Abstract
Barker’s concept of ‘foetal programming’ proposes that intrauterine growth restriction (IUGR) predicts complex metabolic diseases through relationships that may be further modified by the postnatal environment. Dietary restriction and deficit in methyl donors, folate, vitamin B12, and choline are used as experimental conditions of foetal programming as they lead to IUGR and decreased birth weight. Overfeeding and deficit in methyl donors increase central fat mass and lead to a dramatic increase of plasma free fatty acids (FFA) in offspring. Conversely, supplementing the mothers under protein restriction with folic acid reverses metabolic and epigenomic phenotypes of offspring. High-fat diet or methyl donor deficiency (MDD) during pregnancy and lactation produce liver steatosis and myocardium hypertrophy that result from increased import of FFA and impaired fatty acid β-oxidation, respectively. The underlying molecular mechanisms show dysregulations related with similar decreased expression and activity of sirtuin 1 (SIRT1) and hyperacetylation of peroxisome proliferator-activated receptor-γ coactivator 1α (PGC-1α). High-fat diet and overfeeding impair AMPK-dependent phosphorylation of PGC-1α, while MDD decreases PGC-1α methylation through decreased expression of PRMT1 and cellular level of S-adenosyl methionine. The visceral manifestations of metabolic syndrome are under the influence of endoplasmic reticulum (ER) stress in overnourished animal models. These mechanisms should also deserve attention in the foetal programming effects of MDD since vitamin B12 influences ER stress through impaired SIRT1 deacetylation of HSF1. Taken together, similarities and synergies of high-fat diet and MDD suggest, therefore, considering their consecutive or contemporary influence in the mechanisms of complex metabolic diseases.
Similar content being viewed by others
Metabolic disorders linked to obesity represent a major health problem and a major part of the health costs worldwide. Obesity is a strong predictor of metabolic syndrome and insulin resistance. Insulin resistance is defined as inhibition of insulin stimulation of metabolic pathways, including lipid homeostasis. Both obesity (i.e. excess of adipose tissue) and ectopic fat deposition are closely associated with insulin resistance. The accumulation of excess lipids or their metabolites/derivatives (i.e. lipotoxicity hypothesis) in organs decreases insulin signalling and activate pro-inflammatory in liver, skeletal muscle and heart. On the other hand, insulin resistance is closely associated with dysregulation of fatty acid (FA) metabolism. The consequences of hepatic or cardiac steatosis are non-alcoholic fatty liver disease (NAFLD) and lipotoxic cardiomyopathy, respectively. How obesity promotes these visceral complications is not completely understood. The influence of excessive intake of macronutrients deserves much more attention than deficient intake of micronutrients in epidemiological and experimental studies, and the combined influence of global overnutrition and selective deficit in a category of micronutrient remains an open question. An increasing number of these studies have highlighted the influence of nutrients on the expression of genes regulating metabolism through a body of knowledge known as ‘nutrigenomics’.
As recently reviewed [48, 59], genetics, epigenetics, epigenomics and environment interact in defining the individual risk of obesity and related diseases. Epigenetics and epigenomics refer, respectively, to heritable and non-heritable (e.g. dependent from environment) changes of gene expression, which are caused by mechanisms such as DNA methylation, histone acetylation/methylation, dysregulation of gene transactivation and synthesis of miRNA. The influence of genetics is illustrated by the twofold to threefold increased disease risk in offspring from parents with obesity and type 2 diabetes mellitus (T2DM) in European populations [115]. Studies in twins undergoing overfeeding also suggest a strong influence of heritability [21]. Beside genetics, lifestyle and environmental factors clustered within families determine dietary preferences and food availability, two factors that may trigger epigenomic mechanisms. Barker’s concept of ‘foetal programming’ [10], also named developmental origins of health and disease, proposes that unfavourable intrauterine life, including intrauterine growth restriction (IUGR), predicts the risk of postnatal metabolic complex diseases through a relationship that may be further modified by the postnatal environment [179]. Environmental conditions of IUGR include nutritional stress such as protein and/or energy restriction [59, 88]. Recently, experimental and epidemiological studies have also highlighted the involvement of deficiencies in methyl donors during and after intrauterine life.
In this review, we will compare the epigenetic, epigenomic and nutrigenomic influences of three prevalent conditions of imbalanced intake of nutrients, overfeeding, dietary restriction (with a particular interest for proteins and amino acids) and deficit in methyl donors during pregnancy and early postnatal life and their consequences on the risk of obesity and related metabolic disorders in the liver and the heart. We will devote a specific interest for the mechanisms related to the influence of these imbalanced intakes on deregulation of FA metabolism.
The abnormal distribution and storage of fat influences the liver and heart complications of metabolic syndrome and insulin resistance
Obese individuals vary in their body fat distribution, their metabolic profile and the degree of associated cardiovascular and metabolic risks. As far as adipose tissue distribution is concerned, obesity consists of different subtypes or phenotypes with different metabolic profiles [141]. The mechanisms at the origin of the phenotype of metabolically healthy but obese subjects are poorly understood. Recent studies have confirmed that the combined phenotype of decreased lean body mass and central obesity reflects insulin resistance and indicates a high risk of diabetes mellitus [96] in Western and Asian countries. Metabolic syndrome related to central obesity may be viewed as ‘unhealthy obesity’ and the concerned individuals as metabolically abnormal obese patients [17, 140]. More recently, an acquired type of partial lipodystrophy closely linked with the severity of metabolic complications over a wide range of body mass index (BMI) values has been described in overweight adults, children, adolescents and elderly persons [162]. As described for the genetic type of partial lipodystrophy (e.g. Dunnigan syndrome), this phenotype is characterised by partial loss of peripheral fat and accumulation of fat in the trunk while the clinical presentation is less severe.
Many studies support the concept of a major role for intra-abdominal fat accumulation (visceral adipose tissue [VAT]) in the link between abdominal obesity and insulin resistance. Visceral hypertrophic adipocytes and VAT-resident macrophages produce pro-inflammatory cytokines like tumour necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6). VAT is also pathogenic because its venous blood drainage is direct via the portal vein to the liver. As a consequence of enlarged visceral adipocytes, the flux of free fatty acids (FFA) and pro-inflammatory cytokines contributes to hepatic insulin resistance and fat deposition in the liver (portal hypothesis of insulin resistance) [15, 92] and to NAFLD in obese patients [53]. FFAs promote insulin resistance by increasing hepatic glucose production. On the other hand, the production of pro-inflammatory cytokines by the VAT and circulating levels of IL-6 accelerate the subsequent transition to non-alcoholic steatohepatitis (NASH) and fibrosis [53]. Excess VAT could be also a surrogate marker of metabolic syndrome. The preferential accumulation of fat in the intra-abdominal cavity could be viewed as the consequence of an ectopic deposition [42]. According to this alternative hypothesis, increased visceral fat mass may represent a marker of the inability of patients with insulin-resistant obesity to store fat in subcutaneous adipose tissue (SAT). When the storage capacity of adipose tissue is exceeded, then a continuous exposure to FAs, not counterbalanced by FA oxidation, will lead to an accumulation of FFAs and induces a lipid ‘spill over’ to other tissues.
The impaired fatty acid oxidation is a major facet of the alterations of lipid metabolism in metabolic disorders related to obesity
FFAs meet all the criteria to be a metabolic factor related to insulin resistance in human subjects. Plasma FFA levels are elevated in most obese subjects and will inhibit the antilipolytic action of insulin, which will further increase FFAs release into the circulation [86]. Most studies have devoted attention to stressed adipose tissue releasing more FFAs, but a decreased rate of mitochondrial FA oxidation is another potential mechanism to be considered [127]. A substantial part of the insulin resistance-lowering activity of thiazolidinediones can be attributed to their lowering of plasma FFA levels through increasing FFA oxidation [18]. Several mechanisms grouped in the ‘lipid metabolite hypothesis’ have been proposed to explain how obesity and/or FFAs can interfere with insulin signalling. An increase in plasma FFA concentration results in intramyocellular and intrahepatic accumulation of triglycerides, long-chain acyl-CoAs and diacylglycerol (DAG) [18]. DAG is a potent activator of conventional and novel protein kinase C isoforms. In vivo, plasma FFA levels activate NF-κB in skeletal muscle and result in increased expression of pro-inflammatory cytokines, including TNF-α, IL-1β, IL-6 and MCP1. Possible mechanisms through which FFAs and the subsequent NF-κB activation and cytokine production can result in insulin resistance include activation of JNK by cytokines and induction of the suppressor of cytokine signalling, which can interfere with the binding of IRS1/2 to the insulin receptor [100, 101].
Influences of nutrition and metabolism on the epigenome: a facet of the mechanisms that may influence foetal programming and obesity
Foetal programming can produce heritable and non-heritable changes in adiposity through epigenetic and epigenomic mechanisms due to DNA methylation or histone modification of DNA in gene regulatory regions. The emerging level of evidence in human population studies contrasts with the number of arguments that sustain this hypothesis in experimental models [31].
DNA methylation by DNA (cytosine-5)-methyltransferases (DNMT) occurs at cytosine residues in CpG dinucleotides in vertebrates [140]. The methylated CG is symmetrically paired with the same sequence on the opposite DNA strand, which means that, after DNA replication, sites are transiently methylated in only one of the two strands. Although the pattern of 5-methylcytosines in the genome of differentiated somatic cells is quite stable, during early development, DNA methylation plays a critical role in the control of cell processes including embryonic development, transcription, X chromosome inactivation and genomic imprinting. Histone modifications influence DNA replication, repair and condensation and gene expression. The post-translational covalent modifications of histones include acetylation, methylation, phosphorylation and ubiquitination. The methylation and acetylation of histones are dynamic processes, which depend, respectively, on balances between histone methyltransferases (HMTs) and histone demethylases (HDMs) and between histone acetyltransferases and three classes of histone deacetylases (HDAC). The methylations and acetylations of histone residues obey to inter-histone and trans-histone regulatory pathways forming a ‘histone code’. Lysine methylation displays a high degree of complexity since each lysine residue can be mono-methylated, di-methylated or tri-methylated and each site of methylation can influence gene activity independently. Arginine residues can be mono-methylated or di-methylated symmetrically or asymmetrically [140].
Folate and vitamin B12 (cobalamins [Cbl]) are supposed to play a key role in epigenomic dysregulations of metabolism [64, 65]. These two nutritional methyl donors are needed for the endogenous synthesis of methionine by methionine synthase (MS). The homeostasis of methionine is crucial in cell life, since it is the amino acid required for the translation initiation and the immediate precursor of S-adenosyl methionine (SAM) [56]. They play a significant modulating role on DNA methylation through their influence on the cellular content of SAM, which is the universal methyl donor in transmethylation reactions [64, 65]. The cellular deficit in Cbl and Me-THF leads also to decreased synthesis of methionine and accumulation of homocysteine, which produces cellular stress by mechanisms largely documented in the literature [84, 177]. The role of SAM as methyl donor used by HMTs and DNMTs explains the influence of the deficiency in dietary methyl donors on histone and DNA methylation in rats [25, 132]. The importance of vitamin B12 and folate for maintaining an adequate cellular content of SAM is illustrated by the consequences of their deficiency on the cellular concentration of SAM, S-adenosyl homocysteine (SAH) and SAM/SAH ratio [61, 62]. The subsequent decreased SAM/SAH ratio impairs the cell capacity to ensure the transmethylation reactions of co-regulators of nuclear receptors (NRs), which play a key role in epigenetic and epigenomic mechanisms [65]
Beside dietary methyl donors, there are also nutrigenomic and epigenomic crosstalks between intermediate products of the metabolism of macronutrients and coenzymes derived from micronutrients [88]. The methylation and demethylation of DNA and histones depend on the cellular availability in coenzymes and substrates involved in energy metabolism and one-carbon metabolism (OCM). ATP is required for the synthesis of SAM. AMP-activated protein kinase (AMPK) senses nutrient deprivation through increased AMP levels, activating catabolic pathways to restore ATP levels and to increase mitochondrial biogenesis [33]. The macronutrient intake modifies the cellular content of nicotinamide dinucleotide (NAD+) and flavin adenine dinucleotide (FAD), which act as metabolic sensors of epigenomic regulations through demethylation and deacetylation of histones [165]. There are two types of HDMs, the LSD1-containing domain demethylases and the JumomjiC (JmjC) domain containing demethylases [165]. The LSD1-containing domain HDM is regulated by FAD, while the activity of JmjC-containing domain HDM depends on alpha-ketoglutarate, which is produced from glutamate in the Krebs cycle [169] and from the vitamin B6-dependent cystathionine γ-lyase in the transsulfuration pathway of homocysteine, in the OCM [65]. The loss of function of Jhdm2a is associated with reduced expression of peroxisome proliferator-activated receptor alpha (PPAR-α) and medium-chain acyl-CoA dehydrogenase [164]. NAD+ is required for activation of the class III sirtuin (SIRT) HDACs. The deacetylation of histones catalysed by SIRT leads to the cleavage of NAD+ into nicotinamide and 1-O-acetyl-ADP-ribose [34]. Butyrate, a short-chain carboxylic acid (C4) produced by bacterial flora and the intermediate metabolism of macronutrients and, to a lesser extent, acetate (C2), propionate (C3), valerate (C5) and caproate (C6), inhibits the HDAC of classes I and II [43].
DNA methylation changes during lifetime in function of environmental factors that include nutrition. This is illustrated by studies in humans and in distinct animal models, such as rodents and insects. The methylome of monozygotic twins becomes divergent with age [57]. Both restriction and overnutrition diets are related to changes in DNA methylation in the few epigenome-wide association studies that have investigated foetal programming-related risk for T2DM and obesity. In particular, the study of individuals who were prenatally exposed to famine during the Dutch Hunger Winter in 1944 has provided pertinent findings in favour of epigenomic mechanisms [74]: Six decades later, these individuals exhibited obesity associated with decreased DNA methylation of the imprinted IGF2 gene, as compared to the same-sex siblings without exposure to prenatal malnutrition. Individuals with periconceptional exposure to famine had lower methylation of the INSIGF gene and higher methylation levels for several other genes, including IL10, LEP and ABCA1 [167]. The hypocaloric diet increases methylation in three loci of DNA from SAT in overweight or obese postmenopausal women [22]. This diet also increases methylation at two loci in DNA from peripheral blood mononuclear cells in overweight or obese men [118]. Recently, a meta-analysis of genome-wide association studies has highlighted the rs7202116 at the FTO gene locus to be correlated with BMI [185]. A role for epigenomics was suggested by the influence of methylation of a CpG site in the first intron on the association of the FTO risk allele with BMI. However, the causality role of this methylation remains unclear [3, 13]. The FTO protein has a demethylase activity on N 6-methyladenosine of nuclear RNA, but whether this metabolic function is related to the observed effects on BMI remains an open question [87]. The leptin-responsive preproopiomelanocortin (POMC) gene is a hypothalamic regulator of energy balance. A hypermethylation variant targeting individual CpGs at the intron 2–exon 3 boundary of POMC is associated to obesity in children, in another case–control study. The hypermethylation of exon3 reduces the expression of POMC through reduced binding of the transcription enhancer P300 [99]. The dynamic effect of obesity on the epigenome is also illustrated by an altered promoter methylation of peroxisome proliferator-activated receptor-γ coactivator 1α (PGC-1α) and pyruvate dehydrogenase kinase isozyme 4 in skeletal muscle from adult obese subjects, which is restored to non-obese levels after weight loss induced by by-pass surgery [11]. In this study, the genome-wide DNA methylation analysis of skeletal muscle showed also that obesity is associated with hypermethylation at CpG shores and exonic regions close to transcription start sites [11]. Consistently, sedentary lifestyle and lack of physical activity may modify epigenetic programming and predisposition to obesity and T2DM, as recently reviewed [94]. In particular, they result in decreased expression of the mitochondrial and glucoregulatory genes PGC-1α, hexokinase 2 and ATP synthase subunit beta through epigenomic mechanisms that involve the activation of HDAC family members in skeletal muscle [94].
Epigenome-wide studies performed in insects and rodents under specific diets have also found changes in DNA methylation. An intriguing model is provided by honeybees. Fertile queens and sterile workers are alternative forms of the adult female honeybee that develop from genetically identical larvae following differential feeding with royal jelly, a mixture including proteins, sugars and FAs. Dnmt3 small interfering RNA-treated individuals emerged as queens with fully developed ovaries. DNA methylation by Dnmt3 triggers epigenetic information differentially altered by nutrition, with implications in development, reproduction and behavioural status of honeybees [55, 75, 98].
High-fat diet and foetal programming
The role of deacetylase sirtuin 1 and peroxisome proliferator-activated receptor-γ coactivator 1α in metabolic dysregulations
Maternal obesity and high-fat diet during pregnancy increase the risk of obesity in the offspring through complex mechanisms, which involve metabolic deregulation and alteration of food intake behaviour [82]. Paternal obesity has also to be considered. For example, paternal high-fat diet alters the expression of genes related to ATP binding and calcium-, MAPK- and Wnt-signalling pathways and to apoptosis and cell cycle in the pancreas of rat F1 female offspring. This suggests a role for epigenomic modifications of sperm produced by nutritional status, which continues after epigenetic reprogramming during the meiosis and first post-zygotic division [123].
Epidemiological studies have found an association between maternal overfeeding and chronic diseases in offspring, when they reach adulthood [174]. Worldwide prevalence of childhood obesity has increased greatly during the past three decades. The increasing occurrence of metabolic syndrome in children and adolescents and of type 2 diabetes in young adults is believed to be a consequence of this epidemic obesity. The pandemic obesity is largely related to easy access to energy-dense cheap foods and decreased energy requirements in daily life [175]. Sirtuin 1 (SIRT1), PGC-1α and the related downstream pathways play a major role in these deregulations [85, 146, 185]. The deacetylation of PGC-1α by SIRT1 increases, while its acetylation by general control non-derepressible 5 (GCN5) inhibits its activity [145]. High-fat feeding produces hyperacetylation of PGC-1α and a down-regulated expression of PGC-1α-dependent genes through increased expression of the two acetylases SRC-3 and GCN5 and decreased expression and activity of SIRT1 [32, 39]. These changes are consistent with the hyperacetylation of PGC-1α and the down-regulated expression of PGC-1α-dependent genes in mice lacking SRC-3 (Fig. 1) [39]. SIRT1 deacetylation also plays a key role in metabolic homeostasis through the regulation of the activity of Foxo transcription factors [26] and acetyl-CoA synthetases [70]. Consistently, the treatment of mice fed a high-fat diet with resveratrol and other SIRT1 agonists prevents weight gain and insulin resistance [100, 122].
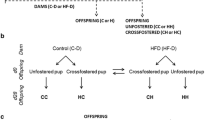
Comparison of the effects of high fat/overfeeding and MDD. PGC-1α is a master regulator of lipid metabolism and FA oxidation. It is phosphorylated and acetylated under the control of AMPK, GCN5 acetylase and SIRT1 deacetylase. High-fat diet and overnutrition decrease the activity of AMPK through high intracellular ATP levels, leading to decreased phosphorylation of PGC-1α. It produces hyperacetylation of PGC-1α through increased expression of GCN5 and decreased expression and activity of SIRT1. MDD in rat pups born from mothers subjected to MDD during pregnancy and lactation produces similar consequences on SIRT1 expression and PGC-1α acetylation in the heart. In addition, MDD decreases the expression of PRMT1 and the level of SAM, leading to decreased methylation of PGC-1α in the heart and liver
High-fat diet during pregnancy influences food intake behaviour in offsprings
Aberrant expression of genes that control the feeding behaviour may contribute to the development of obesity-related diseases. Maternal preference for macronutrient and energy intakes during pregnancy rather than paternal preference is associated with fat preference in the child [24]. The control of appetite and energy balance is regulated by peripheral signals, including glucose, leptin, insulin and gut hormones through their effects on hypothalamic neuropeptides mostly expressed in the arcuate nucleus. High-fat diet and/or maternal obesity increase neurogenesis and the production of hypothalamic neuropeptides that affect food intake, such as neuropeptide Y and POMC [36, 37, 124]. A recent experimental study performed with mice showed that maternal high-fat diet produces offsprings’ epigenetic marks with long-term alterations in expression of dopamine and opioids-related genes [173]. The neonatal overfeeding in rats also produces epigenomic DNA marks in the hypothalamus, with increased methylation of the promoters of POMC and insulin receptor [136, 137]. Leptin is another candidate, which is secreted almost exclusively by adipocytes and exerts a pivotal role in energy homeostasis and regulation of food intake. The high-fat diet produces changes of methylation at specific CpG sites within the leptin promoter, with consequences on circulating leptin levels [119]. Consequently, POMC is not up-regulated in these rats despite hyperinsulinaemia and hyperleptinaemia [136].
Consequences of high-fat diet during pregnancy on offspring’s liver
High-fat diet produces hepatic steatosis and NAFLD through complex mechanisms triggered by insulin resistance, which include the imbalance between uptake and de novo lipogenesis of non-esterified FAs and triglyceride, disposal by FA oxidation and secretion of triglyceride-rich lipoproteins [92]. The liver is subjected to epigenomic changes produced by high-fat diet during the in utero and postnatal periods, which participate in these mechanisms. In non-human primates, maternal high-fat diet during pregnancy increases H3K14 and H3K18 acetylation in offspring, with locus-specific effect on glutamic pyruvate transaminase 2 [1]. It increases the foetal H3K14ac, in relation with decreased SIRT1 expression and activity [159]. In rats, 2-day-old offspring of mothers fed a high-fat diet display hepatic cell cycle inhibition in relation with changes in DNA methylation and gene expression of the cyclin-dependent kinase inhibitor 1A [49], an alteration which may potentially contribute to NAFLD. Maternal high-fat diet impairs the activity of mitochondrial complexes I–IV and carnitine palmitoyltransferase 1A and up-regulates the hepatic lipogenesis in adult offspring. Consistently, high-fat diet during pregnancy and lactation alters hepatic expression of PPAR-α, insulin like growth factor-2 and microRNAs, including miR-122, miR-192, miR-194, miR-26a, let-7a, let7b and let-7c, miR-494 and miR-483, in adult offspring [186, 187]. High-fat feeding results in the up-regulation of miR-143 and down-regulation of miR-27a in mouse mesenteric adipose tissue through altered expression of PPARs [114]. High-fat diet produces also transgenerational and sex-dependent effects in mice. The male offspring of the F2 generation develop obesity and hepatic steatosis earlier and more severely than the F0 and F1 generations. The transgenerational changes in liver include enhanced lipogenesis and endoplasmic reticulum (ER) stress with increased expression of fatty acid synthase (FAS), SREBP, LXRα and β and ERO1-α. These effects play a key role in NAFLD and insulin resistance [52] and are related with epigenomic changes on histone methylations and reduced binding of methylated histones in LXRα and ERO1-α gene promoters [104].
Consequences of high-fat diet during pregnancy on offspring’s myocardium
Whether the deleterious effects of high-fat intake and caloric excess on the myocardium are independent from those related to the consequences of obesity and insulin resistance on endothelial dysfunction, hypertension and hyperlipidemia is a matter of debate in population studies and experimental models. The fat-enriched diet induces insulin resistance, inflammation and apoptosis, and these manifestations may also contribute to the cardiac hypertrophy. High-fat feeding of Wistar rats produces cardiac contractile dysfunction, which enhances CD36-mediated FA uptake and myocardium triacylglycerol accumulation [129]. Cardiac changes leading to cardiac lipotoxicity in rodents include mitochondrial dysfunction and impaired biogenesis, alteration of reactive oxygen species (ROS) production and increased lipid oxidation [188]. In obese Zucker rats, the high-fat ‘Western diet’ increases cardiac triglyceride content within a week, while long-term exposure promotes FA oxidation, which correlates with the prevention of further deterioration in cardiac function and triglyceride accumulation [30]. In response to high blood concentration of long-chain FAs, the heart is forced to increase FA uptake through increased expression of the FA transporter CD36, resulting ultimately to diabetic cardiomyopathy [45]. Then, this leads to the further increase of FAs and lipid intermediates such as DAG and ceramide and the increased production of ROS, with a profound impact on signalling pathways [45]. High-fat diet leads to glucose intolerance, elevated insulin plasma levels and reduced insulin-like growth factor 1 (IGF1) levels in mice. These changes may contribute to disrupting the phosphorylation of insulin receptor and post-receptor signalling molecules such as insulin receptor substrate 1 (tyrosine/serine phosphorylation), forkhead transcriptional factors and mTOR (target of rapamycin) [188].
PPARs play a master role in myocardium deregulations of FA uptake and mitochondrial β-oxidation [171, 176]. In particular, PPAR-α up-regulates the expression of FA transporters and induces the synthesis of metabolic enzymes of the β-oxidation pathway [171]. However, the role of the impaired expression PPAR-α in the metabolic effects of high-fat diet on the myocardium is questioned in part by the results obtained with KO mice. This animal model accumulates myocardial lipids through lower FA oxidation rate but does not produce high fat-induced insulin resistance, suggesting the contribution of other regulators [134, 177]. PPAR-γ seems to have a limited role in regulating cardiac metabolism, probably due to its low myocardial expression. Treatment of wild-type and PPAR-γ KO mice subjected to high-fat diet with PPARs agonists, rosiglitazone, fenofibrate and pioglitazone, indirectly protects the myocardium from lipid accumulation and lipotoxic damage by reducing FAs delivery to the heart. It also produces a shift of myocardial substrate utilisation towards greater contribution of glucose [9].
The influence of high-fat diet on PGC-1α down-regulation and the subsequent consequences in mitochondrial dysfunctions have also been proposed to play a major role in the mechanisms that relate obesity with heart failure [171]. High-fat diet-induced juvenile obesity leads to cardiomyocyte dysfunction, up-regulates the forkhead transcription factor Foxo3a and suppresses mitochondrial aconitase activity without affecting the expression of SIRT1 [143]. However, SIRT1 seems to play an adaptive role since the myocardium stimulation of SIRT1 extends the life span of mice fed a high-fat diet and retards aging in the heart [183, 184]. Another deacetylase, HDAC3, may contribute to the epigenomic mechanisms underlying the deleterious influence of high-fat diet on the myocardium [158]. Embryonic deletion of myocardial Hdac3 in mice causes a major cardiomyopathy that reduces survival. When excision of Hdac3 in the heart is produced during late development, the switch to a high-fat diet leads to severe hypertrophic cardiomyopathy and heart failure, with down-regulation of myocardial mitochondrial genes, specifically those involved in lipid metabolism, suggesting that HDAC3 is important in maintaining proper mitochondrial function [158].
Protein restriction and foetal programming
The Dutch Hunger Winter of 1944 has provided a well-characterised population adapted for studying the relations between food restriction and foetal programming in humans. In the related Dutch cohort, pregnant mothers and foetuses have experienced malnutrition during the first, second or third trimesters of pregnancy. The mother’s food rations were known and the follow-up medical histories of foetuses could be collected in national population registers. This has permitted highlighting the associations between food restriction, IUGR and increased risks of metabolic syndrome, diabetes and cardiovascular diseases [110, 147, 148] and studying the epigenomic changes related to these associations [167]. Beside these population studies, animal models of food and protein restriction have been used to dissect the molecular mechanisms, which underlie the association between foetal growth retardation and metabolic and visceral consequences. In rodents, protein restriction during pregnancy and lactation results in reduced pancreatic β cell mass at birth and reduced insulin secretion in later life [44, 135, 163]. The transcriptional alterations induced by protein restriction during pregnancy rely mainly on transient transcription factor-dependent deregulations, with strong specific transcriptional changes in foetal tissue that cluster the liver with the heart [170]. The vast majority of studies have compared the 20–18 % casein diet (control situation) to 10–8 % casein diet. Methionine content is low in casein diets, and these experimental protocols raise the question of limiting the intake of methionine, which is insufficiently considered.
Dietary protein restriction in insect and rodent models has uncovered a likely role for key nutrient sensors, including mTOR, IGF1, insulin, AMPK, SIRT1 [152] and PGC-1α [51]. The effects of dietary restriction on PGC-1α regulation mirror those of the high-fat diet. Decreased acetylation of PGC-1α results from decreased expression of the two acetylases SRC-3 and GCN5 and increased expression of SIRT1 [32, 39]. The royal jelly diet induces queen bee differentiation through the influence of mTOR and IGF1/insulin pathways, with consequences on DNA methylation [125].
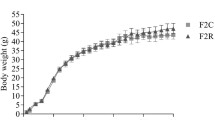
Protein or calorie restriction during pregnancy favours hyperphagia in offspring
The protein or calorie restriction during gestation and/or suckling of rodents produces hyperphagia. Low-protein diet throughout pregnancy and lactation reduces the anorexic effects of serotonin (5-HT) in malnourished rats through a desensitisation of 5-HT(1B) receptors. Pups born from protein-restricted dams and treated with dl-fenfluramine exhibit hyperphagia, at least partially related to a reduced regulatory function of 5-HT [108]. The hypothalamus is one of the brain areas affected by the programming effect of protein restriction. Perinatal protein restriction permanently alters the expression of two gene clusters, the first one regulating insulin signalling and nutrient sensing and the second a functional network of NRs and co-regulators of transcription involved in the use of lipids as fuel and in metabolic regulation by the circadian clock [128]. Consistently, giving the restricted diet at the same time each day changes the daily profiles of PERIOD1 and PERIOD2 protein expression in the brain nucleus of rats [172]. Mice born to mothers fed a low-protein diet have lower body weight and adiposity and higher food intake than animals born to mothers fed a control diet. These modifications persist throughout life and are associated with methylation changes in leptin gene, as observed in rats subjected to high-fat diet. This nutritional stress results in lesser methylation of CpGs located in the promoter of leptin, causing a permanent modification in the dynamics of leptin expression, with stronger induction in response to a meal [90]. The low-protein diet in pregnant rats may have subsequent effects on feeding behaviour of offspring through alteration in the expression level of the genes encoding Dnmt1 and Dnmt3a and in methylation status of promoters of genes encoding orexigenic and anorexigenic hypothalamic neuropeptides, including neuropeptide Y, proopiomelanocortin and leptin [41].
Consequences of calorie or protein restriction during pregnancy on offspring’s liver
Caloric restriction causes epigenetic and epigenomic changes that contribute to an increased risk of insulin resistance and NAFLD. It produces changes in acetylation and methylation of histones and hypomethylation of gene promoters with consequences that include reduced expression of the GLUT4 glucose transporter in rat skeletal muscle [142] and it increases foetal liver phosphoenolpyruvate carboxykinase (PEPCK) in primate [126]. The increased expression and activity of PEPCK in the liver promote gluconeogenesis and, consequently, the induction of insulin resistance. In contrast, hepatic PEPCK activity is reduced in female offspring of dams fed a protein restriction diet [143]
The effects of caloric restriction are targeted by deacetylases [155]. Low birth weight foetuses from pregnant dams fed a restricted diet have an increased prenatal hepatic SIRT1 activity. Low birth weight newborn offspring undergo postnatal suppression of hepatic SIRT1 and AMPK activities in conjunction with increased lipogenesis, decreased lipolysis and increased fat stores [180]. Moreover, transgenic mice overexpressing Sirt1 exhibit metabolic and physiological effects mimicking those induced by dietary restriction [8]. Moderate energy restriction seems to produce distinct results influenced by sex, with lower hepatic expression of SIRT1, sterol response element binding protein 1c (SREBP1c) and stearoyl-CoA desaturase-1 in males and unchanged levels in females, compared to controls [130]. SIRT3 is also a prominent regulator of the mitochondrial adaptation to caloric restriction by coordinately deacetylating proteins involved in mitochondrial maintenance [73]. SIRT6 is significantly decreased following dietary restriction, and this may contribute to the increased acetylation at lysine residue 9, 27 and 56 in H3 [91].
The low-protein diet in maternal rats produces epigenomic hallmarks of NAFLD in foetuses and offsprings [144]. However, the deregulation of imprinting through a general effect on the methylation of differentially methylated regions (DMRs) is unlikely to be involved in developmental programming. Indeed, although expression of some imprinted genes in the liver of offspring is sustainably changed, the methylation of DMRs that control their monoallelic expression remains largely unaltered [83]. Protein restriction during pregnancy induces hypomethylation of PPAR-α and glucocorticoid receptor (GR) promoters and increases expression of GR and PPAR-α in liver of juvenile and day 80 adult offspring [27, 29, 106]. The altered expression of GR, PPAR-α and hepatic nuclear factor 4 (HNF-4) deregulates lipid oxidative metabolism and promotes liver steatosis and insulin resistance. These alterations have an epigenetic characteristic with transmission to future generations [29]. Protein restriction alters the epigenetic regulation of GR through reduced Dnmt1 expression in the offsprings [107]. Other changes include hypomethylation of specific cytosines in the PPAR-α promoter and in offspring’s liver [107] and repressive changes in histone modifications at the cholesterol 7alpha-hydroxylase promoter through decreased hepatic expression of Jmjd2a demethylase in foetal liver [154]. Transgenerational effects of protein restriction have been studied in rats and mice. Offspring from protein-restricted F0 rats show altered fasting glucose homeostasis and changes in PEPCK promoter methylation and expression in the three F0, F2 and F3 generations [79]. The protein restriction in F0 produces also a lower promoter methylation of PPAR-α and GR in the liver from F1 and F2 generations [27]. Similarly to what has been observed on high-fat models, the father’s restriction diet may also produce transgenerational effects, with elevated hepatic expression of genes involved in lipid and cholesterol biosynthesis in offspring. Epigenomic profiling of offspring livers revealed changes in cytosine methylation depending on paternal diet, including changes in methylation over a likely enhancer for PPAR-α [35].
Consequences of caloric or protein restriction during pregnancy on offspring’s myocardium
In contrast to the deleterious effects of high-fat intake and overnutrition, long-term caloric restriction leads to decreased cardiac triglyceride content in obese type 2 diabetic subjects [53, 71] and protects healthy individuals against age-associated decline in diastolic function [117]. However, little is known about the long-term effects of the intrauterine exposure to protein and/or caloric restriction in population studies and, in particular, the molecular and metabolic changes in the myocardium [54, 151]. Long-term caloric restriction decreases left ventricular wall thickness and cardiomyocyte cell length and increases cardiac autophagy in C57BL/6 mice. At the molecular level, it increases the phosphorylation of Akt/glycogen synthase kinase-3β and AMPK/acetyl-CoA carboxylase [72]. Long-term caloric restriction of mice reduces triglyceride content in the heart, with a more dynamic pool in females than in males [7]. It maintains mitochondrial protein synthesis in the heart and skeletal muscle, an observation, which is consistent with an increased somatic maintenance [120]. In contrast, long-term caloric restriction of mice decreases ubiquinone Q9 and COQ transcript levels in heart [131].
Food and protein restriction deregulates fat and energy metabolism in the heart of pregnant rat. The methylation of PPAR-α promoter is decreased and mRNA expression of PPAR-α and carnitine palmitoyltransferase-1 is increased by maternal protein restriction diet in adult, but not in neonatal offspring [153]. Maternal protein restriction of rats during gestation increases the myocardial expression and deposition of collagens in day 70 offspring, compared to controls, in relation with changes in the expression patterns of pro-fibrotic genes and discrete structural abnormalities of heart [116].
Consequences of amino acid restriction during pregnancy
Beside the large number of studies devoted to the foetal programming effects of protein restriction, a lesser attention has been paid to the global or specific deficit in amino acids. Amino acid homeostasis depends on dietary intake of proteins and on the endogenous turnover of protein synthesis and degradation. Part of the mechanisms of foetal programming related to protein restriction may be, therefore, related to this altered homeostasis. Some of them may be explained by specific functions of amino acids [60]. For example, 5-HT is needed for the biosynthesis of tryptophan and glutamate is a neurotransmitter. The deficit in amino acids may also produce consequences through their role as intermediate substrates in many pathways of metabolism as exemplified by the role of methionine, glycine and serine in the OCM [65] and the role of alanine in neoglucogenesis [60].
Interestingly, tryptophan and methionine are the two least abundant essential amino acids in casein, the protein commonly used in the protein restriction diets used in experiments with rodents. Thus, the regimens using casein as the sole source of protein could produce effects related to inadequate intake of these two amino acids, including reduced adiposity, extended maximal longevity, increased resistance to acetaminophen toxicity in the liver and reduced insulin, IGF1 and thyroid hormone levels [121]. Methionine restriction contributes to adiposity resistance by altering the lipogenic/lipolytic balance [133], while leucine deprivation improves insulin sensitivity [180].
Two signal transduction mechanisms are involved in sensing intracellular deficit in amino acids [60]. GCN2 senses the absence of many amino acids, while the TOR pathway senses the presence of branched amino acids (leucine, isoleucine and valine), arginine and glutamine. Both repress general translation through distinct mechanisms. The signal-transducing kinase GCN2 binds to uncharged tRNAs, resulting in kinase activation and phosphorylation of eIF2α in the brain and liver, which leads to slow down translation of most mRNAs and to favour the translation of mRNAs containing specific regulatory elements in their 5′-untranslated regions [60]. TOR is a serine/threonine kinase that controls cell proliferation in response to adequate energy, nutrients and growth factors. The activation of TOR does not involve its binding to amino acids or surrogates such as tRNAs. Rag family of small GTPases is required for amino acid sensing by mTORC1 [60].
Part of the effects of protein restriction diet on food intake could be explained by the influence of amino acid deprivation in the brain. Leucine reduces food intake through activation of mTOR in the hypothalamus [40]; mTORC1 activation by amino acid restriction also results in changes in metabolic pathways such as the stimulation of glycolysis, pentose phosphate pathway and de novo lipid biosynthesis through the activation of hypoxia-inducible factor-1α, SREBP1 and SREBP2 [50]. Aversion to food intake can be produced by diets lacking essential amino acids through activation of GCN2 in anterior piriform cortex [63]. GCN2 can also influence fat metabolism. Expression of lipogenic genes and activity of FAS in the liver are repressed and lipid stores in adipose tissue are mobilised upon leucine deprivation in mice. In contrast, GCN2-deficient mice develop liver steatosis and exhibit reduced lipid mobilisation [69]. Leucine deprivation improves hepatic insulin sensitivity by sequentially activating GCN2 and decreasing mTOR/S6K1 signalling and by activating AMPK [180].
Methyl donors, foetal programming and manifestations of metabolic syndrome
Methyl donors could play a modulating role in complex metabolic diseases, according to epidemiological and experimental data. Deficiencies in folate and vitamin B12, and to a lesser extent in choline, are common during the gestational period in Western countries. The animal models with methyl donor deficiency (MDD) have a small birth weight and undergo altered expression of key regulators of metabolism and obesity-related diseases, such as SIRT1, PGC-1α and Mir-124 [2, 34, 65, 93]. Methyl donors play an essential role in the epigenetic and epigenomic mechanisms (methylation, acetylation) that influence gene expression and cell signalling. They produce IUGR with long-lasting consequences during development and throughout life [46, 65]. In this context, it is noteworthy to note that experimental cellular and animal models of MDD produce molecular hallmarks similar than those associated with overfeeding and obesity, such as decreased expression of SIRT1 and inactivation of PGC-1α through imbalanced acetylation/methylation (Fig. 1).
Methyl donors and foetal programming: the population-based studies
Recent large epidemiological studies have shown that vitamin B12 deficit during pregnancy is the most powerful micronutrient predictor for the risk of small birth weight and subsequent events related to foetal programming, including metabolic syndrome and insulin resistance. In contrast, the influence of folate status during pregnancy on foetal programming manifestations is less consistent. In India, babies are thin but fat, compared to Europe [182] and the high prevalence of mothers with low serum vitamin B12 is associated with IUGR. In a rural area from South India, the most insulin resistant children were born to mothers who had the lowest serum vitamin B12 and the highest erythrocyte folate concentrations [181]. Low maternal vitamin B12 blood level in early pregnancy predicts an elevated risk of insulin resistance, while folic acid maternal supplementation has a weak protective effect on incidence of metabolic syndrome, in school-aged offsprings from rural Nepal [156]. Population studies focused on the influence of folate in foetal programming have also produced contrasted results in Western countries. Antenatal supplementation with folic acid increases birth weight, while high homocysteine and low folate concentrations in early pregnancy are associated with both low placental and birth weights, and higher risk of adverse pregnancy outcomes, in the Netherlands [14, 166]. Folate intake estimated by questionnaire does not influence childhood body composition, in a cohort from South UK [103], while it is associated with birth weight and insulin resistance in French obese adolescents [58]. Methylenetetrahydrofolate reductase (MTHFR) 677 C > T polymorphism is not associated with obesity, BMI or metabolic syndrome in three cohorts from UK, Danemark and Italy [102, 149]. In contrast, in France, this polymorphism was associated with low birth weight and high insulin resistance in morbidly obese adolescents [58].
Several studies suggest that these associations could involve epigenomic mechanisms [157]. A variant of adenosyl-methionine decarboxylase is associated with childhood obesity, in India [161]. Studies conducted in Gambia, have found changes in methylation of metastable epi-alleles [177] when comparing birth exposure to seasonal variations of food-consumption patterns, which produce also significant changes in methyl-donor biomarkers [47].
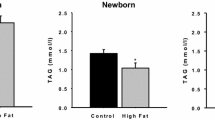
Consequences of methyl donor deficiency on birth weight, food intake and digestive mucosa
The mother-progeny rat model of deficiency in folate, vitamin B12 and choline contributes to understand the complex links between metabolic syndrome and birth weight, according to the foetal programming hypothesis [16, 61, 89, 139]. MDD produces a dramatic injury of digestive mucosa that may participate to the pathomechanisms of IUGR, small birth weight and abnormal food intake, but little is known on its effects on food intake [20]. Ghrelin is a gastric peptide involved in foetal growth through its dual role as growth hormone-releasing factor and appetite stimulating peptide [95]. MDD affects gastric cell organisation and impairs the release of ghrelin in blood [20]. It also produces an over-expression of Cox-2, PLA2 and TNF-α pro-inflammatory pathways in gastric and intestine mucosa and alters mucosal differentiation and function in rat pups from dams subjected to deficiency during gestation and lactation [23, 78].
The link between the one-carbon metabolism and non-alcoholic fatty liver disease
Vitamin B12, folate, homocysteine and genetic determinants of the OCM are associated with NAFLD severity in operated and non-operated obese subjects [68, 77, 97]. Hepatic steatosis is also observed in patients with genetic disorders of OCM [38, 150]
A restriction of the periconceptional diet in cobalt and sulphur in sheep produces low vitamin B12 and methionine and leads to heavier and fatter adult offspring, with insulin resistance and elevated blood pressure that are most obvious in males. The altered methylation status of CpG islands examined by restriction landmark genome scanning in the foetal liver revealed that more than half of the affected loci are specific to males [152]. The normal mitochondrial proteome function relies on the maintenance of methylation in rodents [5]. Impaired mitochondrial metabolism has been reported in genetically altered mice exhibiting SAM deficiency in the liver [112], suggesting that SAM plays a critical role in maintaining proper mitochondrial function. Consistently, supplementation with methyl donors and SAM at concentrations that maintain methylation reactions preserves mitochondrial proteome as well as prevents ethanol-dependent defects in mitochondrial respiration [4, 6, 160]
In the mother–progeny rat model of MDD, fatty liver and fatty heart can be regarded as two early predisposing manifestation of metabolic syndrome through deregulation of lipid fuel homeostasis and mitochondrial metabolism [91, 139]. The deficiency yields microvesicular liver steatosis in pups [16]. The steatosis results from a deficit in carnitine synthesis and epigenomic deregulations, with hypomethylation and decreased expression of PPAR-α, oestrogen-related receptor alpha (ERR-α), ER-α and liver-specific NR HNF-4α and hypomethylation of PGC-1α coactivator through decreased activity of arginine methyltransferase 1 (PRMT1) [139]. The hypomethylation of PGC-1α in the liver participates in the epigenomic deregulation of FA β-oxidation by reducing its partnership with PPAR-α, ERR-α and HNF-4α (Fig. 2) [61, 139]. Consistently, other data show that the lack of PPAR-α enhances steatohepatitis and that the PPAR-α agonist has the opposite effect in mice fed a methionine- and choline-deficient diet [109]. Mice fed a methionine- and choline-deficient diet develop steatohepatitis, with an inflammatory infiltrate prominent in the hepatic acinar zone [178]. Feeding mice a choline- and folate-deficient diet for 12 weeks causes NAFLD with a down-regulation of PPAR-α-regulated lipid catabolic pathway genes [168]. These results have to be considered in regard to the central role of mitochondrial dysfunction in insulin resistance [109]. MDD produces a decreased expression of SIRT1 [136], which is also observed in high-fat diet [81]. Male inbred C57BL/6J and DBA/2J mice fed a methyl-deficient diet develop liver injury similar to NASH. The livers of DBA/2J mice had initially a lower degree of methylation of repetitive elements and lower extent of histone H3 lysine 9 (H3K9) and H3 lysine 27 (H3K27) trimethylation, compared to those in the C57BL/6J mice. They developed subsequently more prominent NASH-specific pathomorphological changes [138].
The molecular links between MDD and impaired FA oxidation. The deficiency in folate and vitamin B12 of the rat ‘dam–progeny’ model impairs FA oxidation and complexes I and II of the mitochondrion respiratory chain through decreased expression of PPAR-α, ERR-α and HNF-4. It impairs the co-regulation of these NRs by PGC-1α through its decreased methylation and/or increased acetylation. This imbalanced methylation/acetylation is the consequence of the decreased expression of arginine methyltransferase PRMT1, the decreased cellular ration of SAM/SAH ratio (which directly influence PRMT1 activity as substrate and inhibitor, respectively) and the decreased expression of deacetylase SIRT1 (adapted from refs. [61, 63, 68])
Consequences of MDD on the heart
MDD during pregnancy and lactation of rodents induces heart hypertrophy, with impaired mitochondrial FA oxidation and decreased activity of complex I and II of the respiratory chain in rat pups [61]. The role of the deficiency in producing myocardium hypertrophy has been ascertained by a significant correlation of heart/body weight with folate, vitamin B12 and Hcy. The diet produces a decreased concentration of folate, a decreased SAM/SAH ratio and an increased immunohistochemical detection of Hcy in the myocardium of the deficient animals. The decreased SAM/SAH ratio is the consequence of a trap whereby the impaired remethylation pathway and the absence of cystathionine-β-synthase produced a conversion of homocysteine into SAH by the reversible enzyme SAH hydrolase [61]. The proteomic analysis of the myocardium of pups from rat dams fed a methyl donor-deficient diet shows altered abundance of proteins associated with developmental disorder, cellular compromise and lipid metabolism [111]. Concurrently, increased protein carbonylation, the major oxidative post-translational protein modification, could contribute to the decreased abundance of many myocardial proteins [111]. The main proteomic changes are observed for proteins regulated by PGC-1α, PPARs and ERR-α. These proteins, namely, trifunctional enzyme subunit α-complex, short-chain acyl-CoA dehydrogenase, acyl-CoA thioesterase 2, fatty acid-binding protein-3, NADH dehydrogenase (ubiquinone) flavoprotein 2, NADH dehydrogenase (ubiquinone) 1α-subunit 10 and Hspd1 protein, are involved in FA oxidation and mitochondrial respiration. These changes are related to the decreased expression of PPAR-α and ERR-α and to the hypomethylation and hyperacetylation of PGC-1α through decreased expression and activity of PRMT1 and SIRT1 and decreased SAM/SAH ratio (Fig. 2). It is noticeable that the decreased expression of SIRT1 is also a molecular hallmark of overnutrition (Fig. 1) [19, 32, 51, 61, 80].
Folate- and vitamin B12-dependent pathways are needed for the proper foetal development of the heart. Indeed, the c.56 + 781 A > C (rs326119) variant of intron 1 of MS reductase results in functionally reduced gene transcription and significantly increases the risk of congenital heart disease in the Han Chinese population [188]. The link between the OCM, cardiomyopathies and impaired mitochondrial FA oxidation has been confirmed in two contrasting populations, patients undergoing coronarography and ambulatory elderly subjects [67]. Folate deficit was more frequent in the coronarography population than in the elderly ambulatory volunteers and produced a higher concentration of homocysteine. Homocysteine and NT-pro-BNP were positively correlated with short-chain, medium-chain and long-chain acylcarnitines and with acylcarnitine ratios indicative of decreased mitochondrial acyldehydrogenase activities. This can contribute to explaining the association of homocysteine with left ventricular mass and left ventricular systolic dysfunction [66, 76].
Comparison of the tissue, metabolic, genomic and epigenomic effects of high fat/overfeeding, protein/caloric restriction and methyl donor deficiency
The pups deprived of methyl donors had a decreased birth weight and no change in insulin concentration, as observed in the protein restriction and food restriction rat models of foetal programming [24–26]. However, comparing the heart and liver manifestations in the three diets and the underlying molecular mechanisms shows intriguing similarities between high fat/overfeeding and MDD. The methyl donor-deficient rats have a dramatic increase of plasma FFA, which is similar to that observed in high-fat diet animals and contrasts to the mild increased level reported in pups under protein and/or food restriction [24–26]. MDD produces a cardiac hypertrophy with myocardium FA accumulation, a phenotype, which is due to impaired FA β-oxidation and possibly to an increased import of FFA from plasma.
Intriguingly, the deficit in methyl donors may produce a central lipodystrophy, with similar molecular hallmarks than those observed following overfeeding and high-fat diet. These data and epidemiological data on the methyl donor status of mothers during pregnancy suggest considering with particular interest the effects of MDD during pregnancy and overnutrition in later life as part of the explanation of the links between foetal programming and metabolic disorders related to obesity. It is noteworthy that several studies on cell and experimental models found a strong imbalance in energy metabolism similar to that observed in metabolic syndrome, with molecular hallmarks similar to those produced by nutrition overload and obesity, including the decreased expression and activity of SIRT1, the related hyperacetylation of PGC-1α and the subsequent disruption of mitochondrial energy metabolism [65]. High-fat diet and overfeeding impairs the AMPK-dependent phosphorylation of PGC-1α, a change to be documented in MDD. AMPK is a key metabolic sensor, which behaves as a control switch to maintain metabolic homeostasis in function of energy supply. It is decreased by calorie restriction and increased by overfeeding, with a mirrored influence that depends on the cellular level of ATP and on AMP/ATP ratio (Fig. 1). The expression and influence of AMPK in MDD needs to be better evaluated, considering the possible inhibitory effect of SAM on its activity [113]. PP2A, one of the four major classes of eukaryotic serine/threonine phosphoprotein phosphatases, is also a metabolic sensor to be considered, since it is activated by methylation and up-regulated by vitamin B12 deficiency [12]. The visceral manifestations of metabolic syndrome and insulin resistance are under the influence of ER stress in overnourished animal models [52]. These mechanisms should also deserve attention in the foetal programming effects of MDD since vitamin B12 influences ER stress through impaired SIRT1 deacetylation of heat shock factor protein 1 (HSF1) (Fig. 3) [62].
Influence of vitamin B12 on cell proliferation through SIRT1-dependent activation of ER stress. The decreased cellular availability in B12 activates ER stress pathways and apoptosis by hyperacetylation of HSF1 through decreased expression of SIRT1. The dramatic reduction in both protein expression and acetylation of HSF1 leads to critical reduction of the molecular chaperons needed for a functional proteome in normal cellular growth. In contrast, B12 supplementation protects the cells from the activation of ER stress and apoptosis in cells subjected to thapsigargin, an ER stress inducer. Thus, B12 will favour fully adapted unfolded protein response (UPR) against any downstream attacks in non-deficient cells, while in deficient cells, activated UPR will likely be shifted from adaptive toward apoptotic maladaptive end point. SIRT1 sirtuin (silent mating type information regulation 2 homolog) 1, HSF1 heat shock factor protein 1
The mirrored influence of MDD and protein restriction on heart and liver manifestations of foetal programming is consistent with the reversal of the metabolic and epigenomic phenotype induced by maternal nutritional restriction when supplementing the mothers with folic acid, in rats [28]. Intriguingly, giving folate supplementation during the juvenile–pubertal period of offspring produced opposite results, with hepatosteatosis, impaired liver FA β-oxidation and decreased liver expression of PPAR-α through promoter hypermethylation [28, 105]. As highlighted by Burdge et al., these findings may reflect the fact that puberty is one of the four periods of increased instability of the epigenome [28]. Giving a high-fat diet to pups from mother fed a protein-restricted diet after weaning exacerbates their obesity [145]. Similar studies should be performed to test the consecutive or contemporary influence of MDD and high-fat diet, in regard to the potential synergic effects of the two diets at the tissue, metabolic and genomic levels.
Conclusion
A limited number of population studies have evaluated the metabolic, epigenomic and genomic effects of foetal programming on liver and heart manifestations. This probably reflects the difficulty to design follow-up and interventional studies adapted to the tested hypotheses, despite the remarkable experimental attention, which has been given to animal models and, particularly, rodents. In contrast to overfeeding and MDD, protein and/or food restriction does not assess a situation, which reproduces the more frequent causes of abnormal nutritional status of mothers during pregnancy and lactation, at least in Western countries. High-fat intake/overfeeding and MDD are two situations, which are frequent during pregnancy, in adolescents and in elderly subjects, in countries, which are not subjected to folate fortification. Their consecutive and/or contemporary influence during pregnancy and later life should be, therefore, investigated in population studies and experimental animal models.
In the liver and heart, experimental consequences include increased influx and storage produced by overfeeding/high fat and impaired FA β-oxidation by MDD. Beside the influence of high fat and overfeeding on insulin resistance and metabolic syndrome, several large epidemiological studies have shown that vitamin B12 deficit during pregnancy is a powerful predictor for the risk of small birth weight, lipodystrophy, metabolic syndrome and insulin resistance in India and Nepal. Paradoxically, its effects are more important in newborns and children from mothers supplemented with folate. Meanwhile, experimental data have shown that the deficiency in Cbl and folate produces central fat accumulation and epigenomic dysregulations, which lead to ER stress and disruption of mitochondrial energy metabolism. Whether methyl donor status and the related dysregulations are involved in the pathomechanisms of metabolic syndrome and insulin resistance in humans needs further attention using integrative genomics, proteomics and metabolomics approaches.
Abbreviations
- AMPK:
-
AMP-activated protein kinase
- Cbl:
-
Cobalamin
- DAG:
-
Diacylglycerol
- DMR:
-
Differentially methylated region
- DNMT:
-
DNA (cytosine-5)-methyltransferase
- ERR-α:
-
Oestrogen-related receptor alpha
- FA:
-
Fatty acid
- FAD:
-
Flavin adenine dinucleotide
- FFA:
-
Free fatty acids
- GCN5:
-
General control non-derepressible 5
- GR:
-
Glucocorticoid receptor
- HSF1:
-
Heat shock factor protein 1
- HDAC:
-
Histone deacetylase
- HDM:
-
Histone demethylase
- HMT:
-
Histone methyltransferase
- IGF1:
-
Insulin-like growth factor 1
- IL-6:
-
Interleukin-6
- IUGR:
-
Intrauterine growth restriction
- MS:
-
Methionine synthase
- MTHFR:
-
Methylenetetrahydrofolate reductase
- MDD:
-
Methyl donor deficiency
- mTOR:
-
Target of rapamycin
- NAD+ :
-
Nicotinamide dinucleotide
- NAFLD:
-
Non-alcoholic fatty liver disease
- NASH:
-
Non-alcoholic steatohepatitis
- OCM:
-
One-carbon metabolism
- PPAR-α:
-
Peroxisome proliferator-activated receptor alpha
- PGC-1α:
-
Peroxisome proliferator-activated receptor-γ coactivator 1α
- POMC:
-
Preproopiomelanocortin
- PRMT1:
-
Protein arginine methyltransferase 1
- ROS:
-
Reactive oxygen species
- SAM:
-
S-adenosyl methionine
- SAH:
-
S-adenosyl homocysteine
- 5-HT:
-
Serotonin
- SIRT:
-
Sirtuins
- SREBP1c:
-
Sterol response element binding protein 1c
- SAT:
-
Subcutaneous adipose tissue
- TNF-α:
-
Tumour necrosis factor-alpha
- T2DM:
-
Type 2 diabetes mellitus
- VAT:
-
Visceral adipose tissue
References
Aagaard-Tillery KM, Grove K, Bishop J, Ke X, Fu Q, McKnight R, Lane RH (2008) Developmental origins of disease and determinants of chromatin structure: maternal diet modifies the primate fetal epigenome. J Mol Endocrinol 41:91–102
Akchiche N, Bossenmeyer-Pourié C, Kerek R, Martin N, Pourié G, Koziel V, Helle D, Alberto JM, Ortiou S, Camadro JM, léger T, Guéant JL, Daval JL (2012) Homocysteinylation of neuronal proteins contributes to folate deficiency-associated alterations of differentiation, vesicular transport, and plasticity in hippocampal neuronal cells. FASEB J 26:3980–3992
Almén MS, Jacobsson JA, Moschonis G, Benedict C, Chrousos GP, Fredriksson R, Schiöth HB (2012) Genome wide analysis reveals association of a FTO gene variant with epigenetic changes. Genomics 99:132–137
Andringa KK, King AL, Eccleston HB, Mantena SK, Landar A, Jhala NC, Dickinson DA, Squadrito GL, Bailey SM (2010) Analysis of the liver mitochondrial proteome in response to ethanol and S-adenosylmethionine treatments: novel molecular targets of disease and hepatoprotection. Am J Physiol Gastrointest Liver Physiol 298:G732–G745
Bailey SM, Landar A, Darley-Usmar V (2005) Mitochondrial proteomics in free radical research. Free Radic Biol Med 38:175–188
Bailey SM, Robinson G, Pinner A, Chamlee L, Ulasova E, Pompilius M, Page GP, Chhieng D, Jhala N, Landar A, Kharbanda KK, Ballinger S, Darley-Usmar V (2006) S-adenosylmethionine prevents chronic alcohol-induced mitochondrial dysfunction in the rat liver. Am J Physiol Gastrointest Liver Physiol 291:G857–G867
Banke NH, Yan L, Pound KM, Dhar S, Reinhardt H, De Lorenzo MS, Vatner SF, Lewandowski ED (2012) Sexual dimorphism in cardiac triacylglyceride dynamics in mice on long term caloric restriction. J Mol Cell Cardiol 52:733–740
Banks AS, Kon N, Knight C, Matsumoto M, Gutierrez-Juarez R, Rossetti L, Gu W, Accili D (2008) SirT1 gain of function increases energy efficiency and prevents diabetes in mice. Cell Metab 8:333–341
Barbieri M, Di Filippo C, Esposito A, Marfella R, Rizzo MR, D’Amico M, Ferraraccio F, Di Ronza C, Duan SZ, Mortensen RM, Rossi F, Paolisso G (2012) Effects of PPARs agonists on cardiac metabolism in littermate and cardiomyocyte-specific PPAR-γ-knockout (CM-PGKO) mice. PLoS One 7:e35999
Barker DJP (2004) The developmental origins of adult disease. J Am Coll Nutr 23(suppl 6):588S–595S
Barres R, Kirchner H, Rasmussen M, Yan J, Kantor FR, Krook A, Näslund E, Zierath JR (2013) Weight loss after gastric bypass surgery in human obesity remodels promoter methylation. Cell Rep 3:1020–1027
Battaglia-Hsu SF, Akchiche N, Noel N, Alberto JM, Jeannesson E, Daval JL, Gueant JL (2009) Vitamin B12 deficiency reduces proliferation and promotes differentiation of neuroblastoma cells and upregulates PP2A, proNGF and TACE. Proc Natl Acad Sci U S A 16:21930–21935
Bell CG, Finer S, Lindgren CM, Wilson GA, Rakyan VK, Teschendorff AE, Akan P, Stupka E, Down TA, Prokopenko I, Morison IM, Mill J, Pidsley R (2010) Integrated genetic and epigenetic analysis identifies haplotype-specific methylation in the FTO type 2 diabetes and obesity susceptibility locus. PLoS ONE 5:e14040
Bergen NE, Jaddoe VW, Timmermans S, Hofman A, Lindemans J, Russcher H, Raat H, Steegers-Theunissen RP, Steegers EA (2012) Homocysteine and folate concentrations in early pregnancy and the risk of adverse pregnancy outcomes: the Generation R Study. BJOG 119:739–751
Björntorp P (1990) “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis 10:493–496
Blaise SA, Alberto JM, Audonnet-Blaise S, Guéant JL, Daval JL (2007) Influence of preconditioning-like hypoxia on the liver of developing methyl-deficient rats. Am J Physiol Endocrinol Metab 293:E1492–E1502
Blüher M (2010) The distinction of metabolically ‘healthy’ from ‘unhealthy’ obese individuals. Curr Opin Lipidol 21:38–43
Boden G, Zhang M (2006) Recent findings concerning thiazolidinediones in the treatment of diabetes. Expert Opin Investig Drugs 15:243–250
Bordone L, Cohen D, Robinson A, Motta MC, van Veen E, Czopik A, Steele AD, Crowe H, Marmor S, Luo J, Gu W, Guarente L (2007) SIRT1 transgenic mice show phenotypes resembling calorie restriction. Aging Cell 6:759–767
Bossenmeyer-Pourié C, Blaise S, Pourié G, Tomasetto C, Audonnet S, Ortiou S, Koziel V, Rio MC, Daval JL, Guéant JL, Beck B (2010) Methyl donor deficiency affects fetal programming of gastric ghrelin cell organization and function in the rat. Am J Pathol 176:270–277
Bouchard C, Tremblay A, Després JP, Nadeau A, Lupien PJ, Thériault G, Dussault J, Moorjani S, Pinault S, Fournier G (1990) The response to long-term overfeeding in identical twins. N Engl J Med 322:1477–1482
Bouchard L, Rabasa-Lhoret R, Faraj M, Lavoie ME, Mill J, Perusse L, Vohl MC (2010) Differential epigenomic and transcriptomic responses in subcutaneous adipose tissue between low and high responders to caloric restriction. Am J Clin Nutr 91:309–320
Bressenot A, Pooya S, Bossenmeyer-Pourie C, Gauchotte G, Germain A, Chevaux JB, Coste F, Vignaud JM, Guéant JL, Peyrin-Biroulet L (2012) Methyl donor deficiency affects small-intestinal differentiation and barrier function in rats. Br J Nutr 16:1–11
Brion MJ, Ness AR, Rogers I, Emmett P, Cribb V, Smith GD, Lawlor DA (2010) Maternal macronutrient and energy intakes in pregnancy and offspring intake at 10 y: exploring parental comparisons and prenatal effects. Am J Clin Nutr 91:748–756
Brunaud L, Alberto JM, Ayav A, Gérard P, Namour F, Antunes L, Braun M, Bronowicki JP, Bresler L, Guéant JL (2003) Vitamin B12 is a strong determinant of low methionine synthase activity and DNA hypomethylation in gastrectomized rats. Digestion 68:133–140
Brunet A, Sweeney LB, Sturgill JF, Chua KF, Greer PL, Lin Y, Tran H, Ross SE, Mostoslavsky R, Cohen HY, Hu LS, Cheng HL, Jedrychowski MP, Gygi SP, Sinclair DA, Alt FW, Greenberg ME (2004) Stress-dependent regulation of FOXO transcription factors by the SIRT1 deacetylase. Science 303:2011–2015
Burdge GC, Slater-Jefferies J, Torrens C, Phillips ES, Hanson MA, Lillycrop KA (2007) Dietary protein restriction of pregnant rats in the F0 generation induces altered methylation of hepatic gene promoters in the adult male offspring in the F1 and F2 generations. Br J Nutr 97:435–439
Burdge GC, Lillycrop KA, Phillips ES, Slater-Jefferies JL, Jackson AA, Hanson MA (2009) Folic acid supplementation during the juvenile–pubertal period in rats modifies the phenotype and epigenotype induced by prenatal nutrition. J Nutr 139:1054–1060
Burdge GC, Lillycrop KA (2010) Nutrition, epigenetics, and developmental plasticity: implications for understanding human disease. Annu Rev Nutr 30:315–339
Burgmaier M, Sen S, Philip F, Wilson CR, Miller CC 3rd, Young ME, Taegtmeyer H (2010) Metabolic adaptation follows contractile dysfunction in the heart of obese Zucker rats fed a high-fat “Western” diet. Obes (Silver Spring) 18:1895–1901
Campion J, Milagro FI, Martinez JA (2009) Individuality and epigenetics in obesity. Obes Rev 10:383–392
Cantó C, Auwerx J (2009) PGC-1alpha, SIRT1 and AMPK, an energy sensing network that controls energy expenditure. Curr Opin Lipidol 20:98–105
Cantó C, Auwerx J (2011) Calorie restriction: is AMPK a key sensor and effector? Physiology (Bethesda) 26:214–224
Cantó C, Auwerx J (2012) Targeting sirtuin 1 to improve metabolism: all you need is NAD(+)? Pharmacol Rev 64:166–187
Carone BR, Fauquier L, Habib N, Shea JM, Hart CE, Li R, Bock C, Li C, Gu H, Zamore PD, Meissner A, Weng Z, Hofmann HA, Friedman N, Rando OJ (2010) Paternally induced transgenerational environmental reprogramming of metabolic gene expression in mammals. Cell 143:1084–1096
Chang GQ, Gaysinskaya V, Karatayev O, Leibowitz SF (2008) Maternal high-fat diet and fetal programming: increased proliferation of hypothalamic peptide-producing neurons that increase risk for overeating and obesity. J Neurosci 28:12107–12119
Chen H, Simar D, Lambert K, Mercier J, Morris MJ (2008) Maternal and postnatal overnutrition differentially impact appetite regulators and fuel metabolism. Endocrinology 149:5348–5356
Christensen B, Rosenblatt DS (1995) Effects of folate deficiency on embryonic development. Baillieres Clin Haematol 8:617–637
Coste A, Louet JF, Lagouge M, Lerin C, Antal MC, Meziane H, Schoonjans K, Puigserver P, O’Malley BW, Auwerx J (2008) The genetic ablation of SRC-3 protects against obesity and improves insulin sensitivity by reducing the acetylation of PGC-1{alpha}. Proc Natl Acad Sci U S A 105:17187–17192
Cota D, Proulx K, Smith KA, Kozma SC, Thomas G, Woods SC, Seeley RJ (2006) Hypothalamic mTOR signaling regulates food intake. Science 312:927–930
Coupé B, Amarger V, Grit I, Benani A, Parnet P (2010) Nutritional programming affects hypothalamic organization and early response to leptin. Endocrinology 151:702–713
Danforth E (2000) Failure of adipocyte differentiation causes type II diabetes mellitus? Nat Genet 26:13
Davie JR (2003) Inhibition of histone deacetylase activity by butyrate. J Nutr 133:2485S–2493S
Desai M, Gayle D, Babu J, Ross MG (2007) The timing of nutrient restriction during rat pregnancy/lactation alters metabolic syndrome phenotype. Am J Obstet Gynecol 196(555):e1–e7
Dirkx E, Schwenk RW, Glatz JF, Luiken JJ, van Eys G (2011) High fat diet induced diabetic cardiomyopathy. Prostaglandins Leukot Essent Fat Acids 85:219–225
Dolinoy DC, Das R, Weidman JR, Jirtle RL (2007) Metastable epialleles, imprinting, and the fetal origins of adult diseases. Pediatr Res 61:30R–37R
Dominguez-Salas P, Moore SE, Cole D, da Costa KA, Cox SE, Dyer RA, Fulford AJ, Innis SM, Waterland RA, Zeisel SH, Prentice AM, Hennig BJ (2013) DNA methylation potential: dietary intake and blood concentrations of one-carbon metabolites and cofactors in rural African women. Am J Clin Nutr 97:1217–1227
Drong AW, Lindgren CM, McCarthy MI (2012) The genetic and epigenetic basis of type 2 diabetes and obesity. Clin Pharmacol Ther 92:707–715
Dudley KJ, Sloboda DM, Connor KL, Beltrand J, Vickers MH (2011) Offspring of mothers fed a high fat diet display hepatic cell cycle inhibition and associated changes in gene expression and DNA methylation. PLoS One 6:e21662
Düvel K, Yecies JL, Menon S, Raman P, Lipovsky AI, Souza AL, Triantafellow E, Ma Q, Gorski R, Cleaver S, Vander Heiden MG, MacKeigan JP, Finan PM, Clish CB, Murphy LO, Manning BD (2010) Activation of a metabolic gene regulatory network downstream of mTOR complex 1. Mol Cell 39:171–183
Fernandez-Marcos PJ, Auwerx J (2011) Regulation of PGC-1α, a nodal regulator of mitochondrial biogenesis. Am J Clin Nutr 93:884S–990S
Flamment M, Hajduch E, Ferré P, Foufelle F (2013) New insights into ER stress-induced insulin resistance. Trends Endocrinol Metab 23:381–390
Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S (2007) Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes 56:1010–1003
Fontana L, Meyer TE, Klein S, Holloszy JO (2004) Long-term calorie restriction is highly effective in reducing the risk for atherosclerosis in humans. Proc Natl Acad Sci U S A 101:6659–6663
Ford D (2012) Honeybees and cell lines as models of DNA methylation and aging in response to diet. Exp Gerontol 48:614–619
Forges T, Monnier-Barbarino P, Alberto JM, Guéant-Rodriguez RM, Daval JL, Guéant JL (2007) Impact of folate and homocysteine metabolism on human reproductive health. Hum Reprod Updat 13:225–238
Fraga MF, Ballestar E, Paz MF, Ropero S, Setien F, Ballestar ML, Heine-Suñer D, Cigudosa JC, Urioste M, Benitez J, Boix-Chornet M, Sanchez-Aguilera A, Ling C, Carlsson E, Poulsen P, Vaag A, Stephan Z, Spector TD, Wu YZ, Plass C, Esteller M (2005) Epigenetic differences arise during the lifetime of monozygotic twins. Proc Natl Acad Sci U S A 102:10604–10609
Frelut ML, Nicolas JP, Guilland JC, de Courcy GP (2011) Methylenetetrahydrofolate reductase 677 C→T polymorphism: a link between birth weight and insulin resistance in obese adolescents. Int J Pediatr Obes 6:e312–e317
Gabory A, Attig L, Junien C (2011) Developmental programming and epigenetics. Am J Clin Nutr 94:1943S–1952S
Gallinetti J, Harputlugil E, Mitchell JR (2013) Amino acid sensing in dietary-restriction-mediated longevity: roles of signal-transducing kinases GCN2 and TOR. Biochem J 449:1–10
Garcia MM, Guéant-Rodriguez RM, Pooya S, Brachet P, Alberto JM, Jeannesson E, Maskali F, Gueguen N, Marie PY, Lacolley P, Herrmann M, Juillière Y, Malthiery Y, Guéant JL (2011) Methyl donor deficiency induces cardiomyopathy through altered methylation/acetylation of PGC-1α by PRMT1 and SIRT1. J Pathol 225:324–335
Ghemrawi R, Pooya S, Lorentz S, Gauchotte G, Arnold C, Guéant JL, Battaglia-Hsu S (2013) Decreased vitamin B12 availability induces ER stress through impaired SIRT1-deacetylation of HSF1. Cell Death Dis 4:e553
Gietzen DW, Hao S, Anthony TG (2007) Mechanisms of food intake repression in indispensable amino acid deficiency. Annu Rev Nutr 27:63–78
Guéant JL, Caillerez-Fofou M, Battaglia-Hsu S, Alberto JM, Freund JN, Dulluc I, Adjalla C, Maury F, Merle C, Nicolas JP, Namour F, Daval JL (2013) Molecular and cellular effects of vitamin B12 in brain, myocardium and liver through its role as co-factor of methionine synthase. Biochimie 95:1033–1040
Guéant JL, Namour F, Guéant-Rodriguez RM, Daval JL (2013) Folate and fetal programming: a play in epigenomics? Trends Endocrinol Metab 24:279–289
Guéant-Rodriguez RM, Juillière Y, Nippert M, Abdelmouttaleb I, Herbeth B, Aliot E, Danchin N, Guéant JL (2007) Left ventricular systolic dysfunction is an independent predictor of homocysteine in angiographically documented patients with or without coronary artery lesions. J Thromb Haemost 5:1209–1216
Guéant-Rodriguez RM, Spada R, Pooya S, Jeannesson E, Moreno Garcia MA, Anello G, Bosco P, Elia M, Romano A, Alberto JM, Juillière Y, Guéant JL (2012) Homocysteine predicts increased NT-pro-BNP through impaired fatty acid oxidation. Int J Cardiol 167:768–775
Gulsen M, Yesilova Z, Bagci S, Uygun A, Ozcan A, Ercin CN, Erdil A, Sanisoglu SY, Cakir E, Ates Y, Erbil MK, Karaeren N, Dagalp K (2005) Elevated plasma homocysteine concentrations as a predictor of steatohepatitis in patients with non-alcoholic fatty liver disease. J Gastroenterol Hepatol 20:1448–1455
Guo F, Cavener DR (2007) The GCN2 eIF2alpha kinase regulates fatty-acid homeostasis in the liver during deprivation of an essential amino acid. Cell Metab 5:103–114
Hallows WC, Lee S, Denu JM (2006) Sirtuins deacetylate and activate mammalian acetyl-CoA synthetases. Proc Natl Acad Sci U S A 103:10230–10235
Hammer S, Snel M, Lamb HJ, Jazet IM, van der Meer RW, Pijl H, Meinders EA, Romijn JA, de Roos A, Smit JW (2008) Prolonged caloric restriction in obese patients with type 2 diabetes mellitus decreases myocardial triglyceride content and improves myocardial function. J Am Coll Cardiol 52:1006–1012
Han X, Turdi S, Hu N, Guo R, Zhang Y, Ren J (2012) Influence of long-term caloric restriction on myocardial and cardiomyocyte contractile function and autophagy in mice. J Nutr Biochem 23:1592–1599
Hebert AS, Dittenhafer-Reed KE, Yu W, Bailey DJ, Selen ES, Boersma MD, Carson JJ, Tonelli M, Balloon AJ, Higbee AJ, Westphall MS, Pagliarini DJ, Prolla TA, Assadi-Porter F, Roy S, Denu JM, Coon JJ (2013) Calorie restriction and SIRT3 trigger global reprogramming of the mitochondrial protein acetylome. Mol Cell 49:186–199
Heijmans BT, Tobi EW, Stein AD, Putter H, Blauw GJ, Susser ES, Slagboom PE, Lumey LH (2008) Persistent epigenetic differences associated with prenatal exposure to famine in humans. Proc Natl Acad Sci U S A 105:17046–17049
Herb BR, Wolschin F, Hansen KD, Aryee MJ, Langmead B, Irizarry R, Amdam GV, Feinberg AP (2012) Reversible switching between epigenetic states in honeybee behavioral subcastes. Nat Neurosci 15:1371–1373
Herrmann WW et al (2007) Homocysteine, brain natriuretic peptide and chronic heart failure: a critical review. Clin Chem Lab Med 45:1633–1644
Hirsch S, Poniachick J, Avendaño M, Csendes A, Burdiles P, Smok G, Diaz JC, de la Maza MP (2005) Serum folate and homocysteine levels in obese females with non-alcoholic fatty liver. Nutrition 21:137–141
Hoile SP, Lillycrop KA, Grenfell LR, Hanson MA, Burdge GC (2012) Increasing the folic acid content of maternal or postweaning diets induces differential changes in phosphoenolpyruvate carboxykinase mRNA expression and promoter methylation in rats. Br J Nutr 108:852–857
Hoile SP, Lillycrop KA, Thomas NA, Hanson MA, Burdge GC (2011) Dietary protein restriction during F0 pregnancy in rats induces transgenerational changes in the hepatic transcriptome in female offspring. PLoS One 6:e21668
Holness MJ, Caton PW, Sugden MC (2010) Acute and long-term nutrient-led modifications of gene expression: potential role of SIRT1 as a central co-ordinator of short and longer-term programming of tissue function. Nutrition 26:491–501
Houtkooper RH, Pirinen E, Auwerx J (2012) Sirtuins as regulators of metabolism and healthspan. Nat Rev Mol Cell Biol 13:225–238
Howie GJ, Sloboda DM, Kamal T, Vickers MH (2009) Maternal nutritional history predicts obesity in adult offspring independent of postnatal diet. J Physiol 587:905–915
Ivanova E, Chen JH, Segonds-Pichon A, Ozanne SE, Kelsey G (2012) DNA methylation at differentially methylated regions of imprinted genes is resistant to developmental programming by maternal nutrition. Epigenetics 7:1200–1210
Jakubowski H, Perla-Kaján J, Finnell RH et al (2009) Genetic or nutritional disorders in homocysteine or folate metabolism increase protein N-homocysteinylation in mice. FASEB J 23:1721–1727
Jeninga EH, Schoonjans K, Auwerx J (2010) Reversible acetylation of PGC-1: connecting energy sensors and effectors to guarantee metabolic flexibility. Oncogene 29:4617–4624
Jensen MD, Haymond MW, Rizza RA, Cryer PE, Miles JM (1989) Influence of body fat distribution on free fatty acid metabolism in obesity. J Clin Invest 83:1168–1173
Jia G, Fu Y, Zhao X, Dai Q, Zheng G, Yang Y, Yi C, Lindahl T, Pan T, Yang YG, He C (2011) N 6-methyladenosine in nuclear RNA is a major substrate of the obesity-associated FTO. Nat Chem Biol 7:885–887
Jiménez-Chillarón JC, Díaz R, Martínez D, Pentinat T, Ramón-Krauel M, Ribó S, Plösch T (2012) The role of nutrition on epigenetic modifications and their implications on health. Biochimie 94:2242–2263
Joseph J (2011) Fattening by deprivation: methyl balance and perinatal cardiomyopathy. J Pathol 225:315–317
Jousse C, Parry L, Lambert-Langlais S, Maurin AC, Averous J, Bruhat A, Carraro V, Tost J, Letteron P, Chen P, Jockers R, Launay JM, Mallet J, Fafournoux P (2011) Perinatal undernutrition affects the methylation and expression of the leptin gene in adults: implication for the understanding of metabolic syndrome. FASEB J 25:3271–3278
Kawakami K, Nakamura A, Goto S (2012) Dietary restriction increases site-specific histone H3 acetylation in rat liver: possible modulation by sirtuins. Biochem Biophys Res Commun 418:836–840
Kawano Y, Cohen DE (2013) Mechanisms of hepatic triglyceride accumulation in non-alcoholic fatty liver disease. J Gastroenterol 48:434–441
Kerek R, Geoffroy A, Guéant JL, Bossenmeyer-Pourié C, Daval JL (2013) Early methyl donor deficiency associated with alteration of the miR-124 and Stat3 signaling pathways impairs embryonic brain development. Cell Death Dis 4:e755
Kirchner H, Osler ME, Krook A, Zierath JR (2013) Epigenetic flexibility in metabolic regulation: disease cause and prevention? Trends Cell Biol 23:203–209
Kojima M, Kangawa K (2005) Ghrelin: structure and function. Physiol Rev 85:495–522
Kong AP, Xu G, Brown N, So WY, Ma RC, Chan JC (2013) Diabetes and its comorbidities—where east meets west. Nat Rev Endocrinol. doi:10.1038/nrendo.2013.102
Koplay M, Gulcan E, Ozkan F (2011) Association between serum vitamin B12 levels and the degree of steatosis in patients with nonalcoholic fatty liver disease. J Invest Med 59:1137–1140
Kucharski R, Maleszka J, Foret S, Maleszka R (2008) Nutritional control of reproductive status in honeybees via DNA methylation. Science 319:1827–1830
Kuehnen P, Mischke M, Wiegand S, Sers C, Horsthemke B, Lau S, Keil T, Lee YA, Grueters A, Krude H (2012) An Alu element-associated hypermethylation variant of the POMC gene is associated with childhood obesity. PLoS Genet 8:e1002543
Lagouge M, Argmann C, Gerhart-Hines Z, Meziane H, Lerin C, Daussin F, Messadeq N, Milne J, Lambert P, Elliott P, Geny B, Laakso M, Puigserver P, Auwerx J (2006) Resveratrol improves mitochondrial function and protects against metabolic disease by activating SIRT1 and PGC-1alpha. Cell 127:1109–1122
Lebrun P, Van Obberghen E (2008) SOCS proteins causing trouble in insulin action. Acta Physiol (Oxf) 192:29–36
Lewis SJ, Lawlor DA, Nordestgaard BG, Tybjaerg-Hansen A, Ebrahim S, Zacho J, Ness A, Leary S, Smith GD (2008) The methylenetetrahydrofolate reductase C677T genotype and the risk of obesity in three large population-based cohorts. Eur J Endocrinol 159:35–40
Lewis SJ, Leary S, Davey Smith G, Ness A (2009) Body composition at age 9 years, maternal folate intake during pregnancy and methyltetrahydrofolate reductase (MTHFR) C677T genotype. Br J Nutr 102:493–496
Li J, Huang J, Li JS, Chen H, Huang K, Zheng L (2011) Accumulation of endoplasmic reticulum stress and lipogenesis in the liver through generational effects of high fat diets. J Hepatol 56:900–907
Lillycrop KA, Phillips ES, Jackson AA, Hanson MA, Burdge GC (2005) Dietary protein restriction of pregnant rats induces and folic acid supplementation prevents epigenetic modification of hepatic gene expression in the offspring. J Nutr 135:1382–1386
Lillycrop KA, Phillips ES, Torrens C, Hanson MA, Jackson AA, Burdge GC (2008) Feeding pregnant rats a protein-restricted diet persistently alters the methylation of specific cytosines in the hepatic PPAR alpha promoter of the offspring. Br J Nutr 100:278–282
Lillycrop KA, Slater-Jefferies JL, Hanson MA, Godfrey KM, Jackson AA, Burdge GC (2007) Induction of altered epigenetic regulation of the hepatic glucocorticoid receptor in the offspring of rats fed a protein-restricted diet during pregnancy suggests that reduced DNA methyltransferase-1 expression is involved in impaired DNA methylation and changes in histone modifications. Br J Nutr 97:1064–1073
Lopes de Souza S, Orozco-Solis R, Grit I, Manhães de Castro R, Bolaños-Jiménez F (2008) Perinatal protein restriction reduces the inhibitory action of serotonin on food intake. Eur J Neurosci 27:1400–1408
Lowell BB, Shulman GI (2005) Mitochondrial dysfunction and type 2 diabetes. Science 307:384–387
Lumey LH, Stein AD, Ravelli AC (1995) Timing of prenatal starvation in women and birth weight in their first and second born offspring: the Dutch Famine Birth Cohort study. Eur J Obstet Gynecol Reprod Biol 61:23–30
Martinez E, Gérard N, Garcia MM, Mazur A, Guéant-Rodriguez RM, Comte B, Guéant JL, Brachet P (2013) Myocardium proteome remodelling after nutritional deprivation of methyl donors. J Nutr Biochem 24:1241–1250
Martínez-Chantar ML, García-Trevijano ER, Latasa MU, Pérez-Mato I, Sánchez del Pino MM, Corrales FJ, Avila MA, Mato JM (2002) Importance of a deficiency in S-adenosyl-l-methionine synthesis in the pathogenesis of liver injury. Am J Clin Nutr 76:1177S–1182S
Mato JM, Martínez-Chantar ML, Lu SC (2008) Methionine metabolism and liver disease. Annu Rev Nutr 28:273–293
McGregor RA, Choi MS (2011) MicroRNAs in the regulation of adipogenesis and obesity. Curr Mol Med 11:304–316
Meigs JB, Cupples LA, Wilson PW (2000) Parental transmission of type 2 diabetes: the Framingham Offspring Study. Diabetes 49:2201–2207
Menendez-Castro C, Fahlbusch F, Cordasic N, Amann K, Münzel K, Plank C, Wachtveitl R, Rascher W, Hilgers KF, Hartner A (2011) Early and late postnatal myocardial and vascular changes in a protein restriction rat model of intrauterine growth restriction. PLoS One 6:e20369
Meyer TE, Kovacs SJ, Ehsani AA, Klein S, Holloszy JO, Fontana L (2006) Long-term caloric restriction ameliorates the decline in diastolic function in humans. J Am Coll Cardiol 47:398–402
Milagro FI, Campion J, Cordero P, Goyenechea E, Gomez-Uriz AM, Abete I, Zulet MA, Martinez JA (2011) A dual epigenomic approach for the search of obesity biomarkers: DNA methylation in relation to diet-induced weight loss. FASEB J 25:1378–1389
Milagro FI, Campión J, García-Díaz DF, Goyenechea E, Paternain L, Martínez JA (2009) High fat diet-induced obesity modifies the methylation pattern of leptin promoter in rats. J Physiol Biochem 65:1–9
Miller BF, Robinson MM, Bruss MD, Hellerstein M, Hamilton KL (2012) A comprehensive assessment of mitochondrial protein synthesis and cellular proliferation with age and caloric restriction. Aging Cell 11:150–161
Miller RA, Buehner G, Chang Y, Harper JM, Sigler R, Smith-Wheelock M (2005) Methionine-deficient diet extends mouse lifespan, slows immune and lens aging, alters glucose, T4, IGF-I and insulin levels, and increases hepatocyte MIF levels and stress resistance. Aging Cell 4:119–125
Milne JC, Lambert PD, Schenk S et al (2007) Small molecule activators of SIRT1 as therapeutics for the treatment of type 2 diabetes. Nature 450:712–716
Skinner MK (2010) Metabolic disorders: fathers’ nutritional legacy. Nature 467:922–923
Muhlhausler BS, Adam CL, Findlay PA, Duffield JA, McMillen IC (2006) Increased maternal nutrition alters development of the appetite-regulating network in the brain. FASEB J 20:1257–1259
Mutti NS, Wang Y, Kaftanoglu O, Amdam GV (2011) Honey bee PTEN—description, developmental knockdown, and tissue-specific expression of splice-variants correlated with alternative social phenotypes. PLoS One 6:e22195
Nijland MJ, Mitsuya K, Li C, Ford S, McDonald TJ, Nathanielsz PW, Cox LA (2010) Epigenetic modification of fetal baboon hepatic phosphoenolpyruvate carboxykinase following exposure to moderately reduced nutrient availability. J Physiol 588:1349–1359
Nisoli E, Clementi E, Carruba MO, Moncada S (2007) Defective mitochondrial biogenesis: a hallmark of the high cardiovascular risk in the metabolic syndrome? Circ Res 100:795–806
Orozco-Solís R, Matos RJ, Guzmán-Quevedo O, Lopes de Souza S, Bihouée A, Houlgatte R, Manhães de Castro R, Bolaños-Jiménez F (2010) Nutritional programming in the rat is linked to long-lasting changes in nutrient sensing and energy homeostasis in the hypothalamus. PLoS One 5:e13537
Ouwens DM, Diamant M, Fodor M, Habets DD, Pelsers MM, El HM, Dang ZC, van den Brom CE, Vlasblom R, Rietdijk A, Boer C, Coort SL, Glatz JF, Luiken JJ (2007) Cardiac contractile dysfunction in insulin-resistant rats fed a high-fat diet is associated with elevated CD36-mediated fatty acid uptake and esterification. Diabetologia 50:1938–1948
Palou M, Priego T, Sánchez J, Palou A, Picó C (2012) Metabolic programming of sirtuin 1 (SIRT1) expression by moderate energy restriction during gestation in rats may be related to obesity susceptibility in later life. Br J Nutr 28:1–8
Parrado-Fernández C, López-Lluch G, Rodríguez-Bies E, Santa-Cruz S, Navas P, Ramsey JJ, Villalba JM (2011) Calorie restriction modifies ubiquinone and COQ transcript levels in mouse tissues. Free Radic Biol Med 50:1728–1736
Pellanda H, Forges T, Bressenot A, Chango A, Bronowicki JP, Guéant JL, Namour F (2012) Fumonisin FB1 treatment acts synergistically with methyl donor deficiency during rat pregnancy to produce alterations of H3- and H4-histone methylation patterns in fetuses. Mol Nutr Food Res 56:976–985
Perrone CE, Mattocks DA, Hristopoulos G, Plummer JD, Krajcik RA, Orentreich N (2008) Methionine restriction effects on 11-HSD1 activity and lipogenic/lipolytic balance in F344 rat adipose tissue. J Lipid Res 49:12–23
Peters JM, Hennuyer N, Staels B, Fruchart JC, Fievet C, Gonzalez FJ, Auwerx J (1997) Alterations in lipoprotein metabolism in peroxisome proliferator-activated receptor alpha-deficient mice. J Biol Chem 272:27307–27312
Petrik J, Reusens B, Arany E, Remacle C, Coelho C, Hoet JJ, Hill DJ (1999) A low protein diet alters the balance of islet cell replication and apoptosis in the fetal and neonatal rat and is associated with a reduced pancreatic expression of insulin-like growth factor-II. Endocrinology 140:4861–4873
Plagemann A, Harder T, Brunn M, Harder A, Roepke K, Wittrock-Staar M, Ziska T, Schellong K, Rodekamp E, Melchior K, Dudenhausen JW (2009) Hypothalamic proopiomelanocortin promoter methylation becomes altered by early overfeeding: an epigenetic model of obesity and the metabolic syndrome. J Physiol 587:4963–4976
Plagemann A, Roepke K, Harder T, Brunn M, Harder A, Wittrock-Staar M, Ziska T, Schellong K, Rodekamp E, Melchior K, Dudenhausen JW (2010) Epigenetic malprogramming of the insulin receptor promoter due to developmental overfeeding. J Perinat Med 38:393–400
Pogribny IP, Tryndyak VP, Bagnyukova TV, Melnyk S, Montgomery B, Ross SA, Latendresse JR, Rusyn I, Beland FA (2009) Hepatic epigenetic phenotype predetermines individual susceptibility to hepatic steatosis in mice fed a lipogenic methyl-deficient diet. J Hepatol 51:176–186
Pooya S, Blaise S, Moreno Garcia M, Giudicelli J, Alberto JM, Guéant-Rodriguez RM, Jeannesson E, Gueguen N, Bressenot A, Nicolas B, Malthiery Y, Daval JL, Peyrin-Biroulet L, Bronowicki JP, Guéant JL (2012) Methyl donor deficiency impairs fatty acid oxidation through PGC-1α hypomethylation and decreased ER-α, ERR-α, and HNF-4α in the rat liver. J Hepatol 57:344–351
Portela A, Esteller M (2010) Epigenetic modifications and human disease. Nat Biotechnol 28:1057–1068
Primeau V, Coderre L, Karelis AD, Brochu M, Lavoie ME, Messier V, Sladek R, Rabasa-Lhoret R (2011) Characterizing the profile of obese patients who are metabolically healthy. Int J Obes (Lond) 35:971–981
Raychaudhuri N, Raychaudhuri S, Thamotharan M, Devaskar SU (2008) Histone code modifications repress glucose transporter 4 expression in the intrauterine growth-restricted offspring. J Biol Chem 283:13611–13626
Rees WD, Hay SM, Cruickshank M, Reusens B, Remacle C, Antipatis C, Grant G (2006) Maternal protein intake in the pregnant rat programs the insulin axis and body composition in the offspring. Metabolism 55:642–649
ReesWD HSM, Brown DS, Antipatis C, Palmer RM (2000) Maternal protein deficiency causes hypermethylation of DNA in the livers of rat foetuses. J Nutr 130:1821–1826
Relling DP, Esberg LB, Fang CX, Johnson WT, Murphy EJ, Carlson EC, Saari JT, Ren J (2006) High-fat diet-induced juvenile obesity leads to cardiomyocyte dysfunction and upregulation of Foxo3a transcription factor independent of lipotoxicity and apoptosis. J Hypertens 24:549–561
Rodgers JT, Lerin C, Haas W, Gygi SP, Spiegelman BM, Puigserver P (2005) Nutrient control of glucose homeostasis through a complex of PGC-1alpha and SIRT1. Nature 434:113–118
Roseboom T, de Rooij S, Painter R (2006) The Dutch famine and its long-term consequences for adult health. Early Hum Dev 82:485–491
Roseboom TJ, van der Meulen JH, Osmond C, Barker DJ, Ravelli AC, Schroeder-Tanka JM, van Montfrans GA, Michels RP, Bleker OP (2000) Coronary heart disease after prenatal exposure to the Dutch famine, 1944–1945. Heart 84:595–598
Russo GT, Di Benedetto A, Alessi E, Ientile R, Antico A, Nicocia G, La Scala R, Di Cesare E, Raimondo G, Cucinotta D (2006) Mild hyperhomocysteinemia and the common C677T polymorphism of methylene tetrahydrofolate reductase gene are not associated with the metabolic syndrome in type 2 diabetes. J Endocrinol Investig 29:201–207
Russo P, Doyon J, Sonsino E, Ogier H, Saudubray JM (1992) A congenital anomaly of vitamin B12 metabolism: a study of three cases. Hum Pathol 23:504–512
Sack MN (2011) Caloric excess or restriction mediated modulation of metabolic enzyme acetylation-proposed effects on cardiac growth and function. Biochim Biophys Acta 1813:1279–1285
Sinclair KD, Allegrucci C, Singh R, Gardner DS, Sebastian S, Bispham J, Thurston A, Huntley JF, Rees WD, Maloney CA, Lea RG, Craigon J, McEvoy TG, Young LE (2007) DNA methylation, insulin resistance, and blood pressure in offspring determined by maternal periconceptional B vitamin and methionine status. Proc Natl Acad Sci U S A 104:19351–19356
Slater-Jefferies JL, Lillycrop KA, Townsend PA, Torrens C, Hoile SP, Hanson MA, Burdge GC (2011) Feeding a protein-restricted diet during pregnancy induces altered epigenetic regulation of peroxisomal proliferator-activated receptor-α in the heart of the offspring. J Dev Orig Health Dis 2:250–255
Sohi G, Marchand K, Revesz A, Arany E, Hardy DB (2011) Maternal protein restriction elevates cholesterol in adult rat offspring due to repressive changes in histone modifications at the cholesterol 7alpha-hydroxylase promoter. Mol Endocrinol 25:785–798
Speakman JR, Mitchell SE (2011) Caloric restriction. Mol Aspects Med 32:159–221
Stewart CP et al (2011) Low maternal vitamin B-12 status is associated with offspring insulin resistance regardless of antenatal micronutrient. J Nutr 141:1912–1917
Stover PJ (2011) Polymorphisms in 1-carbon metabolism, epigenetics and folate-related pathologies. J Nutrigenet Nutrigenomics 4:293–305
Sun Z, Singh N, Mullican SE, Everett LJ, Li L, Yuan L, Liu X, Epstein JA, Lazar MA (2011) Diet-induced lethality due to deletion of the Hdac3 gene in heart and skeletal muscle. J Biol Chem 286:33301–33339
Suter MA, Chen A, Burdine MS, Choudhury M, Harris RA, Lane RH, Friedman JE, Grove KL, Tackett AJ, Aagaard KM (2012) A maternal high-fat diet modulates fetal SIRT1 histone and protein deacetylase activity in nonhuman primates. FASEB J 26:5106–1514
Sykora P, Kharbanda KK, Crumm SE, Cahill A (2009) S-adenosyl-l-methionine co-administration prevents the ethanol-elicited dissociation of hepatic mitochondrial ribosomes in male rats. Alcohol Clin Exp Res 33:1–9
Tabassum R, Jaiswal A, Chauhan G, Dwivedi OP, Ghosh S, Marwaha RK, Tandon N, Bharadwaj D (2012) Genetic variant of AMD1 is associated with obesity in urban Indian children. PLoS One 7:e33162
Taksali SE, Caprio S, Dziura J, Dufour S, Calí AM, Goodman TR, Papademetris X, Burgert TS, Pierpont BM, Savoye M, Shaw M, Seyal AA, Weiss R (2008) High visceral and low abdominal subcutaneous fat stores in the obese adolescent: a determinant of an adverse metabolic phenotype. Diabetes 57:367–371
Tarry-Adkins JL, Chen JH, Jones RH, Smith NH, Ozanne SE (2010) Poor maternal nutrition leads to alterations in oxidative stress, antioxidant defense capacity, and markers of fibrosis in rat islets: potential underlying mechanisms for development of the diabetic phenotype in later life. FASEB J 24:2762–2771
Tateishi K, Okada Y, Kallin EM, Zhang Y (2009) Role of Jhdm2a in regulating metabolic gene expression and obesity resistance. Nature 458:757–761
Teperino R, Schoonjans K, Auwerx J (2010) Histone methyl transferases and demethylases; can they link metabolism and transcription? Cell Metab 12:321–327
Timmermans S, Jaddoe VW, Hofman A, Steegers-Theunissen RP, Steegers EA (2009) Periconception folic acid supplementation, fetal growth and the risks of low birth weight and preterm birth: the Generation R Study. Br J Nutr 102:777–785
Tobi EW, Lumey LH, Talens RP, Kremer D, Putter H, Stein AD, Slagboom PE, Heijmans BT (2009) DNA methylation differences after exposure to prenatal famine are common and timing- and sex-specific. Hum Mol Genet 18:4046–4053
Tryndyak V, de Conti A, Kobets T, Kutanzi K, Koturbash I, Han T, Fuscoe JC, Latendresse JR, Melnyk S, Shymonyak S, Collins L, Ross SA, Rusyn I, Beland FA, Pogribny IP (2012) Interstrain differences in the severity of liver injury induced by a choline- and folate-deficient diet in mice are associated with dysregulation of genes involved in lipid metabolism. FASEB J 26:4592–4602. doi:10.1096/fj.12-209569
Tsukada Y, Fang J, Erdjument-Bromage H, Warren ME, Borchers CH, Tempst P, Zhang Y (2006) Histone demethylation by a family of JmjC domain-containing proteins. Nature 439:811–816
Vaiman D, Gascoin-Lachambre G, Boubred F, Mondon F, Feuerstein JM, Ligi I, Grandvuillemin I, Barbaux S, Ghigo E, Achard V, Simeoni U, Buffat C (2011) The intensity of IUGR-induced transcriptome deregulations is inversely correlated with the onset of organ function in a rat model. PLoS One 6:e21222
Ventura-Clapier R, Garnier A, Veksler V (2008) Transcriptional control of mitochondrial biogenesis: the central role of PGC-1α. Cardiovasc Res 79:208–217
Verwey M, Amir S (2011) Nucleus-specific effects of meal duration on daily profiles of PERIOD1 and PERIOD2 protein expression in rats housed under restricted feeding. Neuroscience 192:304–311
Vucetic Z, Kimmel J, Totoki K, Hollenbeck E, Reyes TM (2010) Maternal high-fat diet alters methylation and gene expression of dopamine and opioid-related genes. Endocrinology 151:4756–4764
Wang J, Wu Z, Li D, Li N, Dindot SV, Satterfield MC, Bazer FW, Wu G (2012) Nutrition, epigenetics, and metabolic syndrome. Antioxid Redox Signal 17:282–301
Wang Y, Lobstein T (2006) Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 1:11–25
Watanabe K, Fujii H, Takahashi T, Kodama M, Aizawa Y, Ohta Y, Ono T, Hasegawa G, Naito M, Nakajima T, Kamijo Y, Gonzalez FJ, Aoyama T (2000) Constitutive regulation of cardiac fatty acid metabolism through peroxisome proliferator-activated receptor alpha associated with age-dependent cardiac toxicity. J Biol Chem 275:22293–22299
Waterland RA, Kellermayer R, Laritsky E, Rayco-Solon P, Harris RA, Travisano M, Zhang W, Torskaya MS, Zhang J, Shen L, Manary MJ, Prentice AM (2010) Season of conception in rural gambia affects DNA methylation at putative human metastable epialleles. PLoS Genet 6:e1001252
Weltman MD, Farrell GC, Liddle C (1996) Increased hepatocyte CYP2E1 expression in a rat nutritional model of hepatic steatosis with inflammation. Gastroenterology 111:1645–1653
Wolfe D, Gong M, Han G, Magee TR, Ross MG, Desai M (2012) Nutrient sensor-mediated programmed non-alcoholic fatty liver disease in low birth weight offspring. Am J Obstet Gynecol 207:308.e1–308.e6
Xiao F, Huang Z, Li H, Yu J, Wang C, Chen S, Meng Q, Cheng Y, Gao X, Li J, Liu Y, Guo F (2011) Leucine deprivation increases hepatic insulin sensitivity via GCN2/mTOR/S6K1 and AMPK pathways. Diabetes 60:746–756
Yajnik CS, Deshpande SS, Jackson AA, Refsum H, Rao S, Fisher DJ, Bhat DS, Naik SS, Coyaji KJ, Joglekar CV, Joshi N, Lubree HG, Deshpande VU, Rege SS, Fall CH (2008) Vitamin B12 and folate concentrations during pregnancy and insulin resistance in the offspring: the Pune Maternal Nutrition Study. Diabetologia 51:29–38
Yajnik CS, Deshmukh US (2012) Fetal programming: maternal nutrition and role of one-carbon metabolism. Rev Endocrinol Metab Disord 13:121–127
Yamamoto T, Sadoshima J (2011) Protection of the heart against ischemia/reperfusion by silent information regulator 1. Trends Cardiovasc Med 21:27–32
Yang J, Loos RJ, Powell JE, Medland SE, Speliotes EK, Chasman DI, Rose LM, Thorleifsson G, Steinthorsdottir V, Mägi R et al (2012) FTO genotype is associated with phenotypic variability of body mass index. Nature 490:267–272
Yu J, Auwerx J (2010) Protein deacetylation by SIRT1: an emerging key post-translational modification in metabolic regulation. Pharmacol Res 62:35–41
Zhang J, Zhang F, Didelot X, Bruce KD, Cagampang FR, Vatish M, Hanson M, Lehnert H, Ceriello A, Byrne CD (2009) Maternal high fat diet during pregnancy and lactation alters hepatic expression of insulin like growth factor-2 and key microRNAs in the adult offspring. BMC Genomics 10:478
Zhang Y, Yuan M, Bradley KM, Dong F, Anversa P, Ren J (2012) Insulin-like growth factor 1 alleviates high-fat diet-induced myocardial contractile dysfunction: role of insulin signaling and mitochondrial function. Hypertension 59:680–693
Zhao JY, Yang XY, Gong XH, Gu ZY, Duan WY, Wang J, Ye ZZ, Shen HB, Shi KH, Hou J, Huang GY, Jin L, Qiao B, Wang HY (2012) Functional variant in methionine synthase reductase intron-1 significantly increases the risk of congenital heart disease in the Han Chinese population. Circulation 125:482–490
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guéant, JL., Elakoum, R., Ziegler, O. et al. Nutritional models of foetal programming and nutrigenomic and epigenomic dysregulations of fatty acid metabolism in the liver and heart. Pflugers Arch - Eur J Physiol 466, 833–850 (2014). https://doi.org/10.1007/s00424-013-1339-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-013-1339-4