Abstract
Background
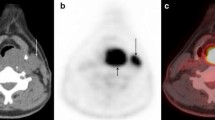
The aim of this study was to evaluate the accuracy of [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography, ultrasonography, and enhanced computed tomography alone in the preoperative diagnosis of lymph node metastasis in patients with papillary thyroid carcinoma.
Methods
In a prospective study performed between January 2007 and December 2009, 74 patients with a diagnosis of papillary thyroid carcinoma confirmed by fine-needle aspiration biopsy were referred to our institution for surgery. Preoperative assessment of metastasis in the central and lateral cervical lymph nodes was done using [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography, ultrasonography, and enhanced computed tomography. The results for each level of cervical node assessed using these methods were correlated with the pathology reports after surgery. We determined the sensitivity, specificity, positive and negative predictive values, and diagnostic accuracy of the three methods for all levels of cervical lymph node.
Results
There were no significant differences in the diagnostic results obtained by [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography and enhanced computed tomography. However, ultrasonography images gave significantly better results than either [18F]-fluoro-2-deoxy-d-glucose-positron emission tomography/computed tomography or enhanced computed tomography alone in identifying metastases on the basis of the level of cervical lymph node. In addition, the overall diagnostic accuracy tended to be higher for the lateral compartment than for the central compartment.
Conclusions
Preoperative assessment by ultrasonography of metastases in the central and lateral cervical lymph nodes might be the best methodology for determining the extent of surgical resection required to remove metastatic lymph nodes adequately in patients with papillary thyroid carcinoma.



Similar content being viewed by others
References
Gilliland FD, Hunt WC, Morris DM et al (1997) Prognostic factors for thyroid carcinoma: a population-based study of 15, 698 cases from the Surveillance, Epidemiology and End Results (SEER) program 1973–1991. Cancer 79:564–573
Clark OH (1996) Predictors of thyroid tumor aggressiveness. West J Med 165:131–138
Grebe SK, Hay ID (1996) Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 5:43–63
Mazzaferri EL, Kloos RT (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. J Clin Endocrinol Metab 86:1447–1463
Noguchi S, Murakami N (1987) The value of lymph-node dissection in patients with differentiated thyroid cancer. Surg Clin North Am 24:325–330
Lee BJ, Wang SG, Lee JC et al (2007) Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 133:1028–1030
Cooper DS, Doherty GM, Haugen BR et al (2006) American Thyroid Association Guidelines Taskforce. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16:109–142
Langer JE, Mandel SJ (2008) Sonographic imaging of cervical lymph nodes in patients with thyroid cancer. Neuroimaging Clin N Am 18:479–489
McGuirt WF, Williams DW 3rd, Keyes JW Jr et al (1995) A comparative diagnostic study of head and neck nodal metastases using positron emission tomography. Laryngoscope 105:373–375
Bochuslavitzki KH, Klutmann S, Kröger S et al (2000) FDG PET detection of unknown primary tumors. J Nucl Med 41:816–822
Frilling A, Tecklenborg K, Gorges R et al (2001) Preoperative diagnostic value of 18fluorodeoxyglucose positron emission tomography in patients with radioiodine-negative recurrent well-differentiated thyroid carcinoma. Ann Surg 234:804–811
Stokkel MP, ten Broek FW, Hordijk GJ et al (2000) Postoperative evaluation of patients with primary head and neck cancer using dual-head 18fluoro-deoxyglucose positron emission tomography. Ann Surg 231:229–234
Jeong HS, Baek CH, Son YI et al (2007) Use of integrated 18F-FDG PET/CT to improve the accuracy of initial cervical nodal evaluation in patients with head and neck squamous cell carcinoma. Head Neck 29:203–210
Jeong HS, Baek CH, Son YI et al (2006) Integrated 18F-FDG PET/CT for the initial evaluation of cervical node level of patients with papillary thyroid carcinoma: comparison with ultrasound and contrast-enhanced CT. Clin Endocrinol (Oxf) 65:402–407
Robbins KT, Clayman G, Lavine PA et al (2002) Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg 128:751–758
Bhattacharyya N (2003) Surgical treatment of cervical nodal metastases in patients with papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg 129:1101–1104
Noguchi S, Murakami N, Yamashita H (1998) Papillary thyroid carcinoma: modified radical neck dissection improves prognosis. Arch Surg 133:276–280
Fish SA, Langer JE, Mandel SJ (2008) Sonographic imaging of thyroid nodules and cervical lymph nodes. Endocrinol Metab Clin North Am 37:401–417
Ahn JE, Lee JH, Yi JS et al (2008) Diagnostic accuracy of CT and ultrasonography for evaluating metastatic cervical lymph nodes in patients with thyroid cancer. World J Surg 32:1552–1558
Kouvaraki MA, Shapiro SE, Fornage BD et al (2003) Role of preoperative ultrasonography in surgical management of patients with thyroid cancer. Surgery 134:946–954; discussion 954–955
Caron NR, Tan YY, Ogilvie JB et al (2006) Selective modified radical neck dissection for papillary thyroid cancer-is level I, II and V dissection always necessary? World J Surg 30:833–840
Köybasioglu A, Tokcaer AB, Uslu S et al (2000) Accessory nerve function after modified radical and lateral neck dissection. Laryngoscope 110:73–77
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Morita, S., Mizoguchi, K., Suzuki, M. et al. The Accuracy of 18[F]-Fluoro-2-Deoxy-d-Glucose-Positron Emission Tomography/Computed Tomography, Ultrasonography, and Enhanced Computed Tomography Alone in the Preoperative Diagnosis of Cervical Lymph Node Metastasis in Patients with Papillary Thyroid Carcinoma. World J Surg 34, 2564–2569 (2010). https://doi.org/10.1007/s00268-010-0733-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-010-0733-8