Abstract
Background
The objectives of this study were to assess the incidence of recurrent laryngeal nerve paralysis (RLNP) using laryngoscopy after esophagectomy for thoracic esophageal carcinoma and to clarify the risk factors influencing postoperative RLNP.
Methods
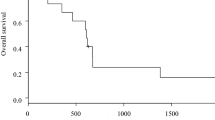
A total of 299 patients who underwent laryngoscopic examination after esophagectomy were retrospectively reviewed. Patients who were found to have postoperative RLNP were followed up every 1–3 months, with a median follow-up period of 3 months. Recovery from paralysis was also evaluated on the basis of each affected nerve. Multivariate analyses using logistic regression were used to identify independent risk factors for RLNP. Cumulative recovery rate was calculated using Kaplan–Meier method.
Results
A total of 178 (59.5 %) patients were diagnosed with RLNP by first laryngoscopy [bilateral in 59 (33.1 %) patients, right in 15 (8.4 %), and left in 104 (58.4 %)]. In 206 patients who underwent transthoracic and thoracoscopic esophagectomy, independent risk factors for RLNP were lymph node dissection along the right RLN (odds ratio [OR] 3.01, 95 % confidence interval [CI] 1.06–8.54, P = 0.04) and cervical anastomosis (OR 5.94, 95 % CI 1.78–19.80, P < 0.01). Cumulative recovery rate from RLNP was 61.7 % at 12 months after esophagectomy with 91 nerves eventually recovering from paralysis. Median recovery time was 6 months.
Conclusions
RLNP developed in 60 % of patients after esophagectomy and may be associated with lymphadenectomy around the right RLN and cervical esophageal mobilization. Although 62 % of affected nerves recovered within 12 months, great attention should be given when performing these procedures.


Similar content being viewed by others
References
Gelpke H, Grieder F, Decurtins M et al (2010) Recurrent laryngeal nerve monitoring during esophagectomy and mediastinal lymph node dissection. World J Surg 34:2379–2382. doi:10.1007/s00268-010-0692-0
Pertl L, Zacherl J, Mancusi G et al (2011) High risk of unilateral recurrent laryngeal nerve paralysis after esophagectomy using cervical anastomosis. Eur Arch Otorhinolaryngol 268:1605–1610
Gockel I, Kneist W, Keilmann A et al (2005) Recurrent laryngeal nerve paralysis (RLNP) following esophagectomy for carcinoma. Eur J Surg Oncol 31:277–281
Suda K, Ishida Y, Kawamura Y et al (2012) Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: technical report and short-term outcomes. World J Surg 36:1608–1616. doi:10.1007/s00268-012-1538-8
Noshiro H, Iwasaki H, Kobayashi K et al (2010) Lymphadenectomy along the left recurrent laryngeal nerve by a minimally invasive esophagectomy in the prone position for thoracic esophageal cancer. Surg Endosc 24:2965–2973
Nishimaki T, Suzuki T, Suzuki S et al (1998) Outcomes of extended radical esophagectomy for thoracic esophageal cancer. J Am Coll Surg 186:306–312
Baba M, Aikou T, Yoshinaka H et al (1994) Long-term results of subtotal esophagectomy with three-field lymphadenectomy for carcinoma of the thoracic esophagus. Ann Surg 219:310–316
Tachibana M, Kinugasa S, Yoshimura H et al (2005) Clinical outcomes of extended esophagectomy with three-field lymph node dissection for esophageal squamous cell carcinoma. Am J Surg 189:98–109
Fujita H, Kakegawa T, Yamana H et al (1995) Mortality and morbidity rates, postoperative course, quality of life, and prognosis after extended radical lymphadenectomy for esophageal cancer. Comparison of three-field lymphadenectomy with two-field lymphadenectomy. Ann Surg 222:654–662
Walther B, Johansson J, Johnsson F et al (2003) Cervical or thoracic anastomosis after esophageal resection and gastric tube reconstruction: a prospective randomized trial comparing sutured neck anastomosis with stapled intrathoracic anastomosis. Ann Surg 238:803–814
Yu Y, Wang Z, Liu XY et al (2010) Therapeutic efficacy comparison of two surgical procedures to treat middle thoracic esophageal carcinoma. World J Surg 34:272–276. doi:10.1007/s00268-009-0341-7
Griffin SM, Shaw IH, Dresner SM (2002) Early complications after Ivor Lewis subtotal esophagectomy with two-field lymphadenectomy: risk factors and management. J Am Coll Surg 194:285–297
Orringer MB, Marshall B, Chang AC et al (2007) Two thousand transhiatal esophagectomies: changing trends, lessons learned. Ann Surg 246:363–374
Yannopoulos P, Theodoridis P, Manes K (2009) Esophagectomy without thoracotomy: 25 years of experience over 750 patients. Langenbecks Arch Surg 394:611–616
Hulscher JB, van Sandick JW, Devriese PP et al (1999) Vocal cord paralysis after subtotal oesophagectomy. Br J Surg 86:1583–1587
Johnson PR, Kanegoanker GS, Bates T (1994) Indirect laryngoscopic evaluation of vocal cord function in patients undergoing transhiatal esophagectomy. J Am Coll Surg 178:605–608
Akiyama H, Tsurumaru M, Udagawa H et al (1994) Radical lymph node dissection for cancer of the thoracic esophagus. Ann Surg 220:364–373
Sharma S, Fujita H, Yamana H et al (1994) Patterns of lymph node metastasis in 3-field dissection for carcinoma in the thoracic esophagus. Surg Today 24:410–414
Taniyama Y, Nakamura T, Mitamura A et al (2013) A strategy for supraclavicular lymph node dissection using recurrent laryngeal nerve lymph node status in thoracic esophageal squamous cell carcinoma. Ann Thorac Surg 95:1930–1937
Nishihira T, Hirayama K, Mori S (1998) A prospective randomized trial of extended cervical and superior mediastinal lymphadenectomy for carcinoma of the thoracic esophagus. Am J Surg 175:47–51
Sobin LH, Gospodarowicz MK, Wittekind C (2009) UICC International Union Against Cancer, TNM classification of malignant tumors, 7th edn. Wiley, New York
Japan Esophageal Society (2008) Japanese Classification of Esophageal Cancer, 10th edn. Kanehara, Tokyo
Baba M, Natsugoe S, Shimada M et al (1999) Does hoarseness of voice from recurrent nerve paralysis after esophagectomy for carcinoma influence patient quality of life? J Am Coll Surg 188:231–236
Wright CD, Zeitels SM (2006) Recurrent laryngeal nerve injuries after esophagectomy. Thorac Surg Clin 16:23–33
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest that should be disclosed.
Rights and permissions
About this article
Cite this article
Sato, Y., Kosugi, Si., Aizawa, N. et al. Risk Factors and Clinical Outcomes of Recurrent Laryngeal Nerve Paralysis After Esophagectomy for Thoracic Esophageal Carcinoma. World J Surg 40, 129–136 (2016). https://doi.org/10.1007/s00268-015-3261-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-3261-8