analysis. Spine (Phila Pa 1976) 34:161–166
Barsa P, Suchomel P (2007) Factors affecting sagittal malalignment due to cage subsidence in standalone cage assisted anterior cervical fusion. Eur Spine J 16:1395–1400
Bydon M, Xu R, De la Garza-Ramos R, Macki M, Sciubba DM, Wolinsky JP, Witham TF, Gokaslan ZL, Bydon A (2014) Adjacent segment disease after anterior cervical discectomy and fusion: incidence and clinical outcomes of patients requiring anterior versus posterior repeat cervical fusion. Surg Neurol Int 5:74–78
Cabraja M, Oezdemir S, Koeppen D, Kroppenstedt S (2012) Anterior cervical discectomy and fusion: comparison of titanium and polyetheretherketone cages. BMC Musculoskelet Disord 13:172
Chagas H, Domingues F, Aversa A, Vidal Fonseca AL, de Souza JM (2005) Cervical spondylotic myelopathy: 10 years of prospective outcome analysis of anterior decompression and fusion. Surg Neurol 64:30–35
Chen Y, Wang X, Lu X, Yang L, Yang H, Yuan W, Chen D (2013) Comparison of titanium and polyetheretherketone (PEEK) cages in the surgical treatment of multilevel cervical spondylotic myelopathy: a prospective, randomized, control study with over 7-year follow-up. Eur Spine J 22:1539–1546
Chou YC, Chen DC, Hsieh WA, Chen WF, Yen PS, Harnod T, Chiou TL, Chang YL, Su CF, Lin SZ, Chen SY (2008) Efficacy of anterior cervical fusion: comparison of titanium cages, polyetheretherketone (PEEK) cages and autogenous bone grafts. J Clin Neurosci 15:1240–1245
Cloward RB (1958) The anterior approach for removal of ruptured cervical disks. J Neurosurg 15:602–617
Demircan MN, Kutlay AM, Colak A, Kaya S, Tekin T, Kibici K, Ungoren K (2007) Multilevel cervical fusion without plates, screws or autogenous iliac crest bone graft. J Clin Neurosci 14:723–728
Dufour T, Huppert J, Louis C, Beaurain J, Stecken J, Aubourg L, Vila T (2010) Radiological analysis of 37 segments in cervical spine implanted with a peek stand-alone device, with at least one-year follow-up. Br J Neurosurg 24:633–640
Ebersold MJ, Pare MC, Quast LM (1995) Surgical treatment for cervical spondylotic myelopathy. J Neurosurg 82:745–751
Ferch RD, Shad A, Cadoux-Hudson TA, Teddy PJ (2004) Anterior correction of cervical kyphotic deformity: effects on myelopathy, neck pain, and sagittal alignment. J Neurosurg 100:13–19
Fujiwara K, Yonenobu K, Ebara S, Yamashita K, Ono K (1989) The prognosis of surgery for cervical compression myelopathy. An analysis of the factors involved. J Bone Joint Surg Br 71:393–398
Gercek E, Arlet V, Delisle J, Marchesi D (2003) Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J 12:513–516
Gore DR, Sepic SB, Gardner GM (1986) Roentgenographic findings of the cervical spine in asymptomatic people. Spine (Phila Pa 1976) 11:521–524
Handa Y, Kubota T, Ishii H, Sato K, Tsuchida A, Arai Y (2002) Evaluation of prognostic factors and clinical outcome in elderly patients in whom expansive laminoplasty is performed for cervical myelopathy due to multisegmental spondylotic canal stenosis. A retrospective comparison with younger patients. J Neurosurg 96:173–179
Harrison DD, Harrison DE, Janik TJ, Cailliet R, Ferrantelli JR, Haas JW, Holland B (2004) Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine 29:2485–2492
Hermansen A, Hedlund R, Vavruch L, Peolsson A (2013) Positive predictive factors and subgroup analysis of clinically relevant improvement after anterior cervical decompression and fusion for cervical disc disease: a 10- to 13-year follow-up of a prospective randomized study: clinical article. J Neurosurg Spine 19:403–411
Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH (1999) Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 81:519–528
Hilibrand AS, Robbins M (2004) Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 4:190S–194S
Hwang SL, Lee KS, Su YF, Kuo TH, Lieu AS, Lin CL, Howng SL, Hwang YF (2007) Anterior corpectomy with iliac bone fusion or discectomy with interbody titanium cage fusion for multilevel cervical degenerated disc disease. J Spinal Disord Tech 20:565–570
Jacobs W, Willems PC, Kruyt M, van Limbeek J, Anderson PG, Pavlov P, Bartels R, Oner C (2011) Systematic review of anterior interbody fusion techniques for single- and double-level cervical degenerative disc disease. Spine (Phila Pa 1976) 36:E950–960
Kaiser MG, Mummaneni PV, Matz PG, Anderson PA, Groff MW, Heary RF, Holly LT, Ryken TC, Choudhri TF, Vresilovic EJ, Resnick DK (2009) Joint section on disorders of the spine and peripheral nerves of the American Association of Neurological Surgeons and Congress of Neurological Surgeons. Radiographic assessment of cervical subaxial fusion. J Neurosurg Spine 11:221–227
Karikari IO, Jain D, Owens TR, Gottfried O, Hodges TR, Nimjee SM, Bagley CA (2014) Impact of subsidence on clinical outcomes and radiographic fusion rates in anterior cervical discectomy and fusion: a systematic review. J Spinal Disord Tech 27:1–10
Katsuura A, Hukuda S, Saruhashi Y, Mori K (2001) Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J 10:320–324
Kim CH, Chung CK, Hahn S (2013) Autologous iliac bone graft with anterior plating is advantageous over the stand-alone cage for segmental lordosis in single-level cervical disc disease. Neurosurgery 72:257–265
Kulkarni AG, Hee HT, Wong HK (2007) Solis cage (PEEK) for anterior cervical fusion: preliminary radiological results with emphasis on fusion and subsidence. Spine J 7:205–209
Laing RJ, Ng I, Seeley HM, Hutchinson PJ (2001) Prospective study of clinical and radiological outcome after anterior cervical discectomy. Br J Neurosurg 15:319–323
Maldonado CV, Paz RD, Martin CB (2011) Adjacent-level degeneration after cervical disc arthroplasty versus fusion. Eur Spine J 20:403–407
Matsumoto M, Okada E, Ichihara D, Watanabe K, Chiba K, Toyama Y, Fujiwara H, Momoshima S, Nishiwaki Y, Iwanami A, Ikegami T, Takahata T, Hashimoto T (2010) Anterior cervical decompression and fusion accelerates adjacent segment degeneration: comparison with asymptomatic volunteers in a ten-year magnetic resonance imaging follow-up study. Spine (Phila Pa 1976) 35:36–43
Mummaneni PV, Burkus JK, Haid RW, Traynelis VC, Zdeblick TA (2007) Clinical and radiographic analysis of cervical disc arthroplasty compared with allograft fusion: a randomized controlled clinical trial. J Neurosurg Spine 6:198–209
Naderi S, Ozgen S, Pamir MN, Ozek MM, Erzen C (1998) Cervical spondylotic myelopathy: surgical results and factors affecting prognosis. Neurosurgery 43:43–49
Niu CC, Liao JC, Chen WJ, Chen LH (2010) Outcomes of interbody fusion cages used in 1 and 2-levels anterior cervical discectomy and fusion: titanium cages versus polyetheretherketone (PEEK) cages. J Spinal Disord Tech 23:310–316
Nunley PD, Jawahar A, Kerr EJ 3rd, Gordon CJ, Cavanaugh DA, Birdsong EM, Stocks M, Danielson G (2012) Factors affecting the incidence of symptomatic adjacent-level disease in cervical spine after total disc arthroplasty: 2- to 4-year follow-up of 3 prospective randomized trials. Spine (Phila Pa 1976) 37:445–451
Park MS, Kelly MP, Lee DH, Min WK, Rahman RK, Riew KD (2013) Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J 14:1228–1234
Payer M, May D, Reverdin A, Tessitore E (2003) Implantation of an empty carbon fiber composite frame cage after single-level anterior cervical discectomy in the treatment of cervical disc herniation: preliminary results. J Neurosurg 98(2 Suppl):143–148
Prasarn ML, Baria D, Milne E, Latta L, Sukovich W (2012) Adjacent-level biomechanics after single versus multilevel cervical spine fusion. J Neurosurg Spine 16:172–177
Peolsson A, Almkvist C, Dahlberg C, Lindqvist S, Pettersson S (2007) Age- and sex-specific reference values of a test of neck muscle endurance. J Manip Physiol Ther 30:171–177
Peolsson A, Peolsson M (2008) Predictive factors for long-term outcome of anterior cervical decompression and fusion: a multivariate data analysis. Eur Spine J 17:406–414
Schils F, Rilliet B, Payer M (2006) Implantation of an empty carbon fiber cage or a tricortical iliac crest autograft after cervical discectomy for single-level disc herniation: a prospective comparative study. J Neurosurg Spine 4:292–299
Thomé C, Krauss JK, Zevgaridis D (2004) A prospective clinical comparison of rectangular titanium cages and iliac crest autografts in anterior cervical discectomy and fusion. Neurosurg Rev 27:34–41
Topuz K, Colak A, Kaya S, Simşek H, Kutlay M, Demircan MN, Velioğlu M (2009) Two-level contiguous cervical disc disease treated with peek cages packed with demineralized bone matrix: results of 3-year follow-up. Eur Spine J 18:238–243
Villavicencio AT, Babuska JM, Ashton A, Busch E, Roeca C, Nelson EL, Mason A, Burneikiene S (2009) Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 68:1309–1316
Wright IP, Eisenstein SM (2007) Anterior cervical discectomy and fusion without instrumentation. Spine (Phila Pa 1976) 32:772–774
Wu WJ, Jiang LS, Liang Y, Dai LY (2012) Cage subsidence does not, but cervical lordosis improvement does affect the long-term results of anterior cervical fusion with stand-alone cage for degenerative cervical disc disease: a retrospective study. Eur Spine J 21:1374–1382
Yamazaki T, Yanaka K, Sato H, Uemura K, Tsukada A, Nose T (2003) Cervical spondylotic myelopathy: surgical results and factors affecting outcome with special reference to age differences. Neurosurgery 52:122–126
Yu S, Li F, Yan N, Yuan C, He S, Hou T (2011) Anterior fusion technique for multilevel cervical spondylotic myelopathy: a retrospective analysis of surgical outcome of patients with different number of levels fused. PLoS ONE 9, e91329
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Disclosure
The authors declare that they have no conflict of interest affecting this study. The study was completely financed by the Department of Neurosurgery.
Rights and permissions
About this article
Cite this article
Shiban, E., Gapon, K., Wostrack, M. et al. Clinical and radiological outcome after anterior cervical discectomy and fusion with stand-alone empty polyetheretherketone (PEEK) cages. Acta Neurochir 158, 349–355 (2016). https://doi.org/10.1007/s00701-015-2630-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2630-2