Abstract
Purpose
Tethered cord syndrome (TCS) is not an uncommon clinical problem in children. The aim of this retrospective study is to document our experience on the surgical treatment of TCS in childhood.
Methods
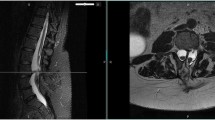
The data of 162 children who underwent surgical treatment for TCS in a 15-year period were reviewed retrospectively. Their demographic, clinical, radiological, and surgical features were documented. They were divided into two groups as primary and secondary TCS, and the surgical technique for each group was demonstrated. Untethering the spinal cord and correction of the associated malformation were the standard surgical technique for each patient. The results of the treatment were summarized.
Results
Among the 162 children, 101 (62.3 %) of them were female and 61 were male with a mean age of 62 months. Primary TCS was detected in 43 patients while secondary TCS was found in 119 (73.4 %) patients. Hypertrichosis was the most common physical finding while back pain was the common complaint. Lipoma, split cord malformation, dermal sinus tract, and myelomeningocele were the associated malformations for secondary TCS.
Conclusions
Children should be individualized for the treatment of TCS. Each patient must be evaluated neurologically and radiologically for the accurate diagnosis. Surgical untethering is the safe and effective method of treatment for children with TCS.





Similar content being viewed by others
References
Ailawadhi P, Kale SS, Agrawal D, Mahapatra AK, Kumar R (2012) Primary tethered cord syndrome—clinical and urological manifestations, diagnosis and management: a prospective study. Pediatr Neurosurg 48(4):210–215
Akay KM, Izci Y, Baysefer A (2002) Dorsal bony septum: a split cord malformation variant. Pediatr Neurosurg 36(5):225–228
Akay KM, Izci Y, Baysefer A, Timurkaynak E (2004) Split cord malformation in adults. Neurosurg Rev 27(2):99–105
Akay KM, Izci Y, Baysefer A, Timurkaynak E (2005) Composite type of split cord malformation: two different types at three different levels: case report. J Neurosurg 102(4 Suppl):436–438
Beyazova M, Zinnuroglu M, Emmez H, Kaya K, Ozkose HZ, Baykaner MK, Erden Z, Orucoglu N, Ozturk GT, Erdogan Z (2010) Intraoperative neurophysiological monitoring during surgery for tethered cord syndrome. Turk Neurosurg. 20(4):480–484
Bui CJ, Tubbs RS, Oakes WJ (2007) Tethered cord syndrome in children: a review. Neurosurg Focus 23(2):–E2
Foster KA, Lam S, Lin Y, Greene S (2014) Putative height acceleration following tethered cord release in children. J Neurosurg Pediatr. 14(6):626–634
Frainey BT, Yerkes EB, Menon VS, Gong EM, Meyer TA, Bowman RM, McLone DG, Cheng EY (2014) Predictors of urinary continence following tethered cord release in children with occult spinal dysraphism. J Pediatr Urol 10(4):627–633
Fukui J, Ohotsuka K, Asagai Y (2011) Improved symptoms and lifestyle more than 20 years after untethering surgery for primary tethered cord syndrome. Neurourol Urodyn 30(7):1333–1337
Huang SL, Peng J, Yuan GL, Ding XY, He XJ, Lan BS (2015) A new model of tethered cord syndrome produced by slow traction. Sci Rep. 5:9116
Izci Y, Gonul M, Gonul E (2007) The diagnostic value of skin lesions in split cord malformations. J Clin Neurosci 14(9):860–863
Izci Y, Pusat S, Onguru O (2011) Fatty filum with different histological features. Case report. Neurocirugia (Astur) 22(5):457–460
Izci Y, Kural C (2011) Composite type of split cord malformation: rare and difficult to explain. Pediatr Neurosurg 47(6):461
Kang JK, Yoon KJ, Ha SS, Lee IW, Jeun SS, Kang SG (2009) Surgical management and outcome of tethered cord syndrome in school-aged children, adolescents, and young adults. J Korean Neurosurg Soc 46(5):468–471
Kural C, Pusat S, Solmaz I, Kaya S, Kılıç C, Izci Y (2011) The evaluation and surgical treatment of sacral dermal sinus tracts in children. Gulhane Med J. 53(4):284–289
Kural C, Solmaz I, Pusat S, Kırık A, Kaya S, Temiz C, Izci Y (2013) Surgical technique for split cord malformations: pitfalls and solution pathways. Gulhane Med J 55(2):77–83
Kural C, Guresci S, Simsek GG, Arslan E, Tehli O, Solmaz I, Izci Y (2014) Histological structure of filum terminale in human fetuses. J Neurosurg Pediatr. 13(4):362–367
Liu FY, Li JF, Guan X, Luo XF, Wang ZL, Dang QH (2011) SEM study on filum terminale with tethered cord syndrome. Childs Nerv Syst 27(12):2141–2144
Mete M, Umur AS, Duransoy YK, Barutçuoğlu M, Umur N, Gurgen SG, Selçuki M (2014) Congenital dermal sinus tract of the spine: experience of 16 patients. J Child Neurol 29(10):1277–1282
Ostling LR, Bierbrauer KS, Kuntz 4th C (2012) Outcome, reoperation, and complications in 99 consecutive children operated for tight or fatty filum. World Neurosurg 77(1):187–191
Samuels R, McGirt MJ, Attenello FJ, Garcés Ambrossi GL, Singh N, Solakoglu C, Weingart JD, Carson BS, Jallo GI (2009) Incidence of symptomatic retethering after surgical management of pediatric tethered cord syndrome with or without duraplasty. Childs Nerv Syst 25(9):1085–1089
Selçuki M, Umur AS, Duransoy YK, Ozdemir S, Selcuki D (2012) Inappropriate surgical interventions for midline fusion defects cause secondary tethered cord symptoms: implications for natural history report of four cases. Childs Nerv Syst 28(10):1755–1760
Selçuki M, Vatansever S, Inan S, Erdemli E, Bağdatoğlu C, Polat A (2003) Is a filum terminale with a normal appearance really normal? Childs Nerv Syst 19(1):3–10
Selçuki M, Unlü A, Uğur HC, Soygür T, Arikan N, Selçuki D (2000) Patients with urinary incontinence often benefit from surgical detethering of tight filum terminale. Childs Nerv Syst 16(3):150–154
Shweikeh F, Al-Khouja L, Nuño M, Johnson JP, Drazin D, Adamo MA (2015) Disparities in clinical and economic outcomes in children and adolescents following surgery fortethered cord syndrome in the United States. J Neurosurg Pediatr 15(4):427–433
Solmaz I, Izci Y, Albayrak B, Cetinalp E, Kural C, Sengul G, Gocmez C, Pusat S, Tuzun Y (2011) Tethered cord syndrome in childhood: special emphasis on the surgical technique and review of the literature with our experience. Turk Neurosurg 21(4):516–521
Tehli O, Hodaj I, Kural C, Solmaz I, Onguru O, Izci Y (2011) A comparative study of histopathological analysis of filum terminale in patients with tethered cord syndrome and in normal human fetuses. Pediatr Neurosurg 47(6):412–416
Yamada S, Iacono RP, Andrade T, Mandybur G, Yamada BS (1995) Pathophysiology of tethered cord syndrome. Neurosurg Clin N Am 6(2):311–323
Yamada S, Won DJ, Siddiqi J, Yamada SM (2004) Tethered cord syndrome: overview of diagnosis and treatment. Neurol Res 26(7):719–721
Yamada S, Won DJ, Pezeshkpour G, Yamada BS, Yamada SM, Siddiqi J, Zouros A, Colohan AR (2007) Pathophysiology of tethered cord syndrome and similar complex disorders. Neurosurg Focus 23(2):–E6
Yener S, Thomas DT, Hicdonmez T, Dagcinar A, Bayri Y, Kaynak A, Dagli TE, Tugtepe H (2015) The effect of untethering on urologic symptoms and urodynamic parameters in children with primary tethered cord syndrome. Urology 85(1):221–226
Conflict of interests
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Geyik, M., Alptekin, M., Erkutlu, I. et al. Tethered cord syndrome in children: a single-center experience with 162 patients. Childs Nerv Syst 31, 1559–1563 (2015). https://doi.org/10.1007/s00381-015-2748-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2748-9