Abstract
Objectives
Longitudinal studies have linked stress at work with a higher incidence of musculoskeletal pain. We aimed to explore the extent to which musculoskeletal pain is a cause as opposed to a consequence of perceived occupational stress.
Methods
As part of the international cultural and psychosocial influences on disability study, we collected information from 305 Italian nurses, at baseline and again after 12 months, about pain during the past month in the low-back and neck/shoulder, and about effort–reward imbalance (ERI) (assessed by Siegrist’s ERI questionnaire). Poisson regression was used to assess the RR of ERI >1 at follow-up according to the report of pain and of ERI >1 at baseline.
Results
Among nurses with ERI ≤1 at baseline, ERI >1 at follow-up was associated with baseline report of pain in the low-back (RR 2.7, 95 % CI 1.4–5.0) and neck/shoulder (RR 2.6, 95 % CI 1.3–5.1). However, there was no corresponding association with persistence of ERI in nurses who already had ERI >1 at baseline. Associations of ERI at baseline with pain at follow-up were weak.
Conclusion
Our results suggest that the well-documented association between job stress and musculoskeletal pain is not explained entirely by an effect of stress on reporting of pain. It appears also that workers who report musculoskeletal pain are more likely to develop subsequent perceptions of stress. This may be because pain renders people less tolerant of the psychological demands of work. Another possibility is that reports of pain and stress are both manifestations of a general tendency to be aware of and complain about symptoms and difficulties.
Similar content being viewed by others
Introduction
Musculoskeletal disorders of the back, neck and upper limb are a major cause of morbidity, disability and long-term sickness absence (Schneider and Irastorza 2010; Office for National Statistics 2012), with substantial economic impact in European countries (Bevan et al. 2009). In some cases, symptoms arise from identifiable pathology such as a herniated inter-vertebral disc or compression of the median nerve in the carpal tunnel. Most often, however, the underlying pathology is unclear, and symptoms are classed as “non-specific” (Walker-Bone et al. 2004; Airaksinen et al. 2006; Krismer et al. 2007).
Epidemiological research has linked the occurrence of back, neck and upper limb disorders with various physical activities in the workplace (Lötters et al. 2003; Palmer and Smedley 2007), but such disorders are not a simple consequence of harmful physical exposures. There is a good evidence from observational studies that they are also associated with, and predicted by, psychological risk factors such as low mood, somatising tendency (a general tendency to worry about common somatic symptoms), job dissatisfaction and job stress (Sauter et al. 1996; Linton 2000; Palmer et al. 2005; MacFarlane et al. 2000).
The association with job stress could occur because stress increases awareness and reporting of pain, either through effects on the processing of sensory information in the central nervous system, or by changing the way in which physical tasks are performed (e.g. with increased muscle tension or altered posture) in a manner that makes them more likely to generate pain. However, it is also possible that pain renders people more prone to perceive and report occupational stress. A recent systematic review and meta-analysis of longitudinal studies (Lang et al. 2012) indicated that perceived stress had small but significant lagged effects on the development of musculoskeletal symptoms. However, this does not preclude a causal relationship also in the opposite direction, which would tend to increase the strength of associations between stress and musculoskeletal pain in cross-sectional surveys. If musculoskeletal pain predisposed workers to subsequent stress, greater attention to mental health would be indicated when workers with musculoskeletal disorders present to occupational health services.
To explore the extent to which musculoskeletal pain is a cause as opposed to a consequence of perceived occupational stress, we analysed longitudinal data on a sample of Italian nurses from the Cultural and Psychosocial Influences on Disability (CUPID) study (Coggon et al. 2012).
Methods
During February–March 2010, we invited all nurses who were employed on medical wards at a large public hospital in Varese, Italy, and who had worked in their current job for at least one year, to complete a baseline self-administered questionnaire about musculoskeletal pain and possible risk factors. Those who agreed and were still employed in the same position were then sent a second follow-up questionnaire after an interval of 12 months.
Questionnaires
The questionnaires were Italian translations (checked by independent back-translation) of instruments that had originally been drafted in English for use in the CUPID study (Coggon et al. 2012), supplemented by additional questions about weight and perceived occupational stress. Of relevance to this report, the baseline questionnaire asked about sex; weight; height; whether an average working day entailed lifting weights of 25 kg or more by hand; whether an average day at work involved working with the hands above shoulder height for longer than an hour; stress at work; and pain in the low-back, neck and shoulders.
Job stress was assessed through the Effort Reward Imbalance (ERI) questionnaire, which was developed by Siegrist and colleagues (Siegrist 2000), and has been used extensively in the investigation of occupational stress among nursing and medical personnel (Weyers et al. 2006; Lamy et al. 2013). We used the version of the questionnaire with 17 items, and for each participant, we quantified effort (6 items) and reward (11 items). Perceived stress was then scored as the ratio of effort to reward. As Siegrist recommended and has been done in earlier studies (Siegrist 1996; Peter et al. 1998), we classified subjects as exposed to high ERI if the ratio of the “effort” to “reward” scores, weighted for the numbers of items, exceeded 1.0.
The methods used to assess pain have been described in an earlier publication, which included a copy of the CUPID questionnaire (Coggon et al. 2012). Among other things, participants were asked whether at any time during the past month they had experienced pain lasting for more than a day in 10 anatomical regions that were depicted in diagrams. The same or similar questions had been used successfully in earlier studies, which collected information through self-administered questionnaires (Palmer et al. 2000, 2001). We defined neck/shoulder pain (NSP) as pain in any of the neck, right shoulder or left shoulder.
The follow-up questionnaire asked again about effort–reward imbalance and pain in the past month, using identical questions to those at baseline.
Statistical analysis
Statistical analysis was carried out with SAS version 9.2 software (Cary, NC, USA). Baseline predictors of low-back pain (LBP), NSP and perceived occupational stress at follow-up were investigated using Poisson multivariate regression models, and associations were summarised by risk ratios (RRs) with associated robust 95 % confidence intervals (CIs). The choice of potentially confounding variables for inclusion in the multivariate models was based on prior knowledge of established risk factors for musculoskeletal pain that might be differentially distributed across ERI categories (age, sex, BMI, physical workload).
Ethics
Ethical approval for the study was provided by the institutional board of the “Ospedale di Circolo Fondazione Macchi” Hospital of Varese, in which subjects were employed. Written informed consent was obtained for both questionnaires and from all participants.
Results
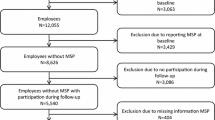
Baseline questionnaires were completed by 409 (79.0 %) of the 518 nurses who were invited to take part in the survey. Of these, 322 (78.7 %) also answered the follow-up questionnaire. After exclusion of 11 subjects with incomplete data in the follow-up questionnaire and a further six nurses who provided insufficient information for the calculation of ERI at baseline or follow-up, the main analysis was based on 305 subjects. Response rates at follow-up varied little by age, sex, BMI or report of pain at baseline, but were slightly lower in nurses with higher perceived stress when first recruited (supplementary Table S1).
Table 1 summarises various baseline characteristics of the 305 nurses who were included in the analysis. They were mostly female (250, 82 %), with a mean age at baseline of 39 years (SD = 9 years) and a mean BMI of 24 kg/m2 (SD = 4.5 kg/m2). At the time of recruitment, 55 (18 %) had an ERI >1, 159 (52 %) reported LBP, and 177 (58 %) reported NSP [including 122 (40 %) who complained of both LBP and NSP]. Nurses with an ERI >1 more frequently reported heavy lifting at work (72 vs. 64 % for nurses with ERI ≤1), and working with the arms elevated (31 vs. 25 %).
Table 2 shows the risk of perceived occupational stress (ERI >1) at follow-up according to the presence of LBP and NSP at baseline. In an analysis that adjusted for age, sex and BMI, LBP at baseline was associated with a more than doubled overall risk of occupational stress at follow-up (RR 2.1, 95 % CI 1.4–3.3). However, this association was limited to nurses who were free from occupational stress at baseline (RR 2.7, 95 % CI 1.4–5.0) and did not extend to those who started with ERI >1. Similarly, NSP at baseline was associated with an increased risk of ERI >1 at follow-up (RR 2.3, 95 % CI 1.4–3.8), but only in subjects with an ERI ≤1 at baseline (RR 2.6, 95 % CI 1.3–5.1).
Table 3 explores the relation between job stress at baseline and report of musculoskeletal pain at follow-up. A baseline ERI >1 was associated with the higher risk of both LBP and NSP (RR 1.2 95 % CI 1.0–1.5) at follow-up. However, this association was less stable, and when we stratified subjects according to pain at baseline, it was present only among subjects who were free from LBP at baseline and among subjects who already reported NSP at the start of the study.
Discussion
In this questionnaire-based longitudinal study, we found that perceived occupational stress was associated with only a small increase in the risk of subsequent musculoskeletal pain, whereas report of pain at baseline carried a substantially increased risk of newly developed stress at follow-up. However, there was no evidence that pain promoted the persistence of stress that was already present at baseline.
We focused on nursing personnel employed in hospital wards, an occupational group with exposure to both psychological and physical workload and often reported to have a relatively high prevalence of musculoskeletal pain, especially in the low-back (Lorusso et al. 2007). Moreover, earlier analysis of the CUPID study had shown that the prevalence of disabling low-back pain in Italian nurses was higher than among nurses in many other participating countries (Coggon et al. 2013). The high prevalence of pain in our sample increased our power to detect associations. High ERI was observed in a smaller proportion of subjects (18 %), a prevalence slightly lower than in recent data from large European occupational cohorts (Lunau et al. 2013; Liao et al. 2013).
A major strength of our study was its longitudinal design, which enabled us to explore the temporal relationship between job stress and musculoskeletal pain. Furthermore, the response rate at follow-up was relatively high (78.7 %) and varied little by relevant baseline characteristics. It therefore seems unlikely that the associations of interest were importantly biased by incomplete participation. Also, we used well-established instruments for the assessment of musculoskeletal pain, job stress and potentially confounding variables.
Against this, the size of the study sample was only modest (305), which limits the conclusions that can be drawn from sub-analyses (e.g. in strata of baseline characteristics). Nevertheless, several clear patterns emerged, and conclusions are strengthened by the similarity of results for LBP and NSP, although there was substantial overlap between the two symptoms.
Some information was lost by our decision to dichotomise our measure of ERI, but we opted to do this because we were most interested in potentially important levels of job stress, and it made the analysis easier to interpret. Importantly, the cut-point for definition of ERI was determined a priori from an earlier recommendation (Siegrist et al. 2004).
A recent review identified several longitudinal studies in which perceived stress predicted the subsequent development of somatic symptoms (Lang et al. 2012), but risk estimates were modest (high job strain carried a pooled odds ratio of 1.38 for LBP and 1.33 for NSP). Our data give some support to this finding, with only small increases in risk (RR 1.2 for LBP and 1.3 for NSP). Much stronger was the association between musculoskeletal pain at baseline and subsequent development of job stress. This may have occurred because experience of pain makes people less tolerant of the demands of work, although interestingly, the relationship did not extend to persistence of stress that was already present at baseline. The reasons for this discrepancy are unclear, and it may simply reflect chance sampling variation (because of small numbers, there was some overlap of confidence intervals—see Table 1).
Several longitudinal studies have previously investigated the relationship between job stress and musculoskeletal pain through repeated questionnaires (Sterud and Tynes 2013; Lindeberg et al. 2011; Miranda et al. 2005; Bonde et al. 2005; Hoogendoorn et al. 2002; Leino and Hänninen 1995), and most have found that risk of developing pain was higher in subjects previously exposed to stress. However, they did not explore the inverse relationship, looking at the risk of developing occupational stress in relation to earlier pain. To our knowledge, only one earlier study has done this (Devereux et al. 2011), and it found that report of neck problems was associated with an increased risk of future psychological distress (RR 1.66). Given our finding of a more than doubled risk of reporting occupational stress among workers free from stress but suffering from musculoskeletal pain one year earlier, it would be worth examining the relationship further in other data sets.
Concluding remarks
Our results suggest that the well-documented association between occupational stress and musculoskeletal pain is not explained entirely by an effect of stress on reporting of pain. In addition, it appears that workers who report musculoskeletal pain are more likely to develop subsequent perceptions of stress. This may be because pain renders people less tolerant of the psychological demands of work. Another possibility is that reports of pain and stress are both manifestations of a general tendency to be aware of and complain about symptoms and difficulties. If confirmed, our findings suggest a need for attention to mental health as well as physical symptoms and limitations when workers present to occupational health services with musculoskeletal pain.
References
Airaksen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G, COST B13 Working Group on Guidelines for Chronic Low Back Pain (2006) European guidelines for the management of chronic nonspecific low back pain. Eur Spine J Suppl 2:S192–S300
Bevan S, Quadrello T, McGee R, Mahdon M, Vavrovsky A, Barham L (2009) Fit for work? Musculoskeletal disorders in the European workforce. The Work Foundation. http://www.fitforworkeurope.eu/Website-Documents/FitfoWorkpan-Europeanreport.pdf. Accessed 2 May 2014
Bonde JP, Mikkelsen S, Andersen JH, Fallentin N, Baelum J, Svendsen SW, PRIM health study group et al (2005) Understanding work related musculoskeletal pain: does repetitive work cause stress symptoms? Occup Environ Med 62(1):41–48
Coggon D, Ntani G, Palmer KT, Felli VE, Harari R et al (2012) The CUPID (Cultural and Psychosocial Influences on Disability) study: methods of data collection and characteristics of study sample. PLoS One 7(7):e39820. doi:10.1371/journal.pone.0039820
Coggon D, Ntani G, Palmer KT, Felli VE, Harari R, Barrero LH et al (2013) Disabling musculoskeletal pain in working populations: is it the job, the person or the culture? Pain 154:856–863
Devereux JJ, Rydstedt LW, Cropley M (2011) Psychosocial work characteristics, need for recovery and musculoskeletal problems predict psychological distress in a sample of British workers. Ergonomics 54(9):840–848. doi:10.1080/00140139.2011.595830
Hoogendoorn WE, Bongers PM, de Vet HC, Ariëns GA, van Mechelen W, Bouter LM (2002) High physical work load and low job satisfaction increase the risk of sickness absence due to low back pain: results of a prospective cohort study. Occup Environ Med 59(5):323–328
Krismer M, van Tulder M, Low Back Pain Group of the Bone and Joint Health Strategies for Europe Project (2007) Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific). Best Pract Res Clin Rheumatol 21(1):77–91
Lamy S, De Gaudemaris R, Lepage B, Sobaszek A, Caroly S et al (2013) The organizational work factors’ effect on mental health among hospital workers is mediated by perceived effort-reward imbalance: result of a longitudinal study. J Occup Environ Med 55(7):809–816. doi:10.1097/JOM.0b013e31828acb19
Lang J, Ochsmann E, Kraus T, Lang JWB (2012) Psychosocial work stressor as antecedents of musculoskeletal problems: a systematic review and meta-analysis of stability-adjusted longitudinal studies. Soc Sci Med 2012:1163–1174
Leino PI, Hänninen V (1995) Psychosocial factors at work in relation to back and limb disorders. Scand J Work Environ Health 21(2):134–142
Liao J, Brunner EJ, Kumari M (2013) Is there an association between work stress and diurnal cortisol patterns? Findings from the Whitehall II study. PLoS One 8(12):e81020
Lindeberg SI, Rosvall M, Choi B, Canivet C, Isacsson SO et al (2011) Psychosocial working conditions and exhaustion in a working population sample of Swedish middle-aged men and women. Eur J Public Health 21(2):190–196. doi:10.1093/eurpub/ckq039
Linton SJ (2000) A review of psychological risk factors in back and neck pain. Spine 25:1148–1156
Lorusso A, Bruno S, L'Abbate N (2007) A review of low back pain and musculoskeletal disorders among Italian nursing personnel. Ind Health 45(5):637–644
Lötters F, Burdorf A, Kuiper J, Miedema H (2003) Model for the work-relatedness of low-back pain. Scand J Work Environ Health 29:431–440
Lunau T, Wahrendorf M, Dragano N, Siegrist J (2013) Work stress and depressive symptoms in older employees: impact of national labour and social policies. BMC Public Health 13:1086
Macfarlane GJ, Hunt IM, Silman AJ (2000) Role of mechanical and psychosocial factors in the onset of forearm pain: prospective population based study. Br Med J 321:676–679
Miranda H, Viikari-Juntura E, Heistaro S, Heliövaara M, Riihimäki H (2005) A population study on differences in the determinants of a specific shoulder disorder versus nonspecific shoulder pain without clinical findings. Am J Epidemiol 161(9):847–855
Office for National Statistics (2012) Sickness absence in the labour market. http://www.ons.gov.uk/ons/dcp171776_265016.pdf. Accessed 2 May 2014
Palmer KT, Smedley J (2007) Work relatedness of chronic neck pain with physical findings—a systematic review. Scand J Work Environ Health 33:165–191
Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D (2000) Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years. Br Med J 320(7249):1577–1578
Palmer KT, Walker-Bone K, Griffin MJ, Syddall H, Pannett B, Coggon D, Cooper C (2001) Prevalence and occupational associations of neck pain in the British population. Scand J Work Environ Health 27(1):49–56
Palmer K, Calnan M, Wainwright D, Poole J, O’Neill C, Winterbottom A, Watkins C, Coggon D (2005) Disabling musculoskeletal pain and its relation to somatization: a community-based postal survey. Occup Med 55:612–617
Peter R, Alfredsson L, Hammar N, Siegrist J, Theorell T, Westerholm P (1998) High effort, low reward, and cardiovascular risk factors in employed Swedish men and women: baseline results from the WOLF Study. J Epidemiol Community Health 52(9):540–547
Sauter S, Swanson N (1996) An ecological model of musculoskeletal disorders in office work. In: Moon SD, Sauter SL (eds) Beyond biomechanics: psychosocial aspects of musculoskeletal disorders in office work. Taylor & Francis, London, pp 3–21
Schneider E, Irastorza X (2010) OSH in figures: work-related musculoskeletal disorders in the EU—facts and figures. European agency for safety and health at work. http://osha.europa.eu/en/publications/reports/TERO09009ENC. Accessed 2 May 2014
Siegrist J (1996) Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol 1(1):27–41
Siegrist J (2000) Place, social exchange and health: proposed sociological framework. Soc Sci Med 51(9):1283–1293
Siegrist J, Starke D, Chandola T, Godin I, Marmot M, Niedhammer I, Peter R (2004) The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med 58(8):1483–1499
Sterud T, Tynes T (2013) Work-related psychosocial and mechanical risk factors for low back pain: a 3-year follow-up study of the general working population in Norway. Occup Environ Med 70(5):296–302. doi:10.1136/oemed-2012-101116
Walker-Bone K, Palmer K, Reading I, Coggon D, Cooper C (2004) Prevalence and impact of musculoskeletal disorders of the upper limb in the general population. Arthritis Care Res 51:642–651
Weyers S, Peter R, Boggild H, Jeppesen HJ, Siegrist J (2006) Psychosocial work stress is associated with poor self-rated health in Danish nurses: a test of the a effort-reward imbalance model. Scand J Caring Sci 20(1):26–34
Acknowledgments
We thank, Dr. Rossana Borchini, Dr. Davide Parassoni, Dr. Filippo Piccinelli and Dr. Stefano Landone who carried out data collection in Varese Hospital and Paul Maurice Conway for back-translation of the Italian questionnaire. We are particularly grateful to all of the organisations that allowed us to approach their employees and all of the workers who kindly participated in the study.
Conflict of interest
All authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bonzini, M., Bertu’, L., Veronesi, G. et al. Is musculoskeletal pain a consequence or a cause of occupational stress? A longitudinal study. Int Arch Occup Environ Health 88, 607–612 (2015). https://doi.org/10.1007/s00420-014-0982-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-014-0982-1