Abstract
Purpose
The purpose of this prospective, observational study was to respiratory variation of stroke volume (stroke volume variation, SVV) against central venous pressure (CVP) and pulmonary artery diastolic pressure (PADP) as an estimate of right and left ventricular preload.
Methods
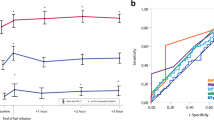
With IRB approval and informed consent, 31 patients undergoing living related renal transplantation were analyzed. Under general anesthesia with positive pressure ventilation, stroke volume index and SVV were continuously monitored with FloTrac/Vigileo monitor. Right ventricular end-diastolic volume index (RVEDVI) as well as CVP and PADP were continuously monitored with volumetric pulmonary artery catheter. Data of every 30 min interval were used for analysis. The relationship between RVEDVI and CVP, PADP, SVV was analyzed with non-linear regression and the goodness-of-fit was assessed with coefficient of determination (R 2) of each regression curve. The ability of CVP, PADP and SVV to correctly differentiate RVEDVI <100, <120 or >138 ml/m2, which were used to guide fluid administration, was also assessed with ROC analysis.
Results
Three hundred forty-eight data sets were obtained and analyzed. The goodness of fit between RVEDVI and SVV (R 2 = 0.48) was better than that between RVEDVI and CVP or PADP (R 2 = 0.19 and 0.33, respectively). The area under the ROC curve of SVV was significantly high compared to CVP or PADP.
Conclusions
This study confirmed the theoretical framework of right ventricular preload and ventricular filling pressure and respiratory variation of stroke volume. The result also suggests that SVV can correctly predict preload status compared to pressure-based indices.




Similar content being viewed by others
References
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121:2000–8.
Osman D, Ridel C, Ray P, Monnet X, Anguel N, Richard C, Teboul JL. Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Crit Care Med. 2007;35:64–8.
Biais M, Nouette-Gaulain K, Cottenceau V, Revel P, Sztark F. Uncalibrated pulse contour-derived stroke volume variation predicts fluid responsiveness in mechanically ventilated patients undergoing liver transplantation. Br J Anaesth. 2008;101:761–8.
Cannesson M, Musard H, Desebbe O, Boucau C, Simon R, Henaine R, Lehot JJ. The ability of stroke volume variations obtained with Vigileo/FloTrac system to monitor fluid responsiveness in mechanically ventilated patients. Anesth Analg. 2009;108:513–7.
Forget P, Lois F, de Kock M. Goal-directed fluid management based on the pulse oximeter-derived pleth variability index reduces lactate levels and improves fluid management. Anesth Analg. 2010;111:910–4.
Biancofiore G, Critchley LA, Lee A, Yang XX, Bindi LM, Esposito M, Bisa M, Meacci L, Mozzo R, Filipponi F. Evaluation of a new software version of the FloTrac/Vigileo (version 3.02) and a comparison with previous data in cirrhotic patients undergoing liver transplant surgery. Anesth Analg. 2011;113:515–22.
Tsai YF, Su BC, Lin CC, Liu FC, Lee WC, Yu HP. Cardiac output derived from arterial pressure waveform analysis: validation of the third-generation software in patients undergoing orthotopic liver transplantation. Transpl Proc. 2012;44:433–7.
Hein M, Roehl AB, Baumert JH, Rossaint R, Steendijk P. Continuous right ventricular volumetry by fast-response thermodilution during right ventricular ischemia: head-to-head comparison with conductance catheter measurements. Crit Care Med. 2009;37:2962–7.
Sprung J, Kapural L, Bourke DL, O’Hara JF Jr. Anesthesia for kidney transplant surgery. Anesthesiol Clin North Am. 2000;18:919–51.
He Z, Qiao H, Zhou W, Wang Y, Xu Z, Che X, Zhang J, Liang W. Assessment of cardiac preload status by pulse pressure variation in patients after anesthesia induction: comparison with central venous pressure and initial distribution volume of glucose. J Anesth. 2011;25:812–7.
Kincaid EH, Meredith JW, Chang MC. Determining optimal cardiac preload during resuscitation using measurements of ventricular compliance. J Trauma. 2001;50:665–9.
Diebel LN, Wilson RF, Tagett MG, Kline RA. End-diastolic volume. A better indicator of preload in the critically ill. Arch Surg. 1992;127:817–21.
Chang MC, Meredith JW. Cardiac preload, splanchnic perfusion, and their relationship during resuscitation in trauma patients. J Trauma. 1997;42:577–82.
Miller PR, Meredith JW, Chang MC. Randomized, prospective comparison of increased preload versus inotropes in the resuscitation of trauma patients: effects on cardiopulmonary function and visceral perfusion. J Trauma. 1998;44:107–13.
Akobeng AK. Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr. 2007;96:644–7.
Reuter DA, Goetz AE. Differentiating “volumetric preload monitoring” and assessing “fluid responsiveness”. Anesth Analg. 2006;102:651–2.
Kumar A, Anel R, Bunnell E, Habet K, Zanotti S, Marshall S, Neumann A, Ali A, Cheang M, Kavinsky C, Parrillo JE. Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med. 2004;32:691–9.
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134:172–8.
Marik PE, Cavallazzi R, Vasu T, Hirani A. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients: a systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Zhang Z, Lu B, Sheng X, Jin N. Accuracy of stroke volume variation in predicting fluid responsiveness: a systematic review and meta-analysis. J Anesth. 2011;25:904–16.
Michard F. Stroke volume variation: from applied physiology to improved outcomes. Crit Care Med. 2011;39:402–3.
Biais M, Ouattara A, Janvier G, Sztark F. Case scenario: respiratory variations in arterial pressure for guiding fluid management in mechanically ventilated patients. Anesthesiology. 2012;116:1354–61.
Spahn DR, Chassot PG. CON: fluid restriction for cardiac patients during major noncardiac surgery should be replaced by goal-directed intravascular fluid administration. Anesth Analg. 2006;102:344–6.
Su BC, Tsai YF, Cheng CW, Yu HP, Yang MW, Lee WC, Lin CC. Stroke volume variation derived by arterial pulse contour analysis is a good indicator for preload estimation during liver transplantation. Transpl Proc. 2012;44:429–32.
Spohr F, Hettrich P, Bauer H, Haas U, Martin E, Bottiger BW. Comparison of two methods for enhanced continuous circulatory monitoring in patients with septic shock. Intensive Care Med. 2007;33:1805–10.
Michard F. Changes in arterial pressure during mechanical ventilation. Anesthesiology. 2005;103:419–28.
Taguchi H, Ichinose K, Tanimoto H, Sugita M, Tashiro M, Yamamoto T. Stroke volume variation obtained with Vigileo/FloTrac system during bleeding and fluid overload in dogs. J Anesth. 2011;25:563–8.
Ytrebo LM. Stop filling patients against central venous pressure, please! Crit Care Med. 2011;39:396–7.
Wagner JG, Leatherman JW. Right ventricular end-diastolic volume as a predictor of the hemodynamic response to a fluid challenge. Chest. 1998;113:1048–54.
Zink W, Noll J, Rauch H, Bauer H, Desimone R, Martin E, Bottiger BW. Continuous assessment of right ventricular ejection fraction: new pulmonary artery catheter versus transoesophageal echocardiography. Anaesthesia. 2004;59:1126–32.
De Simone R, Wolf I, Mottl-Link S, Bottiger BW, Rauch H, Meinzer HP, Hagl S. Intraoperative assessment of right ventricular volume and function. Eur J Cardiothorac Surg. 2005;27:988–93.
Arinc H, Gunduz H, Tamer A, Ozhan H, Akdemir R, Saglam H, Oguzhan A, Uyan C. Use of tissue Doppler to assess right ventricle function in hemodialysis patients. Am J Nephrol. 2005;25:256–61.
Paneni F, Gregori M, Ciavarella GM, Sciarretta S, De Biase L, Marino L, Tocci G, Principe F, Domenici A, Luciani R, Punzo G, Mene P, Volpe M. Right ventricular dysfunction in patients with end-stage renal disease. Am J Nephrol. 2010;32:432–8.
Acknowledgments
This work is supported by JSPS KAKENHI Grant Number 24592361.
Conflict of interest
Dr. Kotake has received consultant fee from Edwards Lifesciences and unrestricted research fund from MSD, Nihon Koden Corp. Dr. Kotake has also received speakers fee from MSD, Fresenius-Kabi, Otsuka Pharmaceuticals and Covidien.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Toyoda, D., Fukuda, M., Iwasaki, R. et al. The comparison between stroke volume variation and filling pressure as an estimate of right ventricular preload in patients undergoing renal transplantation. J Anesth 29, 40–46 (2015). https://doi.org/10.1007/s00540-014-1870-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-014-1870-2