Abstract
Purpose
At present, the standard treatment of neovascular age-related macular degeneration (AMD) is the repeated administration of antivascular endothelial growth factor (VEGF) agents. However, we often encounter patients who develop tachyphylaxis for anti-VEGF agents. In this study, we investigated the characteristics of patients who developed tachyphylaxis on repeated intravitreal aflibercept (IVA) injections for neovascular AMD and the frequency of tachyphylaxis.
Methods
Three hundred thirteen eyes (313 patients) with treatment-naïve AMD who achieved resolution soon after starting IVA and were followed up for ≥ 12 months were enrolled in this retrospective, interventional, consecutive case series. The eyes were investigated for tachyphylaxis to aflibercept. Tachyphylaxis was defined as absence of any improvement (more than 100 μm) in or worsening of CRT within 1 month after more than two repeated monthly IVA injections when the exudative change remained.
Results
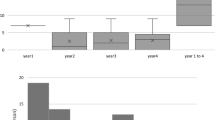
Twenty-eight (8.9%) of the 313 eyes developed tachyphylaxis (occult with no classic, n = 14; polypoidal choroidal vasculopathy, n = 14) at an annual rate of about 3%. The mean number of IVA injections was 10.5 ± 7.8, and the mean interval until tachyphylaxis was 20.9 ± 14.0 months. There was a significant difference in the AMD subtypes between the group with tachyphylaxis and the group without it (p = 0.0029). Occult with no classic type and polypoidal choroidal vasculopathy were the only AMD subtypes in the eyes with tachyphylaxis. In the analysis of the eyes that had occult with no classic or polypoidal choroidal vasculopathy, only intraretinal edema was significantly less common (p = 0.042). A combination of photodynamic therapy and aflibercept was effective in 13 (87%) of 15 eyes with tachyphylaxis, and switching to intravitreal ranibizumab was effective in 5 (56%) of 9 eyes.
Conclusions
Tachyphylaxis occurs after repeated IVA injections in a minority of patients with AMD for a long term and is more likely to occur in eyes with lesions beneath the retinal pigment epithelium and no intraretinal edema. Treatment of AMD should be performed keeping this fact in mind, while considering the consecutive treatment.








Similar content being viewed by others
References
Yasuda M, Kiyohara Y, Hata Y, Arakawa S, Yonemoto K, Doi Y, Iida M, Ishibashi T (2009) Nine-year incidence and risk factors for age-related macular degeneration in a defined Japanese population the Hisayama study. Ophthalmology 116:2135–2140. https://doi.org/10.1016/j.ophtha.2009.04.017
Mitchell P, Smith W, Attebo K, Wang JJ (1995) Prevalence of age-related maculopathy in Australia. The Blue Mountains Eye Study. Ophthalmology 102:1450–1460. https://doi.org/10.1016/S0161-6420(95)30846-9
Klein R, Klein BE, Tomany SC, Meuer SM, Huang GH (2002) Ten-year incidence and progression of age-related maculopathy: the Beaver Dam eye study. Ophthalmology 109:1767–1779. https://doi.org/10.1016/S0161-6420(02)01146-6
Frank RN, Amin RH, Eliott D, Puklin JE, Abrams GW (1996) Basic fibroblast growth factor and vascular endothelial growth factor are present in epiretinal and choroidal neovascular membranes. Am J Ophthalmol 122:393–403. https://doi.org/10.1016/S0002-9394(14)72066-5
D'Amore PA (1994) Mechanisms of retinal and choroidal neovascularization. Invest Ophthalmol Vis Sci 35:3974–3979
Forooghian F, Cukras C, Meyerle CB, Chew EY, Wong WT (2009) Tachyphylaxis after intravitreal bevacizumab for exudative age-related macular degeneration. Retina 29:723–731. https://doi.org/10.1097/IAE.0b013e3181a2c1c3
Schaal S, Kaplan HJ, Tezel TH (2008) Is there tachyphylaxis to intravitreal anti-vascular endothelial growth factor pharmacotherapy in age-related macular degeneration? Ophthalmology 115:2199–2205. https://doi.org/10.1016/j.ophtha.2008.07.007
Keane PA, Liakopoulos S, Ongchin SC, Heussen FM, Msutta S, Chang KT, Walsh AC, Sadda SR (2008) Quantitative subanalysis of optical coherence tomography after treatment with ranibizumab for neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci 49:3115–3120. https://doi.org/10.1167/iovs.08-1689
Gasperini JL, Fawzi AA, Khondkaryan A, Lam L, Chong LP, Eliott D, Walsh AC, Hwang J, Sadda SR (2012) Bevacizumab and ranibizumab tachyphylaxis in the treatment of choroidal neovascularisation. Br J Ophthalmol 96:14–20. https://doi.org/10.1136/bjo.2011.204685
Heier JS, Brown DM, Chong V, Korobelnik JF, Kaiser PK, Nguyen QD, Kirchhof B, Ho A, Ogura Y, Yancopoulos GD, Stahl N, Vitti R, Berliner AJ, Soo Y, Anderesi M, Groetzbach G, Sommerauer B, Sandbrink R, Simader C, Schmidt-Erfurth U, VIEW 1 and VIEW 2 Study Groups (2012) Intravitreal aflibercept (VEGF trap-eye) in wet age-related macular degeneration. Ophthalmology 119:2537–2548. https://doi.org/10.1016/j.ophtha.2012.09.006
Ogura Y, Terasaki H, Gomi F, Yuzawa M, Iida T, Honda M, Nishijo K, Sowade O, Komori T, Schmidt-Erfurth U, Simader C, Chong V, VIEW 2 Investigators (2015) Efficacy and safety of intravitreal aflibercept injection in wet age-related macular degeneration: outcomes in the Japanese subgroup of the VIEW 2 study. Br J Ophthalmol 99:92–97. https://doi.org/10.1136/bjophthalmol-2014-305076
Cho H, Shah CP, Weber M, Heier JS (2013) Aflibercept for exudative AMD with persistent fluid on ranibizumab and/or bevacizumab. Br J Ophthalmol 97:1032–1035. https://doi.org/10.1136/bjophthalmol-2013-303344
Bakall B, Folk JC, Boldt HC, Sohn EH, Stone EM, Russell SR, Mahajan VB (2013) Aflibercept therapy for exudative age-related macular degeneration resistant to bevacizumab and ranibizumab. Am J Ophthalmol 156:15–22.e1. https://doi.org/10.1016/j.ajo.2013.02.017
Lazzeri S, Ripandelli G, Sartini MS, Parravano M, Varano M, Nardi M, Di Desidero T, Orlandi P, Bocci G (2015) Aflibercept administration in neovascular age-related macular degeneration refractory to previous anti-vascular endothelial growth factor drugs: a critical review and new possible approaches to move forward. Angiogenesis 18:397–432. https://doi.org/10.1007/s10456-015-9483-4
Fung AE, Lalwani GA, Rosenfeld PJ, Dubovy SR, Michels S, Feuer WJ, Puliafito CA, Davis JL, Flynn HW Jr, Esquiabro M (2007) An optical coherence tomography-guided, variable dosing regimen with intravitreal ranibizumab (Lucentis) for neovascular age-related macular degeneration. Am J Ophthalmol 143:566–583. https://doi.org/10.1016/j.ajo.2007.01.028
Eghøj MS, Sørensen TL (2012) Tachyphylaxis during treatment of exudative age-related macular degeneration with ranibizumab. Br J Ophthalmol 96:21–23. https://doi.org/10.1136/bjo.2011.203893
Doguizi S, Ozdek S, Yuksel S (2015) Tachyphylaxis during ranibizumab treatment of exudative age-related macular degeneration. Int J Ophthalmol 8:846–848. https://doi.org/10.3980/j.issn.2222-3959.2015.04.37
Freund KB, Zweifel SA, Engelbert M (2010) Do we need a new classification for choroidal neovascularization in age-related macular degeneration? Retina 30:1333–1349. https://doi.org/10.1097/IAE.0b013e3181e7976b
Schmidt-Erfurth U, Waldstein SM, Deak GG, Kundi M, Simader C (2015) Pigment epithelial detachment followed by retinal cystoid degeneration leads to vision loss in treatment of neovascular age-related macular degeneration. Ophthalmology 122:822–832. https://doi.org/10.1016/j.ophtha.2014.11.017
Grossniklaus HE, Ling JX, Wallace TM, Dithmar S, Lawson DH, Cohen C, Elner VM, Elner SG, Sternberg P Jr (2002) Macrophage and retinal pigment epithelium expression of angiogenic cytokines in choroidal neovascularization. Mol Vis 8:119–126
Amsterdam JD, Williams D, Michelson D, Adler LA, Dunner DL, Nierenberg AA, Reimherr FW, Schatzberg AF (2009) Tachyphylaxis after repeated antidepressant drug exposure in patients with recurrent major depressive disorder. Neuropsychobiology 59:227–233. https://doi.org/10.1159/000226611
Forooghian F, Chew EY, Meyerle CB, Cukras C, Wong WT (2011) Investigation of the role of neutralizing antibodies against bevacizumab as mediators of tachyphylaxis. Acta Ophthalmol 89:e206–e207. https://doi.org/10.1111/j.1755-3768.2009.01773.x
Rosenfeld PJ, Brown DM, Heier JS, Boyer DS, Kaiser PK, Chung CY, Kim RY, MARINA Study Group (2006) Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 355:1419–1431. https://doi.org/10.1056/NEJMoa054481
Shiragami C, Ono A, Kobayashi M, Manabe S, Yamashita A, Shiraga F (2014) Effect of switching therapy to pegaptanib in eyes with the persistent cases of exudative age-related macular degeneration. Medicine (Baltimore) 93:e116. https://doi.org/10.1097/MD.0000000000000116
Despreaux R, Cohen SY, Semoun O, Zambrowski O, Jung C, Oubraham H, Souied EH (2016) Short-term results of switchback from aflibercept to ranibizumab in neovascular age-related macular degeneartion in clinical practice. Greafes Arch Clin Exp Ophthalmol 254:639–644. https://doi.org/10.1007/s00417-015-3084-1
Miller JW, Walsh AW, Kramer M, Hasan T, Michaud N, Flotte TJ, Haimovici R, Gragoudas ES (1995) Photodynamic therapy of experimental choroidal neovascularization using lipoprotein-delivered benzoporphyrin. Arch Ophthalmol 113:810–818. https://doi.org/10.1001/archopht.1995.01100060136048
Kramer M, Miller JW, Michaud N, Moulton RS, Hasan T, Flotte TJ, Gragoudas ES (1996) Liposomal benzoporphyrin derivative verteporfin photodynamic therapy. Selective treatment of choroidal neovascularization in monkeys. Ophthalmology 103:427–438. https://doi.org/10.1016/S0161-6420(96)30675-1
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a proprietary interest or conflict of interest in any product mentioned in this article. Dr. Hara has received lecture fees from Alcon pharma, Bayer, Santen, Pfizer, and Senju. Dr. Wakabayashi has received lecture fees from Santen and Senju. Dr. Sayanagi has received lecture fees from Alcon pharma, Bayer, Senju, and Otsuka. Dr. Sakaguchi heads an affiliated endowed department (Menicon) and has received lecture fees from Alcon pharma, Santen, and Nihon Alcon. Dr. Kawasaki also heads an affiliated endowed department (Topcon) and has received lecture fees from Alcon pharma, Bayer, Novartis, Senju, Pfizer, Kowa, Takeda, Astellas, Santen, Nitto Medic, and Topcon, as well as consultancy fees from Novartis, Novo Nordisk, Roche, Office Future, Predictive Analytic Group, and MICIN. Dr. Nishida has received lecture fees from Alcon, Carl Zeiss, Otsuka, Pfizer, Santen, and Senju, as well as grants from HOYA and Santen. Dr. Fukushima and Dr. Sato have no disclosures to make.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Ethics Committee of Osaka University Graduate School of Medicine; approval number 10039) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
The need for informed consent was waived in view of the retrospective nature of the research.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hara, C., Wakabayashi, T., Fukushima, Y. et al. Tachyphylaxis during treatment of exudative age-related macular degeneration with aflibercept. Graefes Arch Clin Exp Ophthalmol 257, 2559–2569 (2019). https://doi.org/10.1007/s00417-019-04456-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-019-04456-2