Abstract
Background: Women with abnormal screening mammograms require diagnostic assessment and experience anxiety until a diagnosis is established. This report evaluated the timeliness of diagnosis after an abnormal screening mammogram in the Screening Mammography Program of British Columbia (SMPBC).
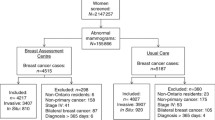
Methods: Information on diagnostic interventions following an abnormal screen (N = 10,314) provided through 11 regional SMPBC services between January 1, 1993 and June 30, 1994 were abstracted and analyzed.
Results: The median time from abnormal screen to diagnosis was 3.4 weeks with regional variation of 2.0 to 4.7 weeks; 10% waited 8.7 weeks or longer. For the 19% of women proceeding to open biopsy, the median diagnostic interval was 7.1 weeks with regional variation of 4.6 to 9.3 weeks; 10% waited 13.1 weeks or longer.
Interpretation: After an abnormal screening mammogram, women waited many weeks for a definitive diagnosis, especially those proceeding to open biopsy. Opportunities for process improvement were identified.
Résumé
Contexte: Les femmes qui ont une mammographie anormale et qui nécessitent une évaluation diagnostique, vivent dans l’anxiété jusqu’à la confirmation du diagnostic. Ce rapport a cherché à évaluer les délais d’attente du diagnostic après une mammographie anormale dans le cadre du programme de dépistage par mammographie de la Colombie-Britannique (Screening Mammography Program of British Columbia ou SMPBC).
Méthodologie: Les données relatives aux interventions diagnostiques suite à une mammographie anormale (N = 10 314) provenant de 11 services régionaux faisant partie du Programme, et couvrant la période du 1er janvier 1993 au 30 juin 1994, ont été analysées.
Résultats: L’intervalle moyen entre la mammographie et la pose du diagnostic était de 3,4 semaines, avec des variations régionales de 2 à 4,7 semaines; 10 % des femmes ont dû attendre 8,7 semaines ou plus. Pour les 19 % sur lesquelles on a procédé à une biopsie, l’intervalle de temps avant le diagnostic était de 7,1 semaines, avec des variations régionales de 4,6 à 9,3 semaines; 10 % des femmes ont dû attendre 13,1 semaines ou plus.
Interprétation: Après une mammographie anormale, les femmes ont dû attendre de nombreuses semaines avant d’avoir un diagnostic définitif, notamment dans le cas de celles ayant eu une biopsie. Nous avons identifié un certain nombre de secteurs qui permettraient d’améliorer la procédure.
Similar content being viewed by others
References
Fletcher SW, Black W, Harris R, et al. Report of the International Workshop on Screening for Breast Cancer. J Natl Cancer Inst 1993;85:1644–56.
Nystrom L, Rutqvist LE, Wall S, et al. Breast cancer screening with mammography: Overview of Swedish randomized trials. Lancet 1993;341:973–78 [published erratum appears in Lancet 1993;342:1372].
Kerlikowske K, Grady D, Rubin SM, et al. Efficacy of screening mammography. A metaanalysis. JAMA 1995;273:149–54.
Fentiman I. Pensive women, painful vigils: Consequences of delay in assessment of mammographic abnormalities. Lancet 1988;1:1041–42.
Gram IT, Lund E, Slenker, SE. Quality of life following a false positive mammogram. Br J Cancer 1990;62:1018–22.
Ong G, Austokar J. Breast screening: Adverse psychological consequences one month after placing women on early recall because of a diagnostic uncertainty: A multicentre study. J Med Screen 1997;4:158–68.
Lerman C, Trock B, Rimer BK, et al. Psychological and behavioral implications of abnormal mammograms. Ann Intern Med 1991;114:657–61.
Hislop TG, Worth AJ, Kan L, et al. Post screendetected breast cancer within the Screening Mammography Program of British Columbia. Breast Cancer Res Treat 1997;42:235–42.
Murray-Sykes K. Organizing Assessment. National Health Service Breast Screening Programme. Breast Screen Publications, 1989.
Commonwealth Department of Human Services and Health (CDHSH). National Program for the Early Detection of Breast Cancer: National accreditation requirements. Australia: CDHSH, 1994.
Libstug A, Moravan V, Aitken, SE. Results from the Ontario Breast Screening Program, 1990–1995. J Med Screen 1998;5:73–80.
Caines J, Chantziantoniou K, Wright BA, et al. Nova Scotia breast screening program experience: Use of needle-core biopsy in the diagnosis of screening-detected abnormalities. Radiology 1996;198:125–30.
The Workshop Group. Reducing Deaths from Breast Cancer in Canada — Workshop report. CMAJ 1989;141:199–201.
Kerlikowske K. Timeliness of follow-up after abnormal screening mammography. Breast Cancer Res Treat 1996;40:53–64.
Chang SW, Kerlikowske K, Napoles-Springer A, et al. Racial differences in timeliness of follow-up after abnormal screening mammography. Cancer 1996;78:1395–402.
Baum M. Delayed assessment of mammographic abnormalities. Lancet 1988;1:1218.
Burman ML, Taplin SH, Herta DF, et al. Effect of false-positive mammograms on interval breast cancer screening in a health maintenance organization. Ann Intern Med 1999;131:1–6.
National Institutes of Health Consensus Development Panel. National Institutes of Health consensus development conference statement: Breast cancer screening for women ages 40–49, January 21–23, 1997. J Natl Cancer Inst 1997;89:1015–26.
Kerlikowske K. Efficacy of screening mammography among women aged 40–49 years and 50–69 years: Comparison of relative and absolute benefit. Monogr Natl Cancer Inst 1997;22:79–86.
Hendrick RE, Smith RA, Rutledge III JH, et al. Benefit of screening mammography in women aged 40–49: A new meta-analysis of randomized controlled trials. Monogr Natl Cancer Inst 1997;22:87–92.
Bear, HD. Image-guided breast biopsy. How, when, and by whom? J Surg Oncol 1998;67:1–5.
Britton PD, Flower CDR, Freeman AH, et al. Change to core biopsy in an NHS breast screening unit. Clin Radiol 1997;52:764–67.
Litherland JC, Evans AJ, Wilson ARM, et al. The impact of core biopsy on pre-operative diagnosis rate of screen detected breast cancers. Clin Radiol 1996;51:562–65.
Coates, AS. Breast cancer: Delays, dilemmas and delusions. Lancet 1999;353L:1112–13.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Olivotto, I.A., Kan, L., King, S. et al. Waiting for a Diagnosis After an Abnormal Screening Mammogram. Can J Public Health 91, 113–117 (2000). https://doi.org/10.1007/BF03404922
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03404922