Abstract
Purpose
To compare the analgesic efficacy of unilateral subcostal transversus abdominis plane (TAP) block with local anesthetic infiltration, applied to the port site in patients undergoing laparoscopic cholecystectomy (LC).
Methods
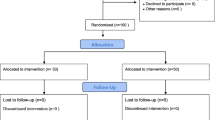
Group T received a unilateral subcostal TAP block, group I received a local anesthetic infiltration at port sites, and group C was the control group. Groups T and I received 20 mL 0.25% bupivacaine. Intravenous patient-controlled analgesia with tramadol was similarly applied to all groups. Postoperative pain levels during rest and cough were evaluated using a numeric rating scale (NRS). Nausea and vomiting were evaluated using postoperative nausea vomiting scores (PONV) at 1, 3, 6, 12 and 24 h and tramadol consumption was also determined. Patient satisfaction was evaluated using a Likert-type scale.
Results
Postoperative resting NRS scores were lower in group T than the other groups at 1 h and 12 h (p = 0.007 and p = 0.016), while NRS values during cough were statistically significant at 1 h (p = 0.004). The 24‑h tramadol consumption was different: group T 229 ± 33 mg, group I 335 ± 95 mg, and group C 358 ± 66 mg (p < 0.001). The percentages of patients reporting that they would prefer the applied postoperative pain control method again were 83.3%, 62.5% and 70.8% in groups T, I and C, respectively (p = 0.118).
Conclusion
Unilateral subcostal TAP block was superior to local anesthetic infiltration at port sites after LC, in terms of low opioid consumption. Unilateral subcostal TAP block is recommended as part of a multimodal analgesic protocol.
Zusammenfassung
Ziel
Die analgetische Wirksamkeit der unilateralen subkostalen Transversus-abdominis-plane(TAP)-Blockade wurde mit der lokalen Port-site-Infiltrationsanästhesie bei laparoskopisch behandelten Patienten verglichen.
Methoden
Gruppe T erhielt eine einseitige subkostale TAP-Blockade, Gruppe I erhielt eine lokale Port-site-Infiltrationsanästhesie. Gruppe C war die Kontrollgruppe. Gruppe T und I erhielt 20 ml Bupivacain 0,25 %. Eine intravenöse patientengesteuerte Analgesie mit Tramadol wurde bei allen Gruppen angewendet. Das postoperative Schmerzniveau während Ruhe und Husten wurde mit dem numerischen Schmerzskala (NRS) bewertet: Übelkeit und Erbrechen wurden mit dem Postoperative Nausea and Vomiting Score (PONV) nach 1, 3, 6, 12 und 24 h bewertet und der kumulative Tramadolverbrauch wurde bestimmt. Die Patientenzufriedenheit wurde anhand der Likert-Skala bewertet.
Ergebnis
Die postoperativen NRS-Werte im Ruhezustand waren in Gruppe T nach der 1. und 12. Stunde niedriger als in den anderen Gruppen (p = 0,007, p = 0,016). Der NRS-Wert während des Hustens war nach der 1. Stunde statistisch signifikant (p = 0,004). Der 24-Stunden-Tramadolverbrauch der Gruppen war unterschiedlich, Gruppe T: 229 + 33 mg; Gruppe I: 335 + 95 mg und Gruppe C: 358 + 66 mg (p < 0,001). Der prozentuale Anteil der Patienten, die angaben, dass sie die angewandte postoperative Schmerzkontrollmethode wieder bevorzugen würden, betrug 83,3 %, 62,5 % und 70,8 % in den Gruppen T, I und C (p = 0,118).
Schlussfolgerung
Die unilaterale subkostale TAP-Blockade war der lokalen Port-site-Infiltrationsanästhesie an den Portstellen nach laparoskopischer Cholezystektomie in Bezug auf einen geringen Opioidverbrauch überlegen. Die Verwendung einer unilateralen subkostalen TAP-Blockade als Teil multimodaler Analgetikaprotokolle ist zu empfehlen.



Similar content being viewed by others
References
Boer HD, Detriche O, Forget P (2017) Opioid-related side effects: postoperative ileus, urinary retention, nausea and vomiting, and shivering. A review of the literature. Best Pract Res Clin Anaesthesiol 31(4):499–504
Soliz JM, Lipski I, Hancher-Hodges S, Bryce Speer B, Popat K (2017) Subcostal transverse abdominis plane block for acute pain management: a review. Anesth Pain Med 7(5):e12923
Ma N, Duncan JK, Scarfe AJ, Schuhmann S, Cameron AL (2017) Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia: a systematic review and meta-analysis. J Anesth 31(3):432–452
Deepanshu M, Sandeep S, Sumi S et al (2019) Anesthetic techniques: focus on transversus abdominis plane (TAP) blocks. Local Reg Anesth 12:81–88
Toju K, Shiraishi K, Hakozaki T, Isosu T, Murakawa M (2015) Plasma ropivacaine concentrationfollowing ultrasound-guided subcostal transversus abdominis plane block in adults. J Anesth 29(1):146–148
El-Boghdadly K, Pawa A, Chin KJ (2018) Local anesthetic systemic toxicity: current perspectives. Local Reg Anesth 11:35–44
Lancaster P, Chadwick M (2010) Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth 104(4):509–510
Soltani Mohammadi S, Dabir A, Shoeibi G (2014) Efficacy of transversus abdominis plane block for acute postoperative pain relief in kidney recipients: a double-blinded clinical trial. Pain Med 15(3):460–464
Børglum J, Gögenür I, Bendtsen TF (2016) Abdominal wall blocks in adults. Curr Opin Anaesthesiol 29(5):638–643
Tanggaard K, Jensen K, Lenz K et al (2015) A randomised controlled trial of bilateral dual transversus abdominis plane blockade for laparoscopic appendicectomy. Anaesthesia 70:1395–1400
Saliminia A, Azimaraghi O, Babayipour S, Ardavan K, Movafeqh A (2015) Efficacy of transverse abdominis plane block in reduction of postoperationpain in laparoscopic cholecystectomy. Acta Anaesthesiol Taiwan 53:119–122
Torup H, Bøgeskov M, Hansen EG et al (2015) Transversus abdominis plane (TAP) block after robot-assisted laparoscopic hysterectomy: a randomised clinical trial. Acta Anaesthesiol Scand 59:928–935
Oh TK, Yim J, Kim J et al (2017) Effects of preoperative ultrasound-guided transversus abdominis plane block on pain after laparoscopic surgery for colorectal cancer. Surg Endosc 31(1):127–134
Hebbard P (2015) TAP block nomenclature. Anaesthesia 70(1):112–113
Tsai HC, Yoshida T, Chuang TY, Yang SF, Chang CC, Yao HY, Tai YT, Lin JA, Chen KY (2017) Transversus abdominis plane block: an updated review of anatomy and techniques. Biomed Res Int. https://doi.org/10.1155/2017/8284363
Oksar M, Koyuncu O, Turhanoglu S, Temiz M, Oran MC (2016) Transversus abdominis plane block as a component of multimodal analgesia for laparoscopic cholecystectomy. J Clin Anesth 34:72–78
Shin HJ, Oh AY, Baik JS, Kim JH, Han SH, Hwang JW (2014) Ultrasound-guided oblique subcostal transversus abdominis plane block for analgesia after laparoscopic cholecystectomy. Minerva Anestesiol 80:185–193
Suseela I, Anandan K, Aravind A, Kaniyil S (2018) Comparison of ultrasound-guided bilateral subcostal transversus abdominis plane block and port-site infiltration with bupivacaine in laparoscopic cholecystectomy. Indian J Anaesth 62(7):497–501
Vrsajkov V, Mančić N, Mihajlović D, Milićević ST, Uvelin A, Vrsajkov JP (2018) Subcostal transversus abdominis plane block can improve analgesia after laparoscopic cholecystectomy. Rev Bras Anestesiol 68(2):149–153
Ma J, Jiang Y, Tang S, Wang B, Lian Q, Xie Z, Li J (2017) Analgesic efficacy of ultrasound-guided subcostal transversus abdominis plane block. Medicine (Baltimore) 96(10):e6309
Støving K, Rothe C, Rosenstock CV, Aasvang EK, Lundstrøm LH, Lange KH (2015) Cutaneous sensory block area, muscle-relaxingeffect, and block duration of the transversus abdominis plane block: a randomized, blinded, and placebo controlled study in healthy volunteers. Reg Anesth Pain Med 40(4):355–362
Tolchard S, Davies R, Martindale S (2012) Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol 28(3):339–343
Ahn SR, Kang DB, Lee C, Park WC, Lee JK (2013) Postoperative pain relief using wound infiltration with 0.5% bupivacaine in single-incision laparoscopic surgery for an appendectomy. Ann Coloproctol 29(6):238–242
Bisgaard T (2006) Analgesic treatment after laparoscopic cholecystectomy: a critical assessment of the evidence. Anesthesiology 104:835–846
Moiniche S, Jorgensen H, Wetterslev J, Dahl JB (2000) Local anesthetic infiltration for postoperative pain relief after laparoscopy: a qualitative and quantitative systematic review of intraperitoneal, port-site infiltration and mesosalpinx block. Anesth Analg 90(4):899–812
Ayman M, Materazzi G, Bericotti M, Rago R, Nidal Y, Miccoli P (2012) Bupivacaine 0.5 % versus ropivacaine 0.75 % wound infiltration to decrease postoperative pain in total thyroidectomy. Minerva Chir 67:511–516
Yu N, Long X, Lujan-Hernandez JR, Succar J, Xin X, Wang X (2014) Transversus abdominis-plane block versus local anesthetic wound infiltration in lower abdominal surgery. BMC Anesthesiol 14:121
Abdallah FW, Laffey JG, Halpern SH, Brull R (2013) Duration of analgesic effectiveness after the posterior and lateral transversus abdominis plane block techniques for transverse lower abdominal incisions: a meta-analysis. Br J Anaesth 111(5):721–735
Chang H, Rimel BJ, Li AJ, Cass I, Karlan BY, Walsh C (2018) Ultrasound guided transversus abdominis plane (TAP) block utilization in multimodal pain management after open gynecologic surgery. Gynecol Oncol Rep 26:75–77
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
E. Arik, T. Akkaya, S. Ozciftci, A. Alptekin and Ş. Balas declare no financial or other conflicts of interest.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Arık, E., Akkaya, T., Ozciftci, S. et al. Unilateral transversus abdominis plane block and port-site infiltration. Anaesthesist 69, 270–276 (2020). https://doi.org/10.1007/s00101-020-00746-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-020-00746-1
Keywords
- Laparoscopic cholecystectomy
- Unilateral transversus abdominis plane block
- Port-site infiltration
- Post-operative analgesia
- Opioid consumption