Abstract
Background
Hepatolithiasis is a well-known risk factor of cholangiocarcinoma. Despite advances in diagnostic modalities, diagnosing cholangiocarcinoma in patients with hepatolithiasis still challenging and there are not enough reports on the incidence of cholangiocarcinoma in patient with hepatolithiasis after treatment. We aimed to evaluate the incidence and clinical characteristics of cholangiocarcinoma in patients with hepatolithiasis who underwent liver resection or non-resection.
Methods
Among a total of 257 patients who received treatment for hepatolithiasis, 236 patients were eligible for analysis. Exclusion criteria were follow-up period less than 9 months, preoperative diagnosis of cholangiocarcinoma, occurrence of cholangiocarcinoma within 1 year after treatment. Completeness of stone clearance was defined when there was no intrahepatic duct stone during whole follow-up period. A retrospective study was done to analyze the patients’ characteristics, the results and complications of the procedure, and the long-term outcomes for these patients. Kaplan–Meier method and cox proportional regression were used for statistical analysis.
Results
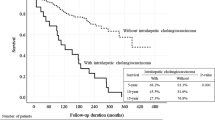
95 patients underwent hepatic resection (resection group) and 144 patients did not (non-resection group). Complete stone clearance was 71 % (67/95) in resection group and 41 % (58/141) in non-resection group (p < 0.001). The incidence of cholangiocarcinoma was 6.8 % (16/236) during follow-up period (mean 41 ± 41 months). Cholangiocarcinoma occurred 6.3 % (6/95) and 7.1 % (10/141) in resection and non-resection group, respectively. There was no significant difference in survival between two groups (p = 0.254). In analysis of according to completeness of stone clearance regardless of treatment modality, cholangiocarcinoma incidence was higher in patients with residual stone (10.4 %) than complete stone removal (3.3 %) (p = 0.263). On multivariate analysis, none of the factors (age, gender, CA19-9, stone location, bile duct stenosis, liver atrophy, stone recurrence, residual stone, and hepatic resection) showed relationship with the incidence of cholangiocarcinoma.
Conclusion
Hepatic resection for hepatolithiasis is considered to have a limited value in preventing cholangiocarcinoma and the patients should be carefully followed even after hepatic resection. A combination of different treatment modalities is necessary to decrease the residual stone and improve the outcome of the patients with hepatolithiasis.



Similar content being viewed by others
References
Tyson GL, El-Serag HB (2011) Risk factors for cholangiocarcinoma. Hepatology 54(1):173–184
Ben-Menachem T (2007) Risk factors for cholangiocarcinoma. Eur J Gastroenterol Hepatol 19(8):615–617
Lin CC, Lin PY, Chen YL (2013) Comparison of concomitant and subsequent cholangiocarcinomas associated with hepatolithiasis: clinical implications. World J Gastroenterol 19(3):375–380
Liu CL, Fan ST, Wong J (1998) Primary biliary stones: diagnosis and management. World J Surg 22(11):1162–1166. doi:10.1007/s002689900536
Su CH, Shyr YM, Lui WY, P’eng FK (1997) Hepatolithiasis associated with cholangiocarcinoma. Br J Surg 84(7):969–973
Zhou Q, Gong Y, Huang F, Lin Q, Zeng B, Li Z et al (2013) Expression Levels and Significance of Nuclear Factor-κB and Epidermal Growth Factor Receptor in Hepatolithiasis Associated with Intrahepatic Cholangiocarcinoma. Dig Surg 30(4–6):309–316
Lee KT, Chang WT, Wang SN, Chuang SC, Chai CY, Hu SW (2006) Expression of DPC4/Smad4 gene in stone-containing intrahepatic bile duct. J Surg Oncol 94(4):338–343
Kuroki T, Tajima Y, Kanematsu T (2005) Hepatolithiasis and intrahepatic cholangiocarcinoma: carcinogenesis based on molecular mechanisms. J Hepatobiliary Pancreat Surg 12(6):463–466
Park JS, Jeong S, Lee DH, Bang BW, Lee JI, Lee JW et al (2013) Risk factors for long-term outcomes after initial treatment in hepatolithiasis. J Korean Med Sci 28(11):1627–1631
Uenishi T, Hamba H, Takemura S, Oba K, Ogawa M, Yamamoto T et al (2009) Outcomes of hepatic resection for hepatolithiasis. Am J Surg 198(2):199–202
Hur H, Park IY, Sung GY, Lee DS, Kim W, Won JM (2009) Intrahepatic cholangiocarcinoma associated with intrahepatic duct stones. Asian J Surg 32(1):7–12
Uchiyama K, Kawai M, Ueno M, Ozawa S, Tani M, Yamaue H (2007) Reducing residual and recurrent stones by hepatectomy for hepatolithiasis. J Gastrointest Surg 11(5):626–630
Cheung MT, Kwok PC (2005) Liver resection for intrahepatic stones. Arch Surg 140(10):993–997
Chen DW, Tung-Ping R, Liu CL, Fan ST, Wong J (2004) Immediate and longterm outcomes of hepatectomy for hepatolithiasis. Surgery 135(4):386–393
Cai X, Wang Y, Yu H, Liang X, Peng S (2007) Laparoscopic hepatectomy for hepatolithiasis: a feasibility and safety study in 29 patients. Surg Endosc 21(7):1074–1078
Chijiiwa K, Ichimiya H, Kuroki S, Koga A, Nakayama F (1993) Late development of cholangiocarcinoma after the treatment of hepatolithiasis. Surg Gynecol Obstet 177(3):279–282
Sheen-Chen SM, Chou FF, Eng HL (1991) Intrahepatic cholangiocarcinoma in hepatolithiasis: a frequently overlooked disease. J Surg Oncol 47(2):131–135
Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS (2009) Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery 146(5):843–853
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, H.J., Kim, J.S., Suh, S.J. et al. Cholangiocarcinoma Risk as Long-term Outcome After Hepatic Resection in the Hepatolithiasis Patients. World J Surg 39, 1537–1542 (2015). https://doi.org/10.1007/s00268-015-2965-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-015-2965-0