Abstract
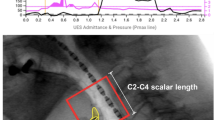
Automated impedance manometry (AIM) analysis measures swallow variables defining bolus timing, pressure, contractile vigour, and bolus presence, which are combined to derive a swallow risk index (SRI) correlating with aspiration. In a heterogeneous cohort of dysphagia patients, we assessed the impact of bolus volume and viscosity on AIM variables. We studied 40 patients (average age = 46 years). Swallowing of boluses was recorded with manometry, impedance, and videofluoroscopy. AIMplot software was used to derive functional variables: peak pressure (PeakP), pressure at nadir impedance (PNadImp), time from nadir impedance to peak pressure (TNadImp-PeakP), the interval of impedance drop in the distal pharynx (flow interval, FI), upper oesophageal sphincter (UES) relaxation interval (UES RI), nadir UES pressure (Nad UESP), UES intrabolus pressure (UES IBP), and UES resistance. The SRI was derived using the formula SRI = (FI * PNadImp)/(PeakP * (TNadImp-PeakP + 1)) * 100. A total of 173 liquid, 44 semisolid, and 33 solid boluses were analysed. The SRI was elevated in relation to aspiration. PeakP increased with volume. SRI was not significantly altered by bolus volume. PNadImp, UES IBP, and UES resistance increased with viscosity. SRI was lower with increased viscosity. In patients with dysphagia, the SRI is elevated in relation to aspiration, reduced by bolus viscosity, and not affected by bolus volume. These data provide evidence that pharyngeal AIM analysis may have clinical utility for assessing deglutitive aspiration risk to liquid boluses.


Similar content being viewed by others
Abbreviations
- NadUESP:
-
UES nadir relaxation pressure
- PAS:
-
Penetration–aspiration scale
- PeakP:
-
Peak pressure
- PNadImp:
-
Pressure at nadir impedance
- SRI:
-
Swallow risk index
- TNadImp-PeakP:
-
Time from nadir impedance to peak pressure
- UES IBP:
-
UES intrabolus pressure
- UES RI:
-
UES relaxation interval
- UES:
-
Upper oesophageal sphincter
References
Noll L, Rommel N, Davidson GP, Omari TI. Pharyngeal flow interval: a novel impedance-based parameter correlating with aspiration. Neurogastroenterol Motil. 2011;23(6):551–e206.
Omari TI, Dejaeger E, Van Beckevoort D, Goeleven A, Davidson GP, Dent J, Tack J, Rommel N. A method to objectively assess swallow function in adults with suspected aspiration. Gastroenterology. 2011;140:1454–63.
Omari TI, Dejaeger E, Van Beckevoort D, Goeleven A, De Cock, Hoffman I, Smet MH, Davidson G, Tack J, Rommel N. A novel method for the nonradiological assessment of ineffective swallowing. Am J Gastroenterol. 2011;106(10):1796–802.
Omari TI, Papathanasopoulos A, Dejaeger E, Wauters L, Scarpellini E, Vos R, Slootmaekers S, Seghers V, Cornelissen L, Goeleven A, Tack J, Rommel N. Reproducibility and agreement of pharyngeal automated impedance manometry with videofluoroscopy. Clin Gastroenterol Hepatol. 2011;9(10):862–7.
Butler SG, Stuart A, Castell D, Russell GB, Koch K, Kemp S. Effects of age, gender, bolus condition, viscosity, and volume on pharyngeal and upper esophageal sphincter pressure and temporal measurements during swallowing. J Speech Lang Hear Res. 2009;52(1):240–53.
Hoffman MR, Ciucci MR, Mielens JD, Jiang JJ, McCulloch TM. Pharyngeal swallow adaptations to bolus volume measured with high-resolution manometry. Laryngoscope. 2010;120(12):2367–73.
Pal A, Williams RB, Cook IJ, Brasseur JG. Intrabolus pressure gradient identifies pathological constriction in the upper esophageal sphincter during flow. Am J Physiol Gastrointest Liver Physiol. 2003;285:G1037–48.
Williams RB, Pal A, Brasseur JG, Cook IJ. Space-time pressure structure of pharyngo-esophageal segment during swallowing. Am J Physiol Gastrointest Liver Physiol. 2001;281:G1290–300.
Williams RB, Wallace KL, Ali GN, Cook IJ. Biomechanics of failed deglutitive upper esophageal sphincter relaxation in neurogenic dysphagia. Am J Physiol Gastrointest Liver Physiol. 2002;283(1):G16–26.
Williams RB, Grehan MJ, Hersch M, Andre J, Cook IJ. Biomechanics, diagnosis, and treatment outcome in inflammatory myopathy presenting as oropharyngeal dysphagia. Gut. 2003;52:471–8.
Ghosh SK, Pandolfino JE, Zhang Q, Jarosz A, Kahrilas PJ. Deglutitive upper esophageal sphincter relaxation: a study of 75 volunteer subjects using solid-state high resolution manometry. Am J Physiol Gastrointest Liver Physiol. 2006;291:525–31.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Bardan E, Kern M, Torrico S, Arndorfer RC, Massey BT, Shaker R. Radial asymmetry of the upper oesophageal sphincter pressure profile: fact or artefact. Neurogastroenterol Motil. 2006;18(6):418–24.
Acknowledgments
This study was supported by The Thrasher Research Fund, The National Health and Medical Research Council, and a Methusalem grant from Leuven University to Prof. J. Tack.
Conflict of interest
Dr. Omari has acted as a consultant to Sandhill Scientific Inc. E. Dejaeger, J. Tack, D. Van Beckevoort, and N. Rommel have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Omari, T.I., Dejaeger, E., Tack, J. et al. Effect of Bolus Volume and Viscosity on Pharyngeal Automated Impedance Manometry Variables Derived for Broad Dysphagia Patients. Dysphagia 28, 146–152 (2013). https://doi.org/10.1007/s00455-012-9423-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-012-9423-z