Abstract
Purpose
Iodine deficiency affects 30% of populations worldwide. The amount of thyroglobulin (Tg) in blood increases in iodine deficiency and also in iodine excess. Tg is considered as a sensitive index of iodine status in groups of children and adults, but its usefulness for individuals is unknown. The aim of this study was to determine the diagnostic performance of Tg as an index of iodine status in individual adults.
Methods
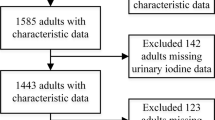
Adults aged 18–40 years (n = 151) provided five spot urine samples for the measurement of urinary iodine concentration expressed as μg/L (UIC), μg/g of creatinine (I:Cre), and μg/day (estimated UIE); the mean of the five samples was used as the reference standard. Participants also provided a blood sample for the determination of Tg, thyroid-stimulating hormone (TSH), and free thyroxine (FT4).
Results
The median of UIC, I:Cre, estimated UIE, and Tg was 72 (range 16–350) μg/L, 90 (range 33–371) μg/g, 129 (range 41–646) μg/day, and 16.4 (range 0.8–178.9) μg/L, respectively. Using Tg cut-offs of >10, >11, >13, and >15 μg/L, the sensitivity and specificity for UIC, I:Cre, and estimated UIE ranged from 52 to 79% and 20–48%, respectively, below the acceptable value of ≥80%. Furthermore, receiver-operating characteristic (ROC) curves for Tg using the three measurements of urinary iodine were situated close to the chance line and the area under the curve ranged from 0.49 to 0.52.
Conclusions
The results from this cross-sectional study indicate that Tg has low sensitivity and specificity to repeated measures of urinary iodine excretion. Further studies are still needed to investigate the usefulness of Tg as a biomarker of individual iodine status.


Similar content being viewed by others
References
WHO/UNICEF/ICCIDD (2007) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. 3rd edn. WHO, Geneva
Thomson CD, Colls AJ, Conaglen JV, Macormack M, Stiles M, Mann J (1997) Iodine status of New Zealand residents as assessed by urinary iodide excretion and thyroid hormones. Br J Nutr 78(6):901–912
Lazarus JH (2014) Iodine status in Europe in 2014. Eur Thyroid J 3(1):3–6. doi:10.1159/000358873
Knudsen N, Bülow I, Jørgensen T, Perrild H, Ovesen L, Laurberg P (2001) Serum Tg—a sensitive marker of thyroid abnormalities and iodine deficiency in epidemiological studies. J Clin Endocrinol Metab 86(8):3599–3603. doi:10.1210/jcem.86.8.7772
Ma ZF, Venn BJ, Manning PJ, Cameron CM, Skeaff SA (2016) Iodine supplementation of mildly iodine-deficient adults lowers thyroglobulin: a randomized controlled trial. J Clin Endocrinol Metab 101(4):1737–1744. doi:10.1210/jc.2015-3591
Swanson CA, Zimmermann MB, Skeaff S, Pearce EN, Dwyer JT, Trumbo PR, Zehaluk C, Andrews KW, Carriquiry A, Caldwell KL, Egan SK, Long SE, Bailey RL, Sullivan KM, Holden JM, Betz JM, Phinney KW, Brooks SP, Johnson CL, Haggans CJ (2012) Summary of an NIH workshop to identify research needs to improve the monitoring of iodine status in the United States and to inform the DRI. J Nutr 142(6):1175S–1185S. doi:10.3945/jn.111.156448
Giovanella L, Clark PM, Chiovato L, Duntas L, Elisei R, Feldt-Rasmussen U, Leenhardt L, Luster M, Schalin-Jantti C, Schott M, Seregni E, Rimmele H, Smit J, Verburg FA (2014) Thyroglobulin measurement using highly sensitive assays in patients with differentiated thyroid cancer: a clinical position paper. Eur J Endocrinol 171(2):R33–R46. doi:10.1530/eje-14-0148
Snozek CL, Chambers EP, Reading CC, Sebo TJ, Sistrunk JW, Singh RJ, Grebe SK (2007) Serum thyroglobulin, high-resolution ultrasound, and lymph node thyroglobulin in diagnosis of differentiated thyroid carcinoma nodal metastases. J Clin Endocrinol Metab 92(11):4278–4281. doi:10.1210/jc.2007-1075
Keutgen XM, Filicori F, Crowley MJ, Wang Y, Scognamiglio T, Hoda R, Buitrago D, Cooper D, Zeiger MA, Zarnegar R, Elemento O, Fahey TJI (2012) A panel of four miRNAs accurately differentiates malignant from benign indeterminate thyroid lesions on fine needle aspiration. Clin Cancer Res 18(7):2032–2038. doi:10.1158/1078-0432.ccr-11-2487
Xing M, Haugen BR, Schlumberger M (2013) Progress in molecular-based management of differentiated thyroid cancer. The Lancet 381(9871):1058–1069. doi:10.1016/s0140-6736(13)60109-9
König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB (2011) Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J Nutr 141(11):2049–2054. doi:10.3945/jn.111.144071
Edmonds JC, McLean RM, Williams SM, Skeaff SA (2015) Urinary iodine concentration of New Zealand adults improves with mandatory fortification of bread with iodised salt but not to predicted levels. Eur J Nutr 55(3):1201–1212. doi:10.1007/s00394-015-0933-y
Baloch Z, Carayon P, Conte-Devolx B, Demers LM, Feldt-Rasmussen U, Henry JF, LiVosli VA, Niccoli-Sire P, John R, Ruf J, Smyth PP, Spencer CA, Stockigt JR (2003) Laboratory medicine practice guidelines. Laboratory support for the diagnosis and monitoring of thyroid disease. Thyroid 13(1):3–126. doi:10.1089/105072503321086962
Pino S, Fang SL, Braverman LE (1996) Ammonium persulfate: a safe alternative oxidizing reagent for measuring urinary iodine. Clin Chem 42(2):239–243
Ohashi T, Yamaki M, Pandav CS, Karmarkar MG, Irie M (2000) Simple microplate method for determination of urinary iodine. Clin Chem 46(4):529–536
Fabiny DL, Ertingshausen G (1971) Automated reaction-rate method for determination of serum creatinine with the CentrifiChem. Clin Chem 17(8):696–700
Knudsen N, Christiansen E, Brandt-Christensen M, Nygaard B, Perrild H (2000) Age- and sex-adjusted iodine/creatinine ratio. A new standard in epidemiological surveys? Evaluation of three different estimates of iodine excretion based on casual urine samples and comparison to 24 h values. Eur J Clin Nutr 54(4):361–363
WHO/UNICEF/ICCIDD (1994) Indicators for assessing iodine deficiency disorders and their control through salt iodization. Document WHO/NUT, 6. WHO, Geneva, p 36
Friberg JC (2010) Considerations for test selection: How do validity and reliability impact diagnostic decisions? Child Lang Teach Ther 26(1):77–92. doi:10.1177/0265659009349972
Maxim LD, Niebo R, Utell MJ (2014) Screening tests: a review with examples. Inhal Toxicol 26(13):811–828. doi:10.3109/08958378.2014.955932
Zimmermann MB, Andersson M (2012) Assessment of iodine nutrition in populations: past, present, and future. Nutr Rev 70(10):553–570. doi:10.1111/j.1753-4887.2012.00528.x
Zimmermann MB, Aeberli I, Andersson M, Assey V, Yorg JA, Jooste P, Jukić T, Kartono D, Kusić Z, Pretell E, San Luis TO Jr, Untoro J, Timmer A (2013) Thyroglobulin is a sensitive measure of both deficient and excess iodine intakes in children and indicates no adverse effects on thyroid function in the UIC range of 100–299 µg/L: a UNICEF/ICCIDD study group report. J Clin Endocrinol Metab 98(3):1271–1280. doi:10.1210/jc.2012-3952
Hajian-Tilaki K (2013) Receiver operating characteristic (ROC) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med 4(2):627–635
Karmisholt J, Laurberg P, Andersen S (2014) Recommended number of participants in iodine nutrition studies is similar before and after an iodine fortification programme. Eur J Nutr 53(2):487–492. doi:10.1007/s00394-013-0551-5
Li C, Peng S, Zhang X, Xie X, Wang D, Mao J, Teng X, Shan Z, Teng W (2016) The urine iodine to creatinine as an optimal index of iodine during pregnancy in an iodine adequate area in China. J Clin Endocrinol Metab 101(3):1290–1298. doi:10.1210/jc.2015-3519
Gutekunst R, Smolarek H, Hasenpusch U, Stubbe P, Friedrich HJ, Wood WG, Scriba PC (1986) Goitre epidemiology: thyroid volume, iodine excretion, thyroglobulin and thyrotropin in Germany and Sweden. Acta Endocrinol (Copenh) 112 (4):494–501
Bjergved L, Jørgensen T, Perrild H, Carlé A, Cerqueira C, Krejbjerg A, Laurberg P, Ovesen L, Bulow Pedersen I, Banke RL, Knudsen N (2012) Predictors of change in serum TSH after iodine fortification: an 11-year follow-up to the DanThyr study. J Clin Endocrinol Metab 97(11):4022–4029. doi:10.1210/jc.2012-2508
Laurberg P, Jørgensen T, Perrild H, Ovesen L, Knudsen N, Pedersen IB, Rasmussen LB, Carlé A, Vejbjerg P (2006) The Danish investigation on iodine intake and thyroid disease, DanThyr: status and perspectives. Eur J Endocrinol 155(2):219–228. doi:10.1530/eje.1.02210
Rohner F, Zimmermann M, Jooste P, Pandav C, Caldwell K, Raghavan R, Raiten DJ (2014) Biomarkers of nutrition for development- iodine review. J Nutr 144(8):1322s–1342s. doi:10.3945/jn.113.181974
Feldt-Rasmussen U, Hyltoft Petersen P, Date J (1979) Sex and age correlated reference values of serum thyroglobulin measured by a modified radioimmunoassay. Acta Endocrinol (Copenh) 90(3):440–450
Feldt-Rasmussen U, Hyltoft Petersen P, Blaabjerg O, Hørder M (1980) Long-term variability in serum thyroglobulin and thyroid related hormones in healthy subjects. Acta Endocrinol (Copenh) 95(3):328–334
Jensen E, Petersen PH, Blaabjerg O, Hegedüs L (2007) Biological variation of thyroid autoantibodies and thyroglobulin. Clin Chem Lab Med 45(8):1058–1064. doi:10.1515/cclm.2007.185
Stinca S, Andersson M, Erhardt J, Zimmermann MB (2015) Development and validation of a new low-cost enzyme-linked immunoassay for serum and dried blood spot thyroglobulin. Thyroid 25(12):1297–1305. doi:10.1089/thy.2015.0428
Acknowledgements
The authors are extremely grateful to all the participants who took part and acknowledge Andrea Samson and Glenna Paterson for assistance with the collection of blood samples.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Funding
This work was supported by Laurenson fund from the Otago Medical Research Foundation and the Department of Human Nutrition, University of Otago.
Rights and permissions
About this article
Cite this article
Ma, Z.F., Venn, B.J., Manning, P.J. et al. The sensitivity and specificity of thyroglobulin concentration using repeated measures of urinary iodine excretion. Eur J Nutr 57, 1313–1320 (2018). https://doi.org/10.1007/s00394-017-1410-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-017-1410-6