Abstract
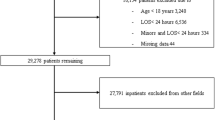
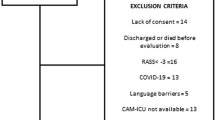
Delirium is the most common and serious neurobehavioral complication in acute hospital admissions. Some patients develop signs of delirium but do not meet all diagnostic criteria. Stroke is a major risk factor for delirium. The aim of this prospective study was to build a predictive model for delirium and subsyndromal post-stroke delirium. Patients with stroke were screened for delirium during the first 7 days after admission. Delirium was diagnosed according to DSM-V criteria. Baseline demographic, biochemical, stroke-related data, medications used, neurological deficit, and premorbid cognitive and functional impairment were assessed. 750 consecutive stroke patients (71.75 ± 13.13 years) were recruited; 203 (27.07%) had delirium. In predictive model for delirium MoCA score and white blood count on admission, neglect, vision deficits, physical impairment, and higher comorbidity prior to stroke had the highest predictive value. Subsyndromal delirium was diagnosed in 60 patients. MoCA score and potassium level on admission, and urinary tract infection during hospitalization had the highest predictive value for its development. Delirium occurs in one-fourth of admissions due to stroke; subsyndromal delirium is less prevalent and affects less than one per ten patients. The hyperactive form is the most rare type of delirium. The factors best predicting delirium are easily assessed in everyday practice and their co-occurrence in patients with stroke should alert the treating physician of high risk of delirium.
Similar content being viewed by others
References
Siddiqi N, House AO, Holmes JD (2006) Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing 35:350–364
Neto AS, Nassar AP Jr, Cardoso SO, Manetta JA, Pereira VG, Espósito DC et al (2012) Delirium screening in critically ill patients: a systematic review and meta-analysis. Crit Care Med 40:1946–1951
Liptzin B, Levkoff SE (1992) An empirical study of delirium subtypes. Br J Psychiatry 161:843–845
Kiely DK, Bergmann MA, Murphy KM, Jones RN, Orav EJ, Marcantonio ER (2003) Delirium among newly admitted postacute facility patients: prevalence, symptoms, and severity. J Gerontol A Biol Sci Med Sci 58:441–445
Cole MG, Ciampi A, Belzile E, Dubuc-Sarrasin M (2013) Subsyndromal delirium in older people: a systematic review of frequency, risk factors, course and outcomes. Int J Geriatr Psychiatry 28:771–780
Meagher D, O’Regan N, Ryan D, Connolly W, Boland E, O’Caoimhe R et al (2014) Frequency of delirium and subsyndromal delirium in an adult acute hospital population. Br J Psychiatry 205:478–785
Gustafson Y, Olsson T, Eriksson S, Asplund K, Bucht G (1991) Acute confusional states (delirium) in stroke patients. Cerebrovasc Dis 1:257–264
Henon H, Lebert F, Durieu I, Godefroy O, Lucas C, Pasquier F et al (1999) Confusional state in stroke. Relation to preexisting dementia, patient characteristics, and outcome. Stroke 30:773–779
Caeiro L, Ferro JM, Albuquerque R, Figueira ML (2004) Delirium in the first days of acute stroke. J Neurol 251:171–178
Sheng AZ, Shen Q, Cordato D, Zhang YY, Chan DKY (2006) Delirium within three days of stroke in a cohort of elderlypatients. J Am Geriatr Soc 54:1192–1198
Mc Manus J, Pathansali R, Hassan H, Ouldred E, Cooper D, Stewart R et al (2009) The evaluation of delirium post-stroke. Int J Geriatr Psychiatry 24:1251–1256
Oldenbeuving AW, de Kort PL, Jansen BP, Algra A, Kappelle LJ, Roks G (2011) Delirium in the acute phase after stroke: incidence, risk factors, and outcome. Neurology 15:993–999
Melkas S, Laurila JV, Vataja R, Oksala N, Jokinen H, Pohjasvaara T, Leppävuori A, Kaste M, Karhunen PJ, Erkinjuntti T (2012) Post-stroke delirium in relation to dementia and long-term mortality. Int J Geriatr Psychiatry 27:401–408
Mitasova A, Kostalova M, Bednarik J, Michalcakova R, Kasparek T, Balabanova P et al (2012) Poststroke delirium incidence and outcomes: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med 40:484–490
Miu DK, Yeung JC (2013) Incidence of post-stroke delirium and 1-year outcome. Geriatr Gerontol Int 13:123–129
Dahl MH, Rønning OM, Thommessen B (2010) Delirium in acute stroke-prevalence and risk factors. Acta Neurol Scand Suppl 190:39–43
Meagher D (2009) Motor subtypes of delirium: past, present and future. Int Rev Psychiatry 21:59–73
Intercollegiate Stroke Working Party (2012) National clinical guideline for stroke, 4th edn. Royal College of Physicians, London
Klimiec E, Dziedzic T, Kowalska K, Szyper A, Pera J, Potoczek P et al (2015) PRospective Observational POLIsh Study on post-stroke delirium (PROPOLIS): methodology of hospital-based cohort study on delirium prevalence, predictors and diagnostic tools. BMC Neurol 19(15):94
Inouye SK, Van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113:941–948
Ely EWE, Inouye SK, Bernard GR, Gordon S, Francis J, May L et al (2001) Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA 286:2703–2710
Trzepacz PT, Mittal D, Torres R, Kanary K, Norton J, Jimerson N (2001) Validation of the delirium rating scale-revised-98: comparison with the delirium rating scale and the cognitive test for delirium. J Neuropsychiatry Clin Neurosci 13:229–242
Hart RP, Levenson JL, Sessler CN, Best AM, Schwartz SM, Rutherford LE (1996) Validation of a cognitive test for delirium in medical ICU patients. Psychosomatics 37:533–546
Meagher DJ, Moran M, Raju B, Gibbons D, Donnelly S, Saunders J et al (2008) Motor symptoms in 100 patients with delirium versus control subjects: comparison of subtyping methods. Psychosomatics 49:300–308
Meagher D, Adamis D, Leonard M, Trzepacz P, Grover S, Jabbar F et al (2014) Development of an abbreviated version of the delirium motor subtyping scale (DMSS-4). Int Psychogeriatr 26:693–702
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, 5th edn. American Psychiatric Association, Arlington
Klimkowicz A, Dziedzic T, Slowik A, Szczudlik A (2002) Incidence of pre-and poststroke dementia: cracow stroke registry. Dement Geriatr Cogn Disord 14:137–140
Nasreddine ZS, Phillips NA, Bédirian V, Charbonneau S, Whitehead V, Collin I et al (2005) The Montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc 53:695–699
Dubois B, Slachevsky A, Litvan I, Pillon B (2000) The FAB: a frontal assessment battery at bedside. Neurology 2000(55):1621–1626
Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J (1994) The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementia. Neurology 44:2308–2314
de Groot V, Beckerman H, Lankhorst GJ, Bouter LM (2003) How to measure comorbidity. a critical review of available methods. J Clin Epidemiol 56:221–229
Adams HP, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al (1993) Classification of subtype of acute ischemic stroke. definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in acute stroke treatment
Meyer BC, Lyden PD (2009) The modified national institutes of health stroke scale: its time has come. Int J Stroke 4:267–273
Ojagbemi A, Owolabi M, Bello T, Baiyewu O (2017) Stroke severity predicts poststroke delirium and its association with dementia: longitudinal observation from a low income setting. J Neurol Sci 15:376–381
Kozak HH, Uğuz F, Kılınç İ, Uca AU, Serhat Tokgöz O, Akpınar Z et al (2017) Delirium in patients with acute ischemic stroke admitted to the non-intensive stroke unit: incidence and association between clinical features and inflammatory markers. Neurol Neurochir Pol 51:38–44
Alvarez-Perez FJ, Paiva F (2017) Prevalence and risk factors for delirium in acute stroke patients. a retrospective 5-years clinical series. J Stroke Cerebrovasc Dis 26:567–573
Arshad Q, Siddiqui S, Ramachandran S, Goga U, Bonsu A, Patel M et al (2015) Right hemisphere dominance directly predicts both baseline V1 cortical excitability and the degree of top-down modulation exerted over low-level brain structures. Neuroscience 17:484–489
Edlund A, Lundström M, Karlsson S, Brännström B, Bucht G, Gustafson Y (2006) Delirium in older patients admitted to general internal medicine. J Geriatr Psychiatry Neurol 19:83–90
The prevention, diagnosis and management of delirium in older people (2006) National Guidelines, Royal College of Physicians
Acknowledgements
We thank Malgorzata Mazurek for editing assistance.
Funding
The Leading National Research Centre funded the collection of data for the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical standard statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pasinska, P., Kowalska, K., Klimiec, E. et al. Frequency and predictors of post-stroke delirium in PRospective Observational POLIsh Study (PROPOLIS). J Neurol 265, 863–870 (2018). https://doi.org/10.1007/s00415-018-8782-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-018-8782-2