Abstract
Introduction
The purpose of this study was to identify the prevalence and severity of dysphagia in patients diagnosed with aspiration pneumonia, with and without neurologic disorders.
Methods
We retrospectively reviewed the medical records of inpatients with aspiration pneumonia who underwent a videofluoroscopic swallowing study (VFSS) for evaluation of dysphagia. Patients were divided into two groups based on the presence or absence of neurologic disorders. The prevalence and severity of aspiration and pharyngeal residue due to dysphagia were assessed using the penetration–aspiration scale (PAS) and pharyngeal residue grade (PRG).
Results
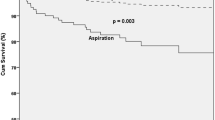
A total of 784 patients were enrolled; of these, 58.7% were males and the mean age was 76.12 ± 6.69. Penetration–aspiration-related dysphagia (PAS scores 3–8) was seen in 56.5% of all subjects, and 32.5% showed silent aspiration (PAS 8). Pharyngeal residue-related dysphagia (PRG scores 2–3) was seen in 65.2% of all patients, and the PAS and PRG were positively correlated. On dividing the subjects into two groups based on the presence of neurologic disorders, there was no significant difference in prevalence of the dysphagia between groups (PAS: p = 0.641; PRG: p = 0.872) with the proportion of silent aspiration (p = 0.720).
Conclusion
In patients hospitalized for aspiration pneumonia, there was a high prevalence of dysphagia. There were no differences in the prevalence and severity of dysphagia in patients with aspiration pneumonia based on the presence or absence of a neurologic disorder. Therefore, diagnostic evaluation of dysphagia is necessary regardless of the presence of neurologic disorders.


Similar content being viewed by others
References
Organization WH (2018) The top 10 causes of death. https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death
Marik PE (2001) Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 344(9):665–671. https://doi.org/10.1056/NEJM200103013440908
Taylor JK, Fleming GB, Singanayagam A et al (2013) Risk factors for aspiration in community-acquired pneumonia: analysis of a hospitalized UK cohort. Am J Med 126(11):995–1001
Yoshikawa TT, Marrie TJ (2000) Community-acquired pneumonia in the elderly. Clin Infect Dis 31(4):1066–1078
Hayashi M, Iwasaki T, Yamazaki Y et al (2014) Clinical features and outcomes of aspiration pneumonia compared with non-aspiration pneumonia: a retrospective cohort study. J Infect Chemother 20(7):436–4426
Teramoto S, Fukuchi Y, Sasaki H et al (2008) High incidence of aspiration pneumonia in community-and hospital-acquired pneumonia in hospitalized patients: a multicenter, prospective study in Japan. J Am Geriatr Soc 56(3):577–579
Mandell LA, Niederman MS (2019) Aspiration pneumonia. N Engl J Med 380(7):651–663. https://doi.org/10.1056/NEJMra1714562
Takizawa C, Gemmell E, Kenworthy J et al (2016) A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia 31(3):434–441
Eun KJ, Hae HW, Sung JJ (2019) The changes for strength of oropharyngeal muscles in patients with dementia and dysphagia. Brain NeuroRehabil 12(2):e12
Mokhlesi B, Logemann JA, Rademaker AW et al (2002) Oropharyngeal deglutition in stable COPD. Chest 121(2):361–369
DiBardino DM, Wunderink RG (2015) Aspiration pneumonia: a review of modern trends. J Crit Care 30(1):40–48
Wakabayashi H, Takahashi R, Murakami T (2019) The prevalence and prognosis of sarcopenic dysphagia in patients who require dysphagia rehabilitation. J Nutr Health Aging 23(1):84–88
Okazaki T, Ebihara S, Mori T et al (2020) Association between sarcopenia and pneumonia in older people. Geriatr Gerontol Int 20(1):7–13. https://doi.org/10.1111/ggi.13839
Cabre M, Serra-Prat M, Palomera E et al (2010) Prevalence and prognostic implications of dysphagia in elderly patients with pneumonia. Age Ageing 39(1):39–45
Belafsky PC, Kuhn MA (2014) The clinician’s guide to swallowing fluoroscopy. Springer, New York
Baijens LW, Clavé P, Cras P et al (2016) European Society for Swallowing Disorders - European Union Geriatric Medicine Society white paper: oropharyngeal dysphagia as a geriatric syndrome. Clin Interv Aging 11:1403–1428. https://doi.org/10.2147/cia.S107750
Logemann JA (1998) Evaluation and treatment of swallowing disorders, 2nd edn. PRO-ED, Austin
Johnson ER, McKenzie SW, Sievers A (1993) Aspiration pneumonia in stroke. Arch Phys Med Rehabil 74(9):973–976
Yu KJ, Moon H, Park D (2018) Different clinical predictors of aspiration pneumonia in dysphagic stroke patients related to stroke lesion: a STROBE-complaint retrospective study. Medicine (Baltimore) 97(52):e13968. https://doi.org/10.1097/md.0000000000013968
Watanabe S, Shimozato K, Oh-Shige H et al (2014) Examination of factors associated with aspiration pneumonia following stroke. Oral Sci Int 11(1):15–21. https://doi.org/10.1016/S1348-8643(13)00009-8
Park S, Lee JY, Jung H (2012) Use of videofluoroscopic swallowing study in patients with aspiration pneumonia. Ann Rehabil Med 36(6):785–790
Logemann JA (1993) Manual for the videofluorographic study of swallowing. Pro-ED, Austin
Rosenbek JC, Robbins JA, Roecker EB et al (1996) A penetration-aspiration scale. Dysphagia 11(2):93–98
Allen JE, White CJ, Leonard RJ et al (2010) Prevalence of penetration and aspiration on videofluoroscopy in normal individuals without dysphagia. Otolaryngol Head Neck Surg 142(2):208–21323
Daggett A, Logemann J, Rademaker A et al (2006) Laryngeal penetration during deglutition in normal subjects of various ages. Dysphagia 21(4):270–274
Han TR, Paik N-J, Park JW (2001) Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil 82(5):677–682
Dejaeger E, Pelemans W, Ponette E et al (1997) Mechanisms involved in postdeglutition retention in the elderly. Dysphagia 12(2):63–67
Cook I, Weltman M, Wallace K et al (1994) Influence of aging on oral-pharyngeal bolus transit and clearance during swallowing: scintigraphic study. Am J Physiol-Gastrointest Liver Physiol 266(6):972–977
Marik PE, Kaplan D (2003) Aspiration pneumonia and dysphagia in the elderly. Chest 124(1):328–336
Loeb M, Neupane B, Walter SD et al (2009) Environmental risk factors for community-acquired pneumonia hospitalization in older adults. J Am Geriatr Soc 57(6):1036–1040
Brodsky MB, Suiter DM, González-Fernández M et al (2016) Screening accuracy for aspiration using bedside water swallow tests: a systematic review and meta-analysis. Chest 150(1):148–163
Teramoto S (2014) Clinical significance of aspiration pneumonia and diffuse aspiration bronchiolitis in the elderly. J Gerontol Geriat Res 3(1):1–6
Ebihara S, Sekiya H, Miyagi M et al (2016) Dysphagia, dystussia, and aspiration pneumonia in elderly people. J Thorac Dis 8(3):632
Dang T, Majumdar S, Marrie T et al (2015) Recurrent pneumonia: a review with focus on clinical epidemiology and modifiable risk factors in elderly patients. Drugs Aging 32(1):13–19
Nakashima T, Maeda K, Tahira K et al (2018) Silent aspiration predicts mortality in older adults with aspiration pneumonia admitted to acute hospitals. Geriatr Gerontol Int 18(6):828–832. https://doi.org/10.1111/ggi.13250
Brady S, Donzelli J (2013) The modified barium swallow and the functional endoscopic evaluation of swallowing. Otolaryngol Clin N Am 46(6):1009–1022
Langmore SE, Schatz K, Olson N (1991) Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol 100(8):678–681. https://doi.org/10.1177/000348949110000815
Beck TJ, Gayler BW (1990) Image quality and radiation levels in videofluoroscopy for swallowing studies: a review. Dysphagia 5(3):118–128. https://doi.org/10.1007/bf02412634
Gates J, Hartnell GG, Gramigna GD (2006) Videofluoroscopy and swallowing studies for neurologic disease: a primer. Radiographics 26(1):e22. https://doi.org/10.1148/rg.e22
Splaingard ML, Hutchins B, Sulton LD et al (1988) Aspiration in rehabilitation patients: videofluoroscopy vs bedside clinical assessment. Arch Phys Med Rehabil 69(8):637–640
Rugiu MJAOI (2007) Role of videofluoroscopy in evaluation of neurologic dysphagia. Acta Otorhinolaryngol Ital 27(6):306
Omari TI, Kritas S, Cock C et al (2014) Swallowing dysfunction in healthy older people using pharyngeal pressure-flow analysis. Neurogastroenterol Motil 26(1):59–68
Aviv JE, Martin JH, Jones ME et al (1994) Age-related changes in pharyngeal and supraglottic sensation. Ann Otol Rhinol Laryngol 103(10):749–752
Ebihara S, Ebihara T, Kohzuki M (2012) Effect of aging on cough and swallowing reflexes: implications for preventing aspiration pneumonia. Lung 190(1):29–33. https://doi.org/10.1007/s00408-011-9334-z
Kikuchi R, Watabe N, Konno T et al (1994) High incidence of silent aspiration in elderly patients with community-acquired pneumonia. Am J Respir Crit Care Med 150(1):251–253
Love C, Opoku-Agyemang P, Tomas MB et al (2002) Pulmonary activity on labeled leukocyte images: physiologic, pathologic, and imaging correlation. RadioGraphics 22(6):1385–1393
Almirall J, Rofes L, Serra-Prat M et al (2013) Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J 41(4):923–92846
Nordio S, Di Stadio A, Koch I et al (2020) The correlation between pharyngeal residue, penetration/aspiration and nutritional modality: a cross-sectional study in patients with neurogenic dysphagia. Acta Otorhinolaryngol Ital 40(1):38–43. https://doi.org/10.14639/0392-100x-2136
Molfenter SM, Steele CM (2013) The relationship between residue and aspiration on the subsequent swallow: an application of the normalized residue ratio scale. Dysphagia 28(4):494–500. https://doi.org/10.1007/s00455-013-9459-8
Eisenhuber E, Schima W, Schober E et al (2002) Videofluoroscopic assessment of patients with dysphagia. Am J Roentgenol 178(2):393–398. https://doi.org/10.2214/ajr.178.2.1780393
Acknowledgements
We would like to extend thanks to all the members who work with us for performing VFSS in our dysphagia clinic. We would like to thank Editage for English language editing services.
Funding
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared that they have no conflict of interest.
Ethical Approval
This study was approved by the Institutional Review Board of Pusan National University Yangsan Hospital (No. 05-2020-100).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Seo, Z.W., Min, J.H., Huh, S. et al. Prevalence and Severity of Dysphagia Using Videofluoroscopic Swallowing Study in Patients with Aspiration Pneumonia. Lung 199, 55–61 (2021). https://doi.org/10.1007/s00408-020-00413-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00408-020-00413-7