Abstract
Purpose
This study aimed to report the clinical outcome of children with uveitis treated with anti-tumor necrosis factor alpha (TNF-α) agents.
Methods
This included a retrospective cohort study. Children with uveitis treated with infliximab or adalimumab in 2008–2014 at five dedicated uveitis clinics were identified by database search. Their medical records were reviewed for demographic data, clinical presentation, ocular complications, and visual outcome. Systemic side effects and the steroid-sparing effect of treatment were documented.
Results
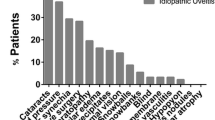
The cohort included 24 patients (43 eyes) of whom 14 received infliximab and 10 received adalimumab after failing conventional immunosuppression therapy. Mean age was 9.3 ± 4.0 years. The most common diagnosis was juvenile idiopathic arthritis-related uveitis (n = 10), followed by Behçet’s disease (n = 4), sarcoidosis (n = 1), and ankylosing spondylitis (n = 1); eight had idiopathic uveitis. Ocular manifestations included panuveitis in 20 eyes (46.5%), chronic anterior uveitis in 19 (44.2%), and intermediate uveitis in 4 (9.3%). The duration of biologic treatment ranged from 6 to 72 months. During the 12 months prior to biologic treatment, while on conventional immunosuppressive therapy, mean visual acuity deteriorated from 0.22 to 0.45 logMAR, with a trend of recovery to 0.25 at 3 months after initiation of biologic treatment, remaining stable thereafter. A full corticosteroid-sparing effect was demonstrated in 16 of the 19 patients (84.2%) for whom data were available. Treatment was well tolerated.
Conclusions
Treatment of pediatric uveitis with anti-TNF-α agents may improve outcome while providing steroid-sparing effect, when conventional immunosuppression fails. The role of anti-TNF-α agents as first-line treatment should be further investigated in controlled prospective clinical trials.


Similar content being viewed by others
References
Lerman MA, Rabinovich CE (2015) The future is now: biologics for non-infectious pediatric anterior uveitis. Pediatr Drugs. https://doi.org/10.1007/s40272-015-0128-2
Jabs DA, Rosenbaum JT, Foster CS et al (2000) Guidelines for the use of immunosuppressive drugs in patients with ocular inflammatory disorders: recommendations of an expert panel. Am J Ophthalmol 130:492–513
Kahn P, Weiss M, Imundo LF, Levy DM (2006) Favorable response to high-dose infliximab for refractory childhood uveitis. Ophthalmology. https://doi.org/10.1016/j.ophtha.2006.01.005
Ardoin SP, Kredich D, Rabinovich E et al (2007) Infliximab to treat chronic noninfectious uveitis in children: retrospective case series with long-term follow-up. Am J Ophthalmol. https://doi.org/10.1016/j.ajo.2007.08.018
Biester S, Deuter C, Michels H et al (2007) Adalimumab in the therapy of uveitis in childhood. Br J Ophthalmol 91:319–324. https://doi.org/10.1136/bjo.2006.103721
Díaz-Llopis M, Salom D, Garcia-De-Vicuña C et al (2012) Treatment of refractory uveitis with adalimumab: a prospective multicenter study of 131 patients. Ophthalmology 119:1575–1581. https://doi.org/10.1016/j.ophtha.2012.02.018
Levy-Clarke G, Jabs DA, Read RW et al (2014) Expert panel recommendations for the use of anti-tumor necrosis factor biologic agents in patients with ocular inflammatory disorders. Ophthalmology 121:785–796. https://doi.org/10.1016/j.ophtha.2013.09.048
Jabs DA (2005) Standardization of uveitis nomenclature for reporting clinical data. Results of the first international workshop. Am J Ophthalmol 140:509–516. https://doi.org/10.1016/j.ajo.2005.03.057
Saurenmann RK, Levin AV, Rose JB et al (2006) Tumour necrosis factor alpha inhibitors in the treatment of childhood uveitis. Rheumatology (Oxford) 45:982–989. https://doi.org/10.1093/rheumatology/kel030
Gallagher M, Quinones K, Cervantes-Castañeda RA et al (2007) Biological response modifier therapy for refractory childhood uveitis. Br J Ophthalmol 91:1341–1344. https://doi.org/10.1136/bjo.2007.124081
Simonini G, Zannin ME, Caputo R et al (2008) Loss of efficacy during long-term infliximab therapy for sight-threatening childhood uveitis. Rheumatology 47:1510–1514. https://doi.org/10.1093/rheumatology/ken298
Ramanan AV, Dick AD, Jones AP et al (2016) THU0213 adalimumab in combination with methotrexate for the treatment of juvenile idiopathic arthritis associated uveitis: the sycamore trial. Ann Rheum Dis 75:264 LP–264265
De Boer J, Wulffraat N, Rothova a (2003) Visual loss in uveitis of childhood. Br J Ophthalmol 87:879–884. https://doi.org/10.1136/bjo.87.7.879
Cunningham ET (2000) Uveitis in children, Ocular Immunology and Inflammation, 8(4):251-261. https://doi.org/10.1076/ocii.8.4.251.6459
Sabri K, Saurenmann RK, Silverman ED, Levin AV (2008) Course, complications, and outcome of juvenile arthritis-related uveitis. J AAPOS 12:539–545. https://doi.org/10.1016/j.jaapos.2008.03.007
Edelsten C, Reddy MA, Stanford MR, Graham EM (2003) Visual loss associated with pediatric uveitis in english primary and referral centers. Am J Ophthalmol 135:676–680. https://doi.org/10.1016/S0002-9394(02)02148-7
Sen ES, Sharma S, Hinchcliffe A et al (2012) Use of adalimumab in refractory non-infectious childhood chronic uveitis: efficacy in ocular disease—a case cohort interventional study. Rheumatology (Oxford) 51:2199–2203. https://doi.org/10.1093/rheumatology/kes212
Kaburaki T, Namba K, Sonoda K et al (2014) Behçet’s disease ocular attack score 24: evaluation of ocular disease activity before and after initiation of infliximab. Jpn J Ophthalmol 58:120–130. https://doi.org/10.1007/s10384-013-0294-0
Schaap-Fogler M, Amer R, Friling R et al (2014) Anti-TNF-α agents for refractory cystoid macular edema associated with noninfectious uveitis. Graefes Arch Clin Exp Ophthalmol 252:633–640. https://doi.org/10.1007/s00417-013-2552-8
Rajaraman RT, Kimura Y, Li S et al (2006) Retrospective case review of pediatric patients with uveitis treated with infliximab. Ophthalmology 113:308–314. https://doi.org/10.1016/j.ophtha.2005.09.037
Anderson PJ (2005) Tumor necrosis factor inhibitors: clinical implications of their different immunogenicity profiles. Semin Arthritis Rheum 34:19–22. https://doi.org/10.1016/j.semarthrit.2005.01.005
Ruperto N, Lovell DJ, Cuttica R et al (2007) A randomized, placebo-controlled trial of infliximab plus methotrexate for the treatment of polyarticular-course juvenile rheumatoid arthritis. Arthritis Rheum 56:3096–3106. https://doi.org/10.1002/art.22838
Wolbink GJ, Vis M, Lems W et al (2006) Development of antiinfliximab antibodies and relationship to clinical response in patients with rheumatoid arthritis. Arthritis Rheum 54:711–715. https://doi.org/10.1002/art.21671
Samson CM, Waheed N, Baltatzis S, Foster CS (2001) Methotrexate therapy for chronic noninfectious uveitis: analysis of a case series of 160 patients. Ophthalmology 108:1134–1139
Lerman MA, Burnham JM, Chang PY et al (2013) Response of pediatric uveitis to tumor necrosis factor-α inhibitors. J Rheumatol. https://doi.org/10.3899/jrheum.121180
Sella R, Oray M, Friling R et al (2015) Dexamethasone intravitreal implant (Ozurdex®) for pediatric uveitis. Graefes Arch Clin Exp Ophthalmol 253:1777–1782. https://doi.org/10.1007/s00417-015-3124-x
Zannin ME, Birolo C, Gerloni VM et al (2013) Safety and efficacy of infliximab and adalimumab for refractory uveitis in juvenile idiopathic arthritis: 1-year followup data from the Italian registry. J Rheumatol 40:74–79. https://doi.org/10.3899/jrheum.120583
Simonini G, Taddio A, Cattalini M et al (2011) Prevention of flare recurrences in childhood-refractory chronic uveitis: an open-label comparative study of adalimumab versus infliximab. Arthritis Care Res (Hoboken) 63:612–618. https://doi.org/10.1002/acr.20404
Sobrin L, Kim EC, Christen W et al (2007) Infliximab therapy for the treatment of refractory ocular inflammatory disease. Arch Ophthalmol 125:895
Horneff G (2015) Safety of biologic therapies for the treatment of juvenile idiopathic arthritis. Expert Opin Drug Saf 14:1111–1126. https://doi.org/10.1517/14740338.2015.1042453
Acknowledgements
We would like to thank Mrs.Dorit Karesh for her contribution to the statistical analysis.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Michal Kramer served as an advisor to Abbvie and as principal investigator in a clinical trial, not related to this study. All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Deitch, I., Amer, R., Tomkins-Netzer, O. et al. The effect of anti-tumor necrosis factor alpha agents on the outcome in pediatric uveitis of diverse etiologies. Graefes Arch Clin Exp Ophthalmol 256, 801–808 (2018). https://doi.org/10.1007/s00417-018-3928-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-3928-6