Abstract
Summary
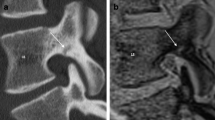
This study demonstrated the predictive values of radiological findings for delayed union after osteoporotic vertebral fractures (OVFs). High-signal changes on T2WI were useful findings.
Introduction
The purpose of the present study is to determine predictive radiological findings for delayed union by magnetic resonance imaging (MRI) and plain X-rays at two time points in the acute phase of OVFs.
Methods
This multicenter cohort study was performed from 2012 to 2015. A total of 218 consecutive patients with OVFs ≤2 weeks old were enrolled. MRIs and plain X-rays were performed at the time of enrollment and at 1- and 6-month follow-ups. Signal changes on T1-weighted imaging (T1WI) were classified as diffuse low-, confined low-, or no-signal change; those on T2WI were classified as high (similar to the intensity of cerebrospinal fluid), confined low-, diffuse low-, or no-signal change. The angular motion of the fractured vertebral body was measured with X-rays.
Results
A total of 153 patients completed the 6-month follow-up. A high-signal change on T2WI was most useful in predicting delayed union. Sensitivity, specificity, and positive predictive values were 53.3, 87.8, and 51.6 % at enrollment and 65.5, 84.8, and 51.4 % at the 1-month follow-up, respectively. The positive predictive value increased to 62.5 % with observation of high- or diffuse low-signal changes at both enrollment and the 1-month follow-up. The cutoff value of vertebral motion was 5 degrees. Sensitivity and specificity at enrollment were 52.4 and 74.1 %, respectively.
Conclusions
This study demonstrated the radiological factors predicting delayed union after an OVF. T2 high-signal changes showed the strongest association with delayed union. Consecutive MRIs were particularly useful as a differential tool to predict delayed union following OVFs.





Similar content being viewed by others
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726–1733
Black DM, Cummings SR, Karpf DB, et al. (1996) Randomised trial of effect of alendronate on risk of fracture in women with existing vertebral fractures. Fracture Intervention Trial Research Group. Lancet (London, England) 348:1535–1541
Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ (1992) Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 7:221–227
Gold DT (2001) The nonskeletal consequences of osteoporotic fractures. Psychologic and social outcomes. Rheum Dis Clin N Am 27:255–262
Rao RD, Singrakhia MD (2003) Painful osteoporotic vertebral fracture. Pathogenesis, evaluation, and roles of vertebroplasty and kyphoplasty in its management. J Bone Joint Surg Am 85-A:2010–2022
Suzuki N, Ogikubo O, Hansson T (2008) The course of the acute vertebral body fragility fracture: its effect on pain, disability and quality of life during 12 months. Eur Spine J 17:1380–1390
Matsumoto T, Hoshino M, Tsujio T, et al. (2012) Prognostic factors for reduction of activities of daily living following osteoporotic vertebral fractures. Spine (Phila Pa 1976) 37:1115–1121
Hasegawa K, Homma T, Uchiyama S, Takahashi H (1998) Vertebral pseudarthrosis in the osteoporotic spine. Spine (Phila Pa 1976) 23:2201–2206
Hoshino M, Nakamura H, Terai H, et al. (2009) Factors affecting neurological deficits and intractable back pain in patients with insufficient bone union following osteoporotic vertebral fracture. Eur Spine J 18:1279–1286
Ito Y, Hasegawa Y, Toda K, Nakahara S Pathogenesis and diagnosis of delayed vertebral collapse resulting from osteoporotic spinal fracture. Spine J 2:101–106
Garfin SR, Yuan HA, Reiley MA (2001) New technologies in spine: kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine (Phila Pa 1976) 26:1511–1515
Diamond TH, Champion B, Clark WA (2003) Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med 114:257–265
Klazen CA, Lohle PN, de Vries J, et al. (2010) Vertebroplasty versus conservative treatment in acute osteoporotic vertebral compression fractures (Vertos II): an open-label randomised trial. Lancet 376:1085–1092
Watts NB, Harris ST, Genant HK (2001) Treatment of painful osteoporotic vertebral fractures with percutaneous vertebroplasty or kyphoplasty. Osteoporos Int 12:429–437
Chandra RV, Yoo AJ, Hirsch JA (2013) Vertebral augmentation: update on safety, efficacy, cost effectiveness and increased survival? Pain Physician J 16:309–320
Tsujio T, Nakamura H, Terai H, et al. (2011) Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: a prospective multicenter study. Spine (Phila Pa 1976) 36:1229–1235
McKiernan F, Faciszewski T (2003) Intravertebral clefts in osteoporotic vertebral compression fractures. Arthritis Rheum 48:1414–1419
Maldague BE, Noel HM, Malghem JJ (1978) The intravertebral vacuum cleft: a sign of ischemic vertebral collapse. Radiology 129:23–29
Fang X, Yu F, Fu S, Song H (2015) Intravertebral clefts in osteoporotic compression fractures of the spine: incidence, characteristics, and therapeutic efficacy. Int J Clin Exp Med 8:16960–16968
Kanchiku T, Imajo Y, Suzuki H, et al. (2013) Usefulness of an early MRI-based classification system for predicting vertebral collapse and pseudoarthrosis after osteoporotic vertebral fractures. J Spinal Disord Tech 27:61–65
McKiernan F, Jensen R, Faciszewski T (2003) The dynamic mobility of vertebral compression fractures. J Bone Miner Res 18:24–29
Cho T, Matsuda M, Sakurai M (1996) MRI findings on healing process of vertebral fracture in osteoporosis. J Orthop Sci 1:16–33
Dupuy DE, Palmer WE, Rosenthal DI (1996) Vertebral fluid collection associated with vertebral collapse. AJR Am J Roentgenol 167:1535–1538
Baur A, Stabler A, Arbogast S, et al. (2002) Acute osteoporotic and neoplastic vertebral compression fractures: fluid sign at MR imaging. Radiology 225:730–735. doi:10.1148/radiol.2253011413
Libicher M, Appelt A, Berger I, et al. (2007) The intravertebral vacuum phenomen as specific sign of osteonecrosis in vertebral compression fractures: results from a radiological and histological study. Eur Radiol 17:2248–2252
Sarli M, Pérez Manghi FC, Gallo R, Zanchetta JR (2005) The vacuum cleft sign: an uncommon radiological sign. Osteoporos Int 16:1210–1214
Malghem J, Maldague B, Labaisse MA, et al. (1993) Intravertebral vacuum cleft: changes in content after supine positioning. Radiology 187:483–487
Meyers SP, Wiener SN (1991) Magnetic resonance imaging features of fractures using the short tau inversion recovery (STIR) sequence: correlation with radiographic findings. Skelet Radiol 20:499–507
Yao L, Lee JK (1988) Occult intraosseous fracture: detection with MR imaging. Radiology 167:749–751
Deutsch AL, Mink JH (1989) Magnetic resonance imaging of musculoskeletal injuries. Radiol Clin N Am 27:983–1002
Vogler JB, Murphy WA (1988) Bone marrow imaging. Radiology 168:679–693
Smith SR, Williams CE, Davies JM, Edwards RH (1989) Bone marrow disorders: characterization with quantitative MR imaging. Radiology 172:805–810
Kanchiku T, Taguchi T, Kawai S (2003) Magnetic resonance imaging diagnosis and new classification of the osteoporotic vertebral fracture. J Orthop 8:463–466
Zhang J, Yu KF (1998) What’s the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280:1690–1691
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Funding
This study was funded by the Japan Orthopedics and Traumatology Research Foundation, Inc. (Grant no. 270).
Ethical approval
This study was approved by the Ethics Committee of Osaka City University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all participants included in the study.
Rights and permissions
About this article
Cite this article
Takahashi, S., Hoshino, M., Takayama, K. et al. Predicting delayed union in osteoporotic vertebral fractures with consecutive magnetic resonance imaging in the acute phase: a multicenter cohort study. Osteoporos Int 27, 3567–3575 (2016). https://doi.org/10.1007/s00198-016-3687-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-016-3687-3