Abstract
Purpose
We examined whether high doses of folic acid and iron supplementation in early-to-mid pregnancy affect the risk of preterm birth, low birth weight, and small for gestational age neonates, in the mother–child cohort in Crete, Greece (Rhea study).
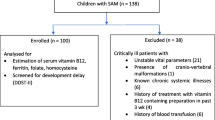
Methods
We included 1,279 women with singleton pregnancies with complete data on supplements use in early-to-mid pregnancy and birth outcomes. Anthropometric measurements at birth were obtained from medical records. Red blood cell folate concentrations in cord blood were measured in a subsample of the study population (n = 58).
Results
Sixty-six percent of the study participants reported high doses of supplemental folic acid use (5 mg/day), while 21 % reported excessive doses of folic acid use (>5 mg/day) in early-to-mid pregnancy. Daily intake of 5-mg supplemental folic acid was associated with a 31 % decrease in the risk of preterm birth (RR, 0.69; 95 % CI, 0.44, 0.99), 60 % decrease in the risk of delivering a low birth weight neonate (RR, 0.40; 95 % CI, 0.21, 0.76), and 66 % decrease in the risk of delivering a small for gestational age (SGA) neonate (RR, 0.34; 95 % CI, 0.16, 0.73). Daily doses of iron supplementation more than 100 mg were associated with a twofold increased risk for SGA neonates (RR, 2.14; 95 % CI, 0.99, 5.97).
Conclusion
These findings suggest that high daily doses of supplementary folic acid in early-to-mid pregnancy may be protective for preterm birth, low birth weight, and small for gestational age neonates, while high daily doses of supplementary iron may be harmful for fetal growth.
Similar content being viewed by others
References
Pena-Rosas JP, Viteri FE (2009) Effects and safety of preventive oral iron or iron + folic acid supplementation for women during pregnancy. Cochrane Database Syst Rev 7(4):CD004736
Czeizel AE, Dudas I (1992) Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. N Engl J Med 327(26):1832–1835
Hernandez-Diaz S, Werler MM, Walker AM, Mitchell AA (2000) Folic acid antagonists during pregnancy and the risk of birth defects. N Engl J Med 343(22):1608–1614
WHO (1992) The prevalence of anaemia in women: a tabulation of available information, 2nd edn. World Health Organization, Geneva
Milman N, Bergholt T, Byg KE, Eriksen L, Graudal N (1999) Iron status and iron balance during pregnancy. A critical re-appraisal of iron supplementation. Acta Obstet Gynecol Scand 78(9):749–757
Charles D, Ness AR, Campbell D, Davey Smith G, Hall MH (2004) Taking folate in pregnancy and risk of maternal breast cancer. BMJ 329(7479):1375–1376
Scholl OT (2005) Iron status during pregnancy: setting the stage for mother and infant. Am J Clin Nutr 81(Suppl):1218S–1222S
Ziaei S, Norrozi M, Faghihzadeh S, Jafarbegloo E (2007) A randomised placebo-controlled trial to determine the effect of iron supplementation on pregnancy outcome in pregnant women with haemoglobin > or = 13.2 g/dl. BJOG 114(6):684–688
Rolschau J, Kristoffersen K, Ulrich M, Grinsted P, Schaumburg E, Foged N (1999) The influence of folic acid supplement on the outcome of pregnancies in the county of Funen in Denmark. Part I. Eur J Obstet Gynecol Reprod Biol 87(2):105–110
Timmermans S, Jaddoe VWV, Hofman A, Steegers-Theunissen RPM, Steegers EAP (2009) Periconception folic acid supplementation, fetal growth and the risks of low birth weight and preterm birth: the Generation R Study. Br J Nutr 102(05):777–785
Pastor-Valero M, Navarrete-Munoz EM, Rebagliato M, Iniguez C, Murcia M, Marco A, Ballester F, Vioque J (2011) Periconceptional folic acid supplementation and anthropometric measures at birth in a cohort of pregnant women in Valencia, Spain. Br J Nutr 105(9):1352–1360
Chatzi L, Plana E, Daraki V, Karakosta P, Alegkakis D, Tsatsanis C, Kafatos A, Koutis A, Kogevinas M (2009) Metabolic syndrome in early pregnancy and risk of preterm birth. Am J Epidemiol 170(7):829–836
Westerway SC, Davison A, Cowell S (2000) Ultrasonic fetal measurements: new Australian standards for the new millennium. Aust N Z J Obstet Gynaecol 40(3):297–302
Goldenberg RL, Tamura T, Cliver SP, Cutter GR, Hoffman HJ, Copper RL (1992) Serum folate and fetal growth retardation: a matter of compliance? Obstet Gynecol 79(5):719–722
Carrascosa A, Yeste D, Copil A, Audi L, Gusinye M, Vicens-Calvet E, Clemente M (2004) Fetal growth regulation and intrauterine growth retardation. J Pediatr Endocrinol Metab 17(Suppl 3):435–443
Tamura T, Picciano MF (2006) Folate and human reproduction. Am J Clin Nutr 83(5):993–1016
Bailey LB, Gregory JF 3rd (1999) Folate metabolism and requirements. J Nutr 129(4):779–782
Scholl TO, Johnson WG (2000) Folic acid: influence on the outcome of pregnancy. Am J Clin Nutr 71(5):1295S–1303S
Scholl T, Hediger M, Schall J, Khoo C, Fischer R (1996) Dietary and serum folate: their influence on the outcome of pregnancy. Am J Clin Nutr 63(4):520–525
Neggers YH, Goldenberg RL, Tamura T, Cliver SP, Hoffman HJ (1997) The relationship between maternal dietary intake and infant birthweight. Acta Obstet Gynecol Scand Suppl 165:71–75
Bukowski R, Malone FD, Porter FT, Nyberg DA, Comstock CH, Hankins GD, Eddleman K, Gross SJ, Dugoff L, Craigo SD, Timor-Tritsch IE, Carr SR, Wolfe HM, D’Alton ME (2009) Preconceptional folate supplementation and the risk of spontaneous preterm birth: a cohort study. PLoS Med 6(5):e1000061
Ronnenberg AG, Goldman MB, Chen D, Aitken IW, Willett WC, Selhub J, Xu X (2002) Preconception homocysteine and B vitamin status and birth outcomes in Chinese women. Am J Clin Nutr 76(6):1385–1391
Petrakos G, Panagopoulos P, Koutras I, Kazis A, Panagiotakos D, Economou A, Kanellopoulos N, Salamalekis E, Zabelas A (2006) A comparison of the dietary and total intake of micronutrients in a group of pregnant Greek women with the dietary reference intakes. Eur J Obstet Gynecol Reprod Biol 127(2):166–171
Williams LJ, Rasmussen SA, Flores A, Kirby RS, Edmonds LD (2005) Decline in the prevalence of spina bifida and anencephaly by race/ethnicity: 1995–2002. Pediatrics 116(3):580–586
Boulet SL, Yang Q, Mai C, Kirby RS, Collins JS, Robbins JM, Meyer R, Canfield MA, Mulinare J (2008) Trends in the postfortification prevalence of spina bifida and anencephaly in the United States. Birth Defects Res A Clin Mol Teratol 82(7):527–532
Sweeney MR, Staines A, Daly L, Traynor A, Daly S, Bailey SW, Alverson PB, Ayling JE, Scott JM (2009) Persistent circulating unmetabolised folic acid in a setting of liberal voluntary folic acid fortification. Implications for further mandatory fortification? BMC Public Health 9:295
Troen AM, Mitchell B, Sorensen B, Wener MH, Johnston A, Wood B, Selhub J, McTiernan A, Yasui Y, Oral E, Potter JD, Ulrich CM (2006) Unmetabolized folic acid in plasma is associated with reduced natural killer cell cytotoxicity among postmenopausal women. J Nutr 136(1):189–194
Cole BF, Baron JA, Sandler RS, Haile RW, Ahnen DJ, Bresalier RS, McKeown-Eyssen G, Summers RW, Rothstein RI, Burke CA, Snover DC, Church TR, Allen JI, Robertson DJ, Beck GJ, Bond JH, Byers T, Mandel JS, Mott LA, Pearson LH, Barry EL, Rees JR, Marcon N, Saibil F, Ueland PM, Greenberg ER (2007) Folic acid for the prevention of colorectal adenomas: a randomized clinical trial. JAMA 297(21):2351–2359
Yajnik CS, Deshpande SS, Jackson AA, Refsum H, Rao S, Fisher DJ, Bhat DS, Naik SS, Coyaji KJ, Joglekar CV, Joshi N, Lubree HG, Deshpande VU, Rege SS, Fall CH (2008) Vitamin B12 and folate concentrations during pregnancy and insulin resistance in the offspring: the Pune Maternal Nutrition Study. Diabetologia 51(1):29–38
Lawrance AK, Deng L, Rozen R (2009) Methylenetetrahydrofolate reductase deficiency and low dietary folate reduce tumorigenesis in Apc min/+ mice. Gut 58(6):805–811
Achon M, Reyes L, Alonso-Aperte E, Ubeda N, Varela-Moreiras G (1999) High dietary folate supplementation affects gestational development and dietary protein utilization in rats. J Nutr 129(6):1204–1208
Pickell L, Brown K, Li D, Wang XL, Deng L, Wu Q, Selhub J, Luo L, Jerome-Majewska L, Rozen R (2010) High intake of folic acid disrupts embryonic development in mice. Birth Defects Res A Clin Mol Teratol 91(1):8–19
Hoyo C, Murtha AP, Schildkraut JM, Forman MR, Calingaert B, Demark-Wahnefried W, Kurtzberg J, Jirtle RL, Murphy SK (2011) Folic acid supplementation before and during pregnancy in the Newborn Epigenetics STudy (NEST). BMC Public Health 11(1):46
Institute of Medicine (2001) Dietary reference intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. National Academy Press, Washington, DC
Casanueva E, Viteri FE (2003) Iron and oxidative stress in pregnancy. J Nutr 133(5 Suppl 2):1700S–1708S
Ziaei S, Janghorban R, Shariatdoust S, Faghihzadeh S (2008) The effects of iron supplementation on serum copper and zinc levels in pregnant women with high-normal hemoglobin. Int J Gynaecol Obstet 100(2):133–135
Hemminki E, Merilainen J (1995) Long-term follow-up of mothers and their infants in a randomized trial on iron prophylaxis during pregnancy. Am J Obstet Gynecol 173(1):205–209
Acknowledgments
The study was supported by the EU Integrated Projects NewGeneris, 6th Framework Programme (Contract no. FOOD-CT-2005-016320), and Chicos, 7th Framework Programme (Contract no. Health-F2-2009-241604).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papadopoulou, E., Stratakis, N., Roumeliotaki, T. et al. The effect of high doses of folic acid and iron supplementation in early-to-mid pregnancy on prematurity and fetal growth retardation: the mother–child cohort study in Crete, Greece (Rhea study). Eur J Nutr 52, 327–336 (2013). https://doi.org/10.1007/s00394-012-0339-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-012-0339-z