Abstract
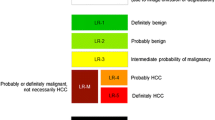
The Liver Imaging Reporting and Data System (LI-RADS) uses an algorithm to assign categories that reflect the probability of hepatocellular carcinoma (HCC), non-HCC malignancy, or benignity. Unlike other imaging algorithms, LI-RADS utilizes ancillary features (AFs) to refine the final category. AFs in LI-RADS v2017 are divided into those favoring malignancy in general, those favoring HCC specifically, and those favoring benignity. Additionally, LI-RADS v2017 provides new rules regarding application of AFs. The purpose of this review is to discuss ancillary features included in LI-RADS v2017, the rationale for their use, potential pitfalls encountered in their interpretation, and tips on their application.




















Similar content being viewed by others
Abbreviations
- AF:
-
Ancillary features
- AASLD:
-
American Association for the Study of Liver Diseases
- ADC:
-
Apparent diffusion coefficient
- APHE:
-
Arterial phase hyperenhancement
- CT:
-
Computed tomography
- DWI:
-
Diffusion-weighted imaging
- ECA:
-
Extracellular agents
- HCC:
-
Hepatocellular carcinoma
- HBP:
-
Hepatobiliary phase
- LI-RADS:
-
Liver Imaging Reporting And Data System
- MRI:
-
Magnetic resonance imaging
- US:
-
Ultrasound
- OPTN:
-
ORGAN Procurement and Transplantation Network
- PVP:
-
Portal venous phase
- TP:
-
Transitional phase
- TVDT:
-
Tumor volume doubling time
References
Wald C, Russo MW, Heimbach JK, et al. (2013) New OPTN/UNOS policy for liver transplant allocation: standardization of liver imaging, diagnosis, classification, and reporting of hepatocellular carcinoma. Radiology 266(2):376–382
Bruix J, Sherman M (2011) Management of hepatocellular carcinoma: an update. Hepatology 53(3):1020–1032
EASL-EORTC clinical practice guidelines (2012) management of hepatocellular carcinoma. J Hepatol 56(4):908–943
Omata M, Lesmana LA, Tateishi R, et al. (2010) Asian Pacific Association for the Study of the Liver consensus recommendations on hepatocellular carcinoma. Hepatol Int 4(2):439–474
Kudo M, Matsui O, Izumi N, et al. (2014) JSH consensus-based clinical practice guidelines for the management of hepatocellular carcinoma: 2014 update by the liver cancer study group of Japan. Liver Cancer 3(3–4):458–468
Wilson; Kono Y. LI-RADS algorithm: CEUS. Abdom Radiol 2017.
Darnell A, Forner A, Rimola J, et al. (2015) Liver imaging reporting and data system with MR imaging: evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology 275(3):698–707
Okada S, Okazaki N, Nose H, et al. (1993) Follow-up examination schedule of postoperative HCC patients based on tumor volume doubling time. Hepato-gastroenterology 40(4):311–315
Kubota K, Ina H, Okada Y, Irie T (2003) Growth rate of primary single hepatocellular carcinoma: determining optimal screening interval with contrast enhanced computed tomography. Dig Dis Sci 48(3):581–586
Furlan A, Marin D, Agnello F, et al. (2012) Hepatocellular carcinoma presenting at contrast-enhanced multi-detector-row computed tomography or gadolinium-enhanced magnetic resonance imaging as a small (</ = 2 cm), indeterminate nodule: growth rate and optimal interval time for imaging follow-up. J Comp Assist Tomogr 36(1):20–25
Taouli B, Goh JS, Lu Y, et al. (2005) Growth rate of hepatocellular carcinoma: evaluation with serial computed tomography or magnetic resonance imaging. J Comp Assist Tomogr 29(4):425–429
Park Y, Choi D, Lim HK, et al. (2008) Growth rate of new hepatocellular carcinoma after percutaneous radiofrequency ablation: evaluation with multiphase CT. AJR Am J Roentgenol 191(1):215–220
Miyayama S, Yamashiro M, Okuda M, et al. (2011) Detection of corona enhancement of hypervascular hepatocellular carcinoma by C-arm dual-phase cone-beam CT during hepatic arteriography. Cardiovasc Interv Radiol 34(1):81–86
Ueda K, Matsui O, Kawamori Y, et al. (1998) Hypervascular hepatocellular carcinoma: evaluation of hemodynamics with dynamic CT during hepatic arteriography. Radiology 206(1):161–166
Terayama N, Matsui O, Ueda K, et al. (2002) Peritumoral rim enhancement of liver metastasis: hemodynamics observed on single-level dynamic CT during hepatic arteriography and histopathologic correlation. J Comput Assist Tomogr 26(6):975–980
Kitao A, Zen Y, Matsui O, Gabata T, Nakanuma Y (2009) Hepatocarcinogenesis: multistep changes of drainage vessels at CT during arterial portography and hepatic arteriography–radiologic–pathologic correlation. Radiology 252(2):605–614
Santillan C FK, Kono Y, Chernyak V. LI-RADS major features: CT, MRI with ECA, and MRI with HBA. Abdom Radiol 2017.
Bruegel M, Holzapfel K, Gaa J, et al. (2008) Characterization of focal liver lesions by ADC measurements using a respiratory triggered diffusion-weighted single-shot echo-planar MR imaging technique. Eur Radiol 18(3):477–485
Taouli B, Vilgrain V, Dumont E, et al. (2003) Evaluation of liver diffusion isotropy and characterization of focal hepatic lesions with two single-shot echo-planar MR imaging sequences: prospective study in 66 patients. Radiology 226(1):71–78
Le Moigne F, Durieux M, Bancel B, et al. (2012) Impact of diffusion-weighted MR imaging on the characterization of small hepatocellular carcinoma in the cirrhotic liver. Magn Reson Imaging 30(5):656–665
Xu PJ, Yan FH, Wang JH, et al. (2010) Contribution of diffusion-weighted magnetic resonance imaging in the characterization of hepatocellular carcinomas and dysplastic nodules in cirrhotic liver. J Comput Assist Tomogr 34(4):506–512
Kwon HJ, Byun JH, Kim JY, et al. (2015) Differentiation of small (</ = 2 cm) hepatocellular carcinomas from small benign nodules in cirrhotic liver on gadoxetic acid-enhanced and diffusion-weighted magnetic resonance images. Abdom Imaging 40(1):64–75
Nasu K, Kuroki Y, Tsukamoto T, et al. (2009) Diffusion-weighted imaging of surgically resected hepatocellular carcinoma: imaging characteristics and relationship among signal intensity, apparent diffusion coefficient, and histopathologic grade. AJR Am J Roentgenol 193(2):438–444
Hwang J, Kim YK, Park MJ, et al. (2012) Differentiating combined hepatocellular and cholangiocarcinoma from mass-forming intrahepatic cholangiocarcinoma using gadoxetic acid-enhanced MRI. J Magn Reson Imaging 36(4):881–889
Kim YK, Lee WJ, Park MJ, et al. (2012) Hypovascular hypointense nodules on hepatobiliary phase gadoxetic acid-enhanced MR images in patients with cirrhosis: potential of DW imaging in predicting progression to hypervascular HCC. Radiology 265(1):104–114
Taouli B, Koh DM (2010) Diffusion-weighted MR imaging of the liver. Radiology 254(1):47–66
Park HJ, Kim YK, Park MJ, Lee WJ (2013) Small intrahepatic mass-forming cholangiocarcinoma: target sign on diffusion-weighted imaging for differentiation from hepatocellular carcinoma. Abdom Imaging. 38(4):793–801
Di Martino M, Anzidei M, Zaccagna F, et al. (2016) Qualitative analysis of small (</ = 2 cm) regenerative nodules, dysplastic nodules and well-differentiated HCCs with gadoxetic acid MRI. BMC Med Imaging 16(1):62
Li CS, Chen RC, Lii JM, et al. (2006) Magnetic resonance imaging appearance of well-differentiated hepatocellular carcinoma. J Comput Assist Tomogr 30(4):597–603
Rhee H, Kim MJ, Park YN, Choi JS, Kim KS (2012) Gadoxetic acid-enhanced MRI findings of early hepatocellular carcinoma as defined by new histologic criteria. J Magn Reson Imaging 35(2):393–398
Kelekis NL, Semelka RC, Worawattanakul S, et al. (1998) Hepatocellular carcinoma in North America: a multiinstitutional study of appearance on T1-weighted, T2-weighted, and serial gadolinium-enhanced gradient-echo images. AJR Am J Roentgenol 170(4):1005–1013
Enomoto S, Tamai H, Shingaki N, et al. (2011) Assessment of hepatocellular carcinomas using conventional magnetic resonance imaging correlated with histological differentiation and a serum marker of poor prognosis. Hepatol Int 5(2):730–737
van den Bos IC, Hussain SM, Dwarkasing RS, et al. (2007) MR imaging of hepatocellular carcinoma: relationship between lesion size and imaging findings, including signal intensity and dynamic enhancement patterns. J Magn Reson Imaging 26(6):1548–1555
Ebara M, Fukuda H, Kojima Y, et al. (1999) Small hepatocellular carcinoma: relationship of signal intensity to histopathologic findings and metal content of the tumor and surrounding hepatic parenchyma. Radiology 210(1):81–88
Kamura T, Kimura M, Sakai K, et al. (2002) Small hypervascular hepatocellular carcinoma versus hypervascular pseudolesions: differential diagnosis on MRI. Abdom Imaging. 27(3):315–324
Hyodo T, Murakami T, Imai Y, et al. (2013) Hypovascular nodules in patients with chronic liver disease: risk factors for development of hypervascular hepatocellular carcinoma. Radiology 266(2):480–490
Jha RC, Zanello PA, Nguyen XM, et al. (2014) Small hepatocellular carcinoma: MRI findings for predicting tumor growth rates. Acad Radiol 21(11):1455–1464
Rosenkrantz AB, Lee L, Matza BW, Kim S (2012) Infiltrative hepatocellular carcinoma: comparison of MRI sequences for lesion conspicuity. Clin Radiol 67(12):e105–e111
Cruite I, Schroeder M, Merkle EM, Sirlin CB (2010) Gadoxetate disodium-enhanced MRI of the liver: part 2, protocol optimization and lesion appearance in the cirrhotic liver. AJR Am J Roentgenol 195(1):29–41
Lee MH, Kim SH, Park MJ, Park CK, Rhim H (2011) Gadoxetic acid-enhanced hepatobiliary phase MRI and high-b-value diffusion-weighted imaging to distinguish well-differentiated hepatocellular carcinomas from benign nodules in patients with chronic liver disease. AJR Am J Roentgenol 197(5):W868–W875
Choi SH, Byun JH, Lim YS, et al. (2016) Diagnostic criteria for hepatocellular carcinoma 3 cm with hepatocyte-specific contrast-enhanced magnetic resonance imaging. J Hepatol 64(5):1099–1107
Bartolozzi C, Battaglia V, Bargellini I, et al. (2013) Contrast-enhanced magnetic resonance imaging of 102 nodules in cirrhosis: correlation with histological findings on explanted livers. Abdom Imaging 38(2):290–296
Cortis K, Liotta R, Miraglia R, et al. (2016) Incorporating the hepatobiliary phase of gadobenate dimeglumine-enhanced MRI in the diagnosis of hepatocellular carcinoma: increasing the sensitivity without compromising specificity. Acta Radiol 57(8):923–931
Orlacchio A, Chegai F, Fabiano S, et al. (2016) Role of MRI with hepatospecific contrast agent in the identification and characterization of focal liver lesions: pathological correlation in explanted livers. La Radiol Med 121(7):588–596
Hope TA, Fowler KJ, Sirlin CB, et al. (2015) Hepatobiliary agents and their role in LI-RADS. Abdom Imaging 40(3):613–625
An C, Rhee H, Han K, et al. (2016) Added value of smooth hypointense rim in the hepatobiliary phase of gadoxetic acid-enhanced MRI in identifying tumour capsule and diagnosing hepatocellular carcinoma. Eur Radiol 27:2610–2618
Dioguardi Burgio M, Picone D, Cabibbo G, et al. (2016) MR-imaging features of hepatocellular carcinoma capsule appearance in cirrhotic liver: comparison of gadoxetic acid and gadobenate dimeglumine. Abdom Radiol 41:1546–1554
Suh YJ, Kim MJ, Choi JY, et al. (2011) Differentiation of hepatic hyperintense lesions seen on gadoxetic acid-enhanced hepatobiliary phase MRI. AJR Am J Roentgenol 197(1):W44–W52
Chong YS, Kim YK, Lee MW, et al. (2012) Differentiating mass-forming intrahepatic cholangiocarcinoma from atypical hepatocellular carcinoma using gadoxetic acid-enhanced MRI. Clin Radiol 67(8):766–773
Kim R, Lee JM, Shin CI, et al. (2016) Differentiation of intrahepatic mass-forming cholangiocarcinoma from hepatocellular carcinoma on gadoxetic acid-enhanced liver MR imaging. Eur Radiol 26(6):1808–1817
Stevens WR, Gulino SP, Batts KP, Stephens DH, Johnson CD (1996) Mosaic pattern of hepatocellular carcinoma: histologic basis for a characteristic CT appearance. J Comput Assist Tomogr 20(3):337–342
Choi BI, Takayasu K, Han MC (1993) Small hepatocellular carcinomas and associated nodular lesions of the liver: pathology, pathogenesis, and imaging findings. AJR Am J Roentgenol 160(6):1177–1187
Yoshida T, Matsue H, Okazaki N, Yoshino M (1987) Ultrasonographic differentiation of hepatocellular carcinoma from metastatic liver cancer. J Clin Ultrasound 15(7):431–437
Kutami R, Nakashima Y, Nakashima O, Shiota K, Kojiro M (2000) Pathomorphologic study on the mechanism of fatty change in small hepatocellular carcinoma of humans. J Hepatol 33(2):282–289
Park HJ, Jang KM, Kang TW, et al. (2016) Identification of imaging predictors discriminating different primary liver tumours in patients with chronic liver disease on gadoxetic acid-enhanced MRI: a classification tree analysis. Eur Radiol 26(9):3102–3111
Sheng RF, Zeng MS, Ji Y, et al. (2015) MR features of small hepatocellular carcinoma in normal, fibrotic, and cirrhotic livers: a comparative study. Abdom Imaging 40(8):3062–3069
Ebara M, Hatano R, Fukuda H, et al. (1998) Natural course of small hepatocellular carcinoma with underlying cirrhosis. A study of 30 patients. Hepato-gastroenterology 45(Suppl 3):1214–1220
Yamagata M, Masaki T, Okudaira T, et al. (1999) Small hyperechoic nodules in chronic liver diseases include hepatocellular carcinomas with low cyclin D1 and Ki-67 expression. Hepatology 29(6):1722–1729
Huz JI, Melis M, Sarpel U (2012) Spontaneous regression of hepatocellular carcinoma is most often associated with tumour hypoxia or a systemic inflammatory response. HPB 14(8):500–505
Tamada T, Ito K, Yamamoto A, et al. (2011) Hepatic hemangiomas: evaluation of enhancement patterns at dynamic MRI with gadoxetate disodium. AJR Am J Roentgenol 196(4):824–830
Kim B, Byun JH, Kim HJ, et al. (2016) Enhancement patterns and pseudo-washout of hepatic haemangiomas on gadoxetate disodium-enhanced liver MRI. Eur Radiol 26(1):191–198
Brancatelli G, Federle MP, Blachar A, Grazioli L (2001) Hemangioma in the cirrhotic liver: diagnosis and natural history. Radiology 219(1):69–74
Krinsky GA, Lee VS, Nguyen MT, et al. (2000) Siderotic nodules at MR imaging: regenerative or dysplastic? J Comput Assist Tomogr 24(5):773–776
Krinsky GA, Zivin SB, Thorner KM, et al. (2002) Low-grade siderotic dysplastic nodules: determination of premalignant lesions on the basis of vasculature phenotype. Acad Radiol 9(3):336–341
Zhang J, Krinsky GA (2004) Iron-containing nodules of cirrhosis. NMR Biomed 17(7):459–464
Krinsky GA, Lee VS, Nguyen MT, et al. (2001) Siderotic nodules in the cirrhotic liver at MR imaging with explant correlation: no increased frequency of dysplastic nodules and hepatocellular carcinoma. Radiology 218(1):47–53
Ringe KI, Husarik DB, Sirlin CB, Merkle EM (2010) Gadoxetate disodium-enhanced MRI of the liver: part 1, protocol optimization and lesion appearance in the noncirrhotic liver. AJR Am J Roentgenol 195(1):13–28
Ahn SJ, Kim MJ, Hong HS, Kim KA, Song HT (2011) Distinguishing hemangiomas from malignant solid hepatic lesions: a comparison of heavily T2-weighted images obtained before and after administration of gadoxetic acid. J Magn Resone Imaging 34(2):310–317
Del Poggio P, Buonocore M (2008) Cystic tumors of the liver: a practical approach. World J Gastroenterol 14(23):3616–3620
Silva AC, Evans JM, McCullough AE, et al. (2009) MR imaging of hypervascular liver masses: a review of current techniques. Radiographics 29(2):385–402
Ahn JH, Yu JS, Hwang SH, et al. (2010) Nontumorous arterioportal shunts in the liver: CT and MRI findings considering mechanisms and fate. Eur Radiol 20(2):385–394
Kim JI, Lee JM, Choi JY, et al. (2008) The value of gadobenate dimeglumine-enhanced delayed phase MR imaging for characterization of hepatocellular nodules in the cirrhotic liver. Investig Radiol. 43(3):202–210
Acknowledgements
This work was supported by [1] the Fonds de recherche du Québec—Santé (Career Award#26993), and New Researcher Startup Grant from the Centre de Recherche du Centre Hospitalier de l’Université de Montréal (CRCHUM) to An Tang.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V Chernyak, M. Flusberg, D. Papadatos, B. Bijan, C. Santillan: None. A. Tang, MD, MSc: Advisory board member of Imagia Cybernetics. Y. Kono: Research Grant support: Toshiba Medical Systems Co.; Contrast agent support: Lantheus Medical Imaging Inc.; Equipment support: GE Healthcare; Equipment support: Philips Ultrasound.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Chernyak, V., Tang, A., Flusberg, M. et al. LI-RADS® ancillary features on CT and MRI. Abdom Radiol 43, 82–100 (2018). https://doi.org/10.1007/s00261-017-1220-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1220-6