Abstract
Summary
The cost-effectiveness of a less intensive fracture liaison service is unknown. We evaluated a fracture liaison service that had been educating and referring patients for secondary prevention of osteoporotic fractures for 6 years. Our results suggest that a less intensive fracture liaison service, with moderate effectiveness, can still be worthwhile.
Introduction
Fragility fractures are common among older patients; the risk of re-fracture is high but could be reduced with treatments; different versions of fracture liaison service have emerged to reduce recurrent osteoporotic fractures. But the cost-effectiveness of a less intensive model is unknown. The objective of this study was to assess the cost-effectiveness of the Ontario Fracture Clinic Screening program, a fracture liaison service that had been educating and referring fragility fracture patients across Ontario, Canada to receive bone mineral density testing and osteoporosis treatments since 2007.
Methods
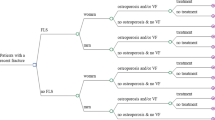
We developed a Markov model to assess the cost-effectiveness of the program over the patients’ remaining lifetime, using rates of bone mineral density testing and osteoporosis treatment and cost of intervention from the program, and supplemented it with the published literature. The analysis took the perspective of a third-party health-care payer. Costs and benefits were discounted at 5 % per year. Sensitivity analyses assessed the effects of different assumptions on the results.
Results
The program improved quality-adjusted life-years (QALYs) by 4.3 years and led to increased costs of CAD $83,000 for every 1000 patients screened, at a cost of $19,132 per QALY gained. The enhanced model, the Bone Mineral Density (BMD) Fast Track program that includes ordering bone mineral density testing, was even more cost-effective ($5720 per QALY gained).
Conclusions
The Ontario Fracture Clinic Screening program appears to be a cost-effective way to reduce recurrent osteoporotic fractures.



Similar content being viewed by others
References
Center JR, Bliuc D, Nguyen TV, Eisman JA (2007) Risk of subsequent fracture after low-trauma fracture in men and women. JAMA 297(4):387–394
Edwards BJ, Bunta AD, Simonelli C, Bolander M, Fitzpatrick LA (2007) Prior fractures are common in patients with subsequent hip fractures. Clin Orthop Relat Res 461:226–230
Freemantle N, Cooper C, Diez-Perez A, Gitlin M, Radcliffe H, Shepherd S, Roux C (2013) Results of indirect and mixed treatment comparison of fracture efficacy for osteoporosis treatments: a meta-analysis. Osteoporos Int 24(1):209–217
Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE (2004) Practice patterns in the diagnosis and treatment of osteoporosis after a fragility fracture: a systematic review. Osteoporos Int 15(10):767–778
Shibli-Rahhal A, Vaughan-Sarrazin MS, Richardson K, Cram P (2011) Testing and treatment for osteoporosis following hip fracture in an integrated U.S. healthcare delivery system. Osteoporos Int 22(12):2973–2980
Mitchell PJ (2013) Best practices in secondary fracture prevention: fracture liaison services. Curr Osteoporos Rep 11(1):52–60
Ganda K, Puech M, Chen JS, Speerin R, Bleasel J, Center JR, Eisman JA, March L, Seibel MJ (2013) Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporos Int 24(2):393–406
Marsh D, Akesson K, Beaton DE et al (2011) Coordinator-based systems for secondary prevention in fragility fracture patients. Osteoporos Int 22(7):2051–2065
Nikitovic M, Wodchis WP, Krahn MD, Cadarette SM (2013) Direct health-care costs attributed to hip fractures among seniors: a matched cohort study. Osteoporos Int 24(2):659–669
Sander B, Elliot-Gibson V, Beaton DE, Bogoch ER, Maetzel A (2008) A coordinator program in post-fracture osteoporosis management improves outcomes and saves costs. J Bone Joint Surg Am 90(6):1197–1205
Canadian Agency for Drugs and Technologies in Health (2006) Guidelines for the economic evaluation of health technologies: Canada. Ottawa
Leslie WD, LaBine L, Klassen P, Dreilich D, Caetano PA (2012) Closing the gap in postfracture care at the population level: a randomized controlled trial. CMAJ 184(3):290–296
Posen J, Beaton DE, Sale J, Bogoch ER (2013) Bone mineral density testing after fragility fracture: Informative test results likely. Can Fam Physician 59(12):e564–571
Hodsman AB, Leslie WD, Tsang JF, Gamble GD (2008) 10-year probability of recurrent fractures following wrist and other osteoporotic fractures in a large clinical cohort: an analysis from the Manitoba Bone Density Program. Arch Intern Med 168(20):2261–2267
MacLean C, Newberry S, Maglione M et al (2008) Systematic review: comparative effectiveness of treatments to prevent fractures in men and women with low bone density or osteoporosis. Ann Intern Med 148(3):197–213
McLellan AR, Gallacher SJ, Fraser M, McQuillian C (2003) The fracture liaison service: success of a program for the evaluation and management of patients with osteoporotic fracture. Osteoporos Int 14(12):1028–1034
Majumdar SR, Johnson JA, Lier DA et al (2007) Persistence, reproducibility, and cost-effectiveness of an intervention to improve the quality of osteoporosis care after a fracture of the wrist: results of a controlled trial. Osteoporos Int 18(3):261–270
Burden AM, Paterson JM, Solomon DH, Mamdani M, Juurlink DN, Cadarette SM (2012) Bisphosphonate prescribing, persistence and cumulative exposure in Ontario, Canada. Osteoporos Int 23(3):1075–1082
Majumdar SR, Lier DA, Leslie WD (2013) Cost-effectiveness of two inexpensive postfracture osteoporosis interventions: results of a randomized trial. J Clin Endocrinol Metab 98(5):1991–2000
Black DM, Schwartz AV, Ensrud KE et al (2006) Effects of continuing or stopping alendronate after 5 years of treatment: the Fracture Intervention Trial Long-term Extension (FLEX): a randomized trial. JAMA 296(24):2927–2938
McLellan AR, Wolowacz SE, Zimovetz EA, Beard SM, Lock S, McCrink L, Adekunle F, Roberts D (2011) Fracture liaison services for the evaluation and management of patients with osteoporotic fracture: a cost-effectiveness evaluation based on data collected over 8 years of service provision. Osteoporos Int 22(7):2083–2098
Haentjens P, Magaziner J, Colon-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, Boonen S (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380–390
Statistics Canada Life Tables, Canada, provinces and territories 2000–2002
Chau D, Becker DL, Coombes ME, Ioannidis G, Adachi JD, Goeree R (2012) Cost-effectiveness of denosumab in the treatment of postmenopausal osteoporosis in Canada. J Med Econ 15(s1):3–14
Leslie WD, Lix LM, Finlayson GS, Metge CJ, Morin SN, Majumdar SR (2013) Direct healthcare costs for 5 years post-fracture in Canada: a long-term population-based assessment. Osteoporos Int 24(5):1697–1705
Statistics Canada Consumer Price Index. http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/econ09a-eng.htm 2014
Orpana HM, Ross N, Feeny D, McFarland B, Bernier J, Kaplan M (2009) The natural history of health-related quality of life: a 10 year cohort study. Statistics Canada, Ottawa, Ontario
Laupacis A, Feeny D, Detsky AS, Tugwell PX (1993) Tentative guidelines for using clinical and economic evaluations revisited. CMAJ 148(6):927–929
Cooper MS, Palmer AJ, Seibel MJ (2012) Cost-effectiveness of the Concord Minimal Trauma Fracture Liaison service, a prospective, controlled fracture prevention study. Osteoporos Int 23(1):97–107
Si L, Winzenberg T, Palmer A (2014) A systematic review of models used in cost-effectiveness analyses of preventing osteoporotic fractures. Osteoporos Int 25(1):51–60
Majumdar SR, Lier DA, Rowe BH, Russell AS, McAlister FA, Maksymowych WP, Hanley DA, Morrish DW, Johnson JA (2011) Cost-effectiveness of a multifaceted intervention to improve quality of osteoporosis care after wrist fracture. Osteoporos Int 22(6):1799–1808
Sato Y, Iwamoto J, Kanoko T, Satoh K (2005) Risedronate sodium therapy for prevention of hip fracture in men 65 years or older after stroke. Arch Intern Med 165(15):1743–1748
Majumdar SR, Beaupre LA, Harley CH, Hanley DA, Lier DA, Juby AG, Maksymowych WP, Cinats JG, Bell NR, Morrish DW (2007) Use of a case manager to improve osteoporosis treatment after hip fracture: results of a randomized controlled trial. Arch Intern Med 167(19):2110–2115
Ontario Ministry of Health and Long-Term Care Ontario Health Insurance (OHIP) Schedule of Benefits and Fees. http://www.health.gov.on.ca/english/providers/program/ohip/sob/sob_mn.html
Ontario Ministry of Health and Long-Term Care Ontario Drug Benefit Formulary/ Comparative Drug Index. https://www.healthinfo.moh.gov.on.ca/formulary/index.jsp
Peasgood T, Herrmann K, Kanis JA, Brazier JE (2009) An updated systematic review of Health State Utility Values for osteoporosis related conditions. Osteoporos Int 20(6):853–868
Jaglal SB, Donescu OS, Bansod V et al (2012) Impact of a centralized osteoporosis coordinator on post-fracture osteoporosis management: a cluster randomized trial. Osteoporos Int 23(1):87–95
Acknowledgments
This project was funded by the Ontario Ministry of Health and Long-Term Care as part of the Ontario Osteoporosis Strategy. The views expressed are those of the researchers and do not necessarily reflect those of the Ministry. The authors would like to acknowledge Mr. Ravi Jain, Director of the Ontario Osteoporosis Strategy, for his help in estimating the cost of program; Dr. Earl Bogoch for his leadership in evaluating the clinical effectiveness of the FCS program; Dr. Beate Sander and Victoria Elliott Gibson for providing helpful advice; and the FCS program evaluation team for their feedback.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 50 kb)
Rights and permissions
About this article
Cite this article
Yong, J.H.E., Masucci, L., Hoch, J.S. et al. Cost-effectiveness of a fracture liaison service—a real-world evaluation after 6 years of service provision. Osteoporos Int 27, 231–240 (2016). https://doi.org/10.1007/s00198-015-3280-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3280-1