Abstract
Objectives
To analyse the clinical value of procalcitonin (PCT), C-reactive protein (CRP) and leucocyte count in the diagnosis of paediatric sepsis and in the stratification of patients according to severity.
Design
Prospective, observational study.
Setting
Paediatric intensive care unit (PICU).
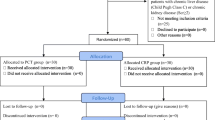
Patients
Ninety-four children.
Measurement and results
Leucocyte count, PCT and CRP were measured when considered necessary during the PICU stay. Patients were classified, when PCT and CRP were measured, into one of six categories (negative, SIRS, localized infection, sepsis, severe sepsis, and septic shock) according to the definitions of the American College of Chest Physicians /Society of Critical Care Medicine. A total of 359 patient day episodes were obtained. Leucocyte count did not differ across the six diagnostic classes considered. Median plasma PCT concentrations were 0.17, 0.43, 0.79, 1.80, 15.40 and 19.13 ng/ml in negative, systemic inflammatory response syndrome (SIRS), localized infection, sepsis, severe sepsis, and septic shock groups, respectively, whereas median plasma CRP concentrations were 1.35, 3.80, 6.45, 5.70, 7.60 and 16.2 mg/dl, respectively. The area under the ROC curve for the diagnosis of septic patients was 0.532 for leucocyte count (95% CI, 0.462–0.602), 0.750 for CRP (95% CI, 0.699–0.802) and 0.912 for PCT (95% CI, 0.882–0.943). We obtained four groups using CRP values and five groups using PCT values that classified a significant percentage of patients according to the severity of the different SIRS groups.
Conclusions
PCT is a better diagnostic marker of sepsis in critically ill children than CRP. The CRP, and especially PCT, may become a helpful clinical tool to stratify patients with SIRS according to disease severity.




Similar content being viewed by others
References
Brun-Buisson C (2000) The epidemiology of the systemic inflammatory response. Intensive Care Med 26: (Suppl. 1) S64–S74
Parrillo JE (1993) Pathogenetic mechanisms of septic shock. N Engl J Med 328:1471–1477
Hayden WR (1994) Sepsis terminology in pediatrics. J Pediatr 124:657–658
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Intensive Care Med 29:530–538
Hatherill M, Tibby SM, Sykes K, Turner C, Murdoch IA (1999) Diagnostic markers of infection: comparison of procalcitonin with C reactive protein and leucocyte count. Arch Dis Child 81:417–421
American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (1992) Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Carcillo JA (2003) Pediatric septic shock and multiple organ failure. Crit Care Clin 19:413–440
Hanley JA, McNeil BA (1982) The meaning and use of the area under a receiver operating (ROC) curve. Radiology 143:29–36
Goh A, Lum L (1999) Sepsis, severe sepsis and septic shock in paediatric multiple organ dysfunction syndrome. J Paediatr Child Health 35:488–492
Castelli GP, Pognani C, Cita M, Stuani A, Sgarbi L, Paladini R (2006) Procalcitonin, C-reactive protein, white blood cells and SOFA score in ICU: diagnosis and monitoring of sepsis. Minerva Anestesiol 72:69–80
Carrol ED, Newland P, Riordan FA, Thomson AP, Curtis N, Hart CA (2002) Procalcitonin as a diagnostic marker of meningococcal disease in children presenting with fever and a rash. Arch Dis Child 86:282–285
Enguix A, Rey C, Concha A, Medina A, Coto D, Dieguez MA (2001) Comparison of procalcitonin with C-reactive protein and serum amyloid for the early diagnosis of bacterial sepsis in critically ill neonates and children. Intensive Care Med 27:211–215
Muller B, Becker KL, Schachinger H, Rickenbacher PR, Huber PR, Zimmerli W, Ritz R (2000) Calcitonin precursors are reliable markers of sepsis in a medical intensive care unit. Crit Care Med 28:977–983
Povoa P, Almeida E, Moreira P, Fernandes A, Mealha R, Aragao A, Sabino H (1998) C-reactive protein as an indicator of sepsis. Intensive Care Med 24:1052–1056
Suprin E, Camus C, Gacouin A, Le Tulzo Y, Lavoue S, Feuillu A, Thomas R (2000) Procalcitonin: A valuable indicator of infection in a medical ICU? Intensive Care Med 26:1232–1238
Ugarte H, Silva E, Mercan D, Mendonca A de, Vincent JL (1999) Procalcitonin used as a marker of infection in the intensive care unit. Crit Care Med 27:498–504
Luzzani A, Polati E, Dorizzi R, Rungatscher A, Pavan R, Merlini A (2003) Comparison of procalcitonin and C-reactive protein as markers of sepsis. Crit Care Med 31:1737–1741
Geppert A, Steiner A, Delle-Karth G, Heinz G, Huber K (2003) Usefulness of procalcitonin for diagnosing complicating sepsis in patients with cardiogenic shock. Intensive Care Med 29:1384–1389
Arkader R, Troster EJ, Lopes MR, Junior RR, Carcillo JA, Leone C, Okay TS (2006) Procalcitonin does discriminate between sepsis and systemic inflammatory response syndrome. Arch Dis Child 91:117–120
Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY (2006) Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med 34:1996–2003
Hatherill M, Tibby SM, Turner C, Ratnavel N, Murdoch IA (2000) Procalcitonin and cytokine levels: relationship to organ failure and mortality in pediatric septic shock. Crit Care Med 28:2591–2594
Castelli GP, Pognani C, Meisner M, Stuani A, Bellomi D, Sgarbi L (2004) Procalcitonin and C-reactive protein during systemic inflammatory response syndrome, sepsis and organ dysfunction. Crit Care 8:R234-R242
Clec'h C, Fosse JP, Karoubi P, Vincent F, Chouahi I, Hamza L, Cupa M, Cohen Y (2006) Differential diagnostic value of procalcitonin in surgical and medical patients with septic shock. Crit Care Med 34:102–107
Celebi S, Koner O, Menda F, Balci H, Hatemi A, Korkut K, Esen F (2006) Procalcitonin kinetics in pediatric patients with systemic inflammatory response after open heart surgery. Intensive Care Med 32:881–887
Meisner M, Tschaikowsky K, Palmaers T, Schmidt J (1999) Comparison of procalcitonin (PCT) and C-reactive protein (CRP) plasma concentrations at different SOFA scores during the course of sepsis and MODS. Crit Care (Lond) 3:45–50
Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, Vadas L, Pugin J (2001) Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med 164:396–402
Casado-Flores J, Blanco-Quiros A, Asensio J, Arranz E, Garrote JA, Nieto M (2003) Serum procalcitonin in children with suspected sepsis: a comparison with C-reactive protein and neutrophil count. Pediatr Crit Care Med 4:190–195
Mimoz O, Benoist JF, Edouard AR, Assicot M, Bohuon C, Samii K (1998) Procalcitonin and C-reactive protein during the early posttraumatic systemic inflammatory response syndrome. Intensive Care Med 24:185–188
Carcillo JA (2004) Mannose-binding lectin deficiency provides a genetic basis for the use of SIRS/sepsis definitions in critically ill patients. Intensive Care Med 30:1263–1265
Trzeciak S, Zanotti-Cavazzoni S, Parrillo JE, Dellinger RP (2005) Inclusion criteria for clinical trials in sepsis: Did the American College of Chest Physicians/Society of Critical Care Medicine consensus conference definitions of sepsis have an impact? Chest 127:242–245
Acknowledgements
The authors gratefully acknowledge the assistance of the medical and nursing staff of the PICU of Hospital Universitario Central de Asturias.
Author information
Authors and Affiliations
Corresponding author
Additional information
An erratum to this article can be found at http://dx.doi.org/10.1007/s00134-007-0650-y
Rights and permissions
About this article
Cite this article
Rey, C., Los Arcos, M., Concha, A. et al. Procalcitonin and C-reactive protein as markers of systemic inflammatory response syndrome severity in critically ill children. Intensive Care Med 33, 477–484 (2007). https://doi.org/10.1007/s00134-006-0509-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-006-0509-7