Abstract
Background
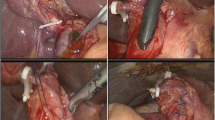
Laparoscopic common bile duct exploration (LCBDE) has gained wide popularity in the treatment of choledocholithiasis. Bile leakage remains a major cause of postoperative morbidity. The aim of this study was to report 5-year results of 500 LCBDEs and identify risk factors associated with bile leakage.
Methods
Five hundred consecutive LCBDEs performed in one institution from September 2011 to June 2016 were reviewed. Patients’ clinical data were retrospectively collected and analyzed. Univariable and multivariable analysis of bile leakage was performed by logistic regression.
Results
We found stones (n = 388) or bile sludge (n = 71) in 459 patients (92%) on exploration, leaving 41 patients (8%) without stones. Operative time was 128 min in the first 250 LCBDEs, and this decreased to 103 min in the second 250 LCBDEs (P = 0.0004). Four hundred and eight (82%) procedures were completed with primary closure after choledochotomy; the rate of primary closure increased significantly in the second 250 patients compared with the first (88 vs 76%; P = 0.0005), whereas T-tube placement (2 vs 6%; P = 0.0225) and transcystic approach (7 vs 12%; P = 0.0464) decreased, respectively. Stone clearance was successful in 495 patients (99%). Overall morbidity was 5%, and bile leakage occurred in 17 patients (3.4%). Two patients died from bile leakage. The median follow-up was 24 months with stone recurrence occurred in two patients and bile duct stricture in one patient. Univariable analysis identified diameter of the common bile duct (CBD), stone clearance, and T-tube insertion as risk factors related to bile leakage. Multivariable analysis taking these three factors into account identified non-dilated CBD (risk ratio (RR) = 9.87; P = 0.007) and failure in stone clearance (RR = 11.88; P = 0.024) as significant risk factors.
Conclusions
Bile leakage following LCBDE is associated with diameter of the CBD and stone clearance. LCBDE would be safer in proficient laparoscopic surgeons with a careful selection of patients.


Similar content being viewed by others
References
Aawsaj Y, Light D, Horgan L (2016) Laparoscopic common bile duct exploration: 15-year experience in a district general hospital. Surg Endosc 30:2563–2566
Khaled YS, Malde DJ, de Souza C, Kalia A, Ammori BJ (2013) Laparoscopic bile duct exploration via choledochotomy followed by primary duct closure is feasible and safe for the treatment of choledocholithiasis. Surg Endosc 27:4164–4170
Zhu HY, Xu M, Shen HJ, Yang C, Li F, Li KW, Shi WJ, Ji F (2015) A meta-analysis of single-stage versus two-stage management for concomitant gallstones and common bile duct stones. Clin Res Hepatol Gastroenterol 39:584–593
Kenny R, Richardson J, McGlone ER, Reddy M, Khan OA (2014) Laparoscopic common bile duct exploration versus pre or post-operative ERCP for common bile duct stones in patients undergoing cholecystectomy: Is there any difference? Int J Surg 12:989–993
Lauter DM, Froines EJ (2000) Laparoscopic common duct exploration in the management of choledocholithiasis. Am J Surg 179:372–374
Reinders JS, Gouma DJ, Ubbink DT, van Ramshorst B, Boerma D (2014) Transcystic or transductal stone extraction during single-stage treatment of choledochocystolithiasis: a systematic review. World J Surg 38:2403–2411
Berthou JC, Drouard F, Charbonneau P, Moussalier K (1998) Evaluation of laparoscopic management of common bile duct stones in 220 patients. Surg Endosc 12:16–22
Rhodes M, Sussman L, Cohen L, Lewis MP (1998) Randomised trial of laparoscopic exploration of common bile duct versus postoperative endoscopic retrograde cholangiography for common bile duct stones. Lancet 351:159–161
Yin Z, Xu K, Sun J, Zhang J, Xiao Z, Wang J, Niu H, Zhao Q, Lin S, Li Y (2013) Is the end of the T-tube drainage era in laparoscopic choledochotomy for common bile duct stones coming? A systematic review and meta-analysis. Ann Surg 257:54–66
Wu X, Yang Y, Dong P, Gu J, Lu J, Li M, Mu J, Wu W, Yang J, Zhang L, Ding Q, Liu Y (2012) Primary closure versus T-tube drainage in laparoscopic common bile duct exploration: a meta-analysis of randomized clinical trials. Langenbecks Arch Surg 397:909–916
Koch M, Garden OJ, Padbury R, Rahbari NN, Adam R, Capussotti L, Fan ST, Yokoyama Y, Crawford M, Makuuchi M, Christophi C, Banting S, Brooke-Smith M, Usatoff V, Nagino M, Maddern G, Hugh TJ, Vauthey JN, Greiq P, Rees M, Nimura Y, Fiqueras J, DeMatteo RP, Buchler MW, Weitz J (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Hua J, Lin S, Qian D, He Z, Zhang T, Song Z (2015) Primary closure and rate of bile leak following laparoscopic common bile duct exploration via choledochotomy. Dig Surg 32:1–8
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205–213
Zhang WJ, Xu GF, Wu GZ, Li JM, Dong ZT, Mo XD (2009) Laparoscopic exploration of common bile duct with primary closure versus T-tube drainage: a randomized clinical trial. J Surg Res 157:e1–e5
Zhu JG, Han W, Guo W, Su W, Bai ZG, Zhang ZT (2015) Learning curve and outcome of laparoscopic transcystic common bile duct exploration for choledocholithiasis. Br J Surg 102:1691–1697
Chen XM, Zhang Y, Gai HH, Sun DL, Liu SY, Duan YF, Yang C, Jiang Y, Wu HR (2013) Transcystic approach with micro-incision of the cystic duct and its confluence part in laparoscopic common bile duct exploration. J Laparoendosc Adv Surg Tech A 23:977–981
Hongjun H, Yong J, Baoqiang W (2015) Laparoscopic common bile duct exploration: choledochotomy versus transcystic approach? Surg Laparosc Endosc Percutaneous Tech 25:218–222
Lee HM, Min SK, Lee HK (2014) Long-term results of laparoscopic common bile duct exploration by choledochotomy for choledocholithiasis: 15-year experience from a single center. Ann Surg Treat Res 86:1–6
Noble H, Whitley E, Norton S, Thompson M (2011) A study of preoperative factors associated with a poor outcome following laparoscopic bile duct exploration. Surg Endosc 25:130–139
Burkhart RA, Relles D, Pineda DM, Gabale S, Sauter PK, Rosato EL, Koniaris LG, Lavu H, Kennedy EP, Yeo CJ, Winter JM (2013) Defining treatment and outcomes of hepaticojejunostomy failure following pancreaticoduodenectomy. J Gastrointest Surg 17:451–460
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Jie Hua, Hongbo Meng, Le Yao, Jian Gong, Bin Xu, Tingsong Yang, Wei Sun, Yuxiang Wang, Yukan Mao, Ti Zhang, Bo Zhou, and Zhenshun Song have no conflicts of interest or financial ties to disclose.
Rights and permissions
About this article
Cite this article
Hua, J., Meng, H., Yao, L. et al. Five hundred consecutive laparoscopic common bile duct explorations: 5-year experience at a single institution. Surg Endosc 31, 3581–3589 (2017). https://doi.org/10.1007/s00464-016-5388-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-016-5388-6