Abstract
Purpose
To assess the differences in early imaging features and progression pattern on CT between intrahepatic biliary metastasis (IBM) and non-mass-forming cholangiocarcinoma (NMFC) in patients with extrabiliary malignancy.
Methods
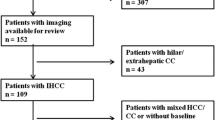
This retrospective study included 35 patients who were surgically and pathologically confirmed with IBM (n = 14) or NMFC (n = 21) at the time of or after surgery for extrabiliary malignancy. Two observers evaluated the following aspects of biliary lesions on initial or follow-up CT images: location, characteristics of intrahepatic duct (IHD) dilatation, presence of duct wall thickening, and periductal infiltration lesion or periductal expansile mass.
Results
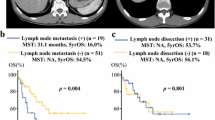
All IBMs were associated with colorectal cancer (p = 0.032). As early imaging features on CT, smooth tapered localized IHD dilatation without duct wall thickening and peripheral duct involvement were observed significantly more often in IBM, and IHD dilatation with abrupt tapering or irregularity of transition site and bile duct wall thickening were significantly more common in NMFC (all p < 0.05). Regarding progression pattern, periductal expansile mass was present only in IBM, whereas periductal infiltrative lesion was present only in NMFC (p < 0.001).
Conclusion
In the differentiation between IBM and NMFC in patients with extrabiliary malignancy, the differences in early imaging features and progression pattern of the two diseases revealed in this study would be helpful for diagnosis.





Similar content being viewed by others
Abbreviations
- IBM:
-
Intrahepatic biliary metastasis
- NMFC:
-
Non-mass-forming cholangiocarcinoma
- IHD:
-
Intrahepatic duct
- CCC:
-
Cholangiocarcinoma
- CEA:
-
Carcinoembryonic antigen
- CA19-9:
-
Carbohydrate antigen 19-9
- TNM:
-
Tumor, node, metastases
- PACS:
-
Picture archiving and communication system
References
Iwasaki M, Furuse J, Yoshino M, et al. (1996) Percutaneous transhepatic biliary drainage for the treatment of obstructive jaundice caused by metastases from nonbiliary and nonpancreatic cancers. Jpn J Clin Oncol 26:465–468
Lee YJ, Kim SH, Lee JY, et al. (2009) Differential CT features of intraductal biliary metastasis and double primary intraductal polypoid cholangiocarcinoma in patients with a history of extrabiliary malignancy. AJR Am J Roentgenol 193:1061–1069. https://doi.org/10.2214/ajr.08.2089
Estrella JS, Othman ML, Taggart MW, et al. (2013) Intrabiliary growth of liver metastases: clinicopathologic features, prevalence, and outcome. Am J Surg Pathol 37:1571–1579. https://doi.org/10.1097/PAS.0b013e318293ddf1
Kawashima K, Watanabe N, Tawada S, et al. (2017) Intrahepatic biliary metastasis of colonic adenocarcinoma: A case report with immunohistochemical analysis. World J Oncol 8:86–91. https://doi.org/10.14740/wjon1037w
Peungjesada S, Aloia TA, Kaur H, et al. (2013) Intrabiliary growth of colorectal liver metastasis: spectrum of imaging findings and implications for surgical management. AJR Am J Roentgenol 201:W582–W589. https://doi.org/10.2214/ajr.12.9508
Adam R, De Gramont A, Figueras J, et al. (2012) The oncosurgery approach to managing liver metastases from colorectal cancer: a multidisciplinary international consensus. Oncologist 17:1225–1239. https://doi.org/10.1634/theoncologist.2012-0121
Adam R, Yi B, Innominato PF, et al. (2017) Resection of colorectal liver metastases after second-line chemotherapy: is it worthwhile? A LiverMetSurvey analysis of 6415 patients. Eur J Cancer 78:7–15. https://doi.org/10.1016/j.ejca.2017.03.009
Chung YE, Kim MJ, Park YN, et al. (2009) Varying appearances of cholangiocarcinoma: radiologic-pathologic correlation. Radiographics 29:683–700. https://doi.org/10.1148/rg.293085729
Lim JH, Mairiang E, Ahn GH (2008) Biliary parasitic diseases including clonorchiasis, opisthorchiasis and fascioliasis. Abdom Imaging 33:157–165. https://doi.org/10.1007/s00261-007-9326-x
Riopel MA, Klimstra DS, Godellas CV, Blumgart LH, Westra WH (1997) Intrabiliary growth of metastatic colonic adenocarcinoma: a pattern of intrahepatic spread easily confused with primary neoplasia of the biliary tract. Am J Surg Pathol 21:1030–1036
Sugiura T, Nagino M, Oda K, et al. (2006) Hepatectomy for colorectal liver metastases with macroscopic intrabiliary tumor growth. World J Surg 30:1902–1908. https://doi.org/10.1007/s00268-006-0205-3
Kubo M, Sakamoto M, Fukushima N, et al. (2002) Less aggressive features of colorectal cancer with liver metastases showing macroscopic intrabiliary extension. Pathol Int 52:514–518
Lim JH (2003) Cholangiocarcinoma: morphologic classification according to growth pattern and imaging findings. AJR Am J Roentgenol 181:819–827. https://doi.org/10.2214/ajr.181.3.1810819
Colagrande S, Batignani G, Messerini L, Pinzani M (2004) Intrabiliary metastasis from rectal cancer mimicking peripheral papillary-type cholangiocarcinoma. J Hepatol 41:172–174. https://doi.org/10.1016/j.jhep.2004.03.027
Ghittoni G, Caturelli E, Viera FT (2010) Intrabile duct metastasis from colonic adenocarcinoma without liver parenchyma involvement: contrast enhanced ultrasonography detection. Abdom Imaging 35:346–348. https://doi.org/10.1007/s00261-009-9510-2
Povoski SP, Klimstra DS, Brown KT, et al. (2000) Recognition of intrabiliary hepatic metastases from colorectal adenocarcinoma. HPB Surg 11:383–390
Takamatsu S, Teramoto K, Kawamura T, et al. (2004) Liver metastasis from rectal cancer with prominent intrabile duct growth. Pathol Int 54:440–445. https://doi.org/10.1111/j.1440-1827.2004.01636.x
Uehara K, Hasegawa H, Ogiso S, et al. (2004) Intrabiliary polypoid growth of liver metastasis from colonic adenocarcinoma with minimal invasion of the liver parenchyma. J Gastroenterol 39:72–75. https://doi.org/10.1007/s00535-002-1248-3
Yamao T, Hayashi H, Higashi T, et al. (2015) Colon cancer metastasis mimicking intraductal papillary neoplasm of the extra-hepatic bile duct. Int J Surg Case Rep 10:91–93. https://doi.org/10.1016/j.ijscr.2015.01.053
Acknowledgements
We appreciate Prof. Cheol Keun Park and Prof. Kee Taek Jang for their histopathologic analysis.
Funding
We declare no sources of financial support or funding received from any organization including National Institutes of Health (NIH); Wellcome Trust; Howard Hughes Medical Institute (HHMI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors (Ji Hye Min, Kyung Mi Jang, Dong Ik Cha, Tae Wook Kang, Seong Hyun Kim, Seo-Youn Choi, and Kwangseon Min) declare no conflict of interest.
Ethical approval
Research involving human participants and/or animals: Research involving human participants. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
This retrospective study was approved by our institutional review board, and the requirement for informed consent was waived.
Rights and permissions
About this article
Cite this article
Min, J.H., Jang, K.M., Cha, D.I. et al. Differences in early imaging features and pattern of progression on CT between intrahepatic biliary metastasis of colorectal origin and intrahepatic non-mass-forming cholangiocarcinoma in patients with extrabiliary malignancy. Abdom Radiol 44, 1350–1360 (2019). https://doi.org/10.1007/s00261-018-1814-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1814-7