Abstract
OBJECTIVE: Treatment of elevated cholesterol levels reduces morbidity and mortality from coronary heart disease in high-risk patients, but can be costly. The purpose of this study was to determine whether physician extenders emphasizing diet modification and, when necessary, effective and inexpensive drug algorithms can provide more cost-effective therapy than conventional care.
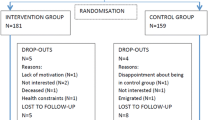
DESIGN: Randomized controlled trial.
SETTING: A Department of Veterans Affairs Medical Center.
PATIENTS: Two hundred forty-seven veterans with type IIa hypercholesterolemia.
INTERVENTIONS: Patients assigned to either a cholesterol treatment program (CTP) or usual health care provided by general internists (UHC). CTP included intensive dietary therapy administered by a registered dietitian utilizing individual and group counseling and drug therapy initiated by physician extenders for those failing to achieve goal low-density lipo-protein (LDL) levels with diet alone. A drug selection algorithm for CTP subjects utilized niacin as initial therapy followed by bile acid sequestrants and lovastatin. Subjects were followed prospectively for 2 years.
MEASUREMENTS: Primary outcome measurements were effectiveness of therapy defined as reductions in LDL cholesterol (LDL-C), and whether goal LDL-C levels were achieved; costs of therapy; and cost-effectiveness defined as the cost per unit reduction in the LDL-C.
MAIN RESULTS: Total program costs were higher for CTP patients than for UHC patients ($659±$43 vs $477±$42 per patient, p<.001). However, at 24 months the patients in CTP were more likely to achieve LDL goal levels (65% vs 44%,p<.005), and also achieved greater reductions in LDL-C 27%±2% vs 14%±2% at 24 months,p<.001). Program costs per unit (mmol/L) reduction in the LDL-C, a measure of cost-effectiveness, was significantly lower for CTP ($758±$58 vs $1,058±$70,p=.002).
CONCLUSIONS: Although more expensive than usual care, the greater effectiveness of physician extenders implementing cholesterol treatment algorithms resulted in more cost-effective therapy.
Similar content being viewed by others
References
The Scandinavian Simvastatin Survival Group. Randomized trial of cholesterol lowering in 4444 patients with coronary heart disease: The Scandinavian Simvastatin Survival Study (4S). Lancet. 1994;344:1383–9.
Jukema J, Bruschke A, Boven AV, et al. Effects of lipid lowering by pravastatin on progression and regression of coronary artery disease in symptomatic men with normal to moderately elevated serum cholesterol levels. The Regression Growth Evaluation Statin Study (REGRESS). Circulation. 1995;91:2528–40.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol Levels. Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II). JAMA. 1993;269:3015–21.
Sempos C, et al. Prevalence of high blood cholesterol among US adults: an update based on guidelines from the second report of the National Cholesterol Education Program Adult Treatment Panel. JAMA. 1993;269:3009–14.
Goldman L, Gordon D, Rifkind B, et al. Cost and health implications of cholesterol lowering. Circulation. 1992;85:1960–8.
Cohen MV, Byrne MJ, Levine B, Gutowski T, Adelson R. Low rate of treatment of hypercholesterolemia by cardiologists in patients with suspected and proven coronary artery disease. Circulation. 1991;83:1294–304.
Superko HR, Desmond DA, de SV, Vranizan KM, Farquhar JW. Blood cholesterol treatment attitudes of community physicians: a major problem. Am Heart J. 1988;116:849–55.
Schectman J, Elinsky E, Bartman B. Primary care clinician compliance with cholesterol treatment guidelines. J Gen Intern Med. 1991;6:121–5.
Hyman D, Maibach E, Flora J, Fortmann S. Cholesterol treatment practices of primary care physicians. Public Health Rep. 1992;107:441–8.
Blair T, Bryant F, Bocuzzi S. Treatment of hypercholesterolemia by a clinical nurse using a stepped-care protocol in a nonvolunteer population. Arch Intern Med. 1988;148:1046–8.
Debusk R, Miller N, Superko H, et al. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–9.
Shaffer J, Wexler L. Reducing low-density lipoprotein cholesterol levels in an ambulatory care system. Arch Intern Med. 1995;155:2330–5.
Schectman G, Hiatt J, Hartz A. Telephone contacts do not improve compliance to niacin or bile acid sequestrants. Ann Pharmacother. 1994;28:29–34.
The Expert Panel. Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Arch Intern Med. 1988;148:36–69.
Kinosian B, Glick H, Garland G. Cholesterol and coronary heart disease: predicting risks by levels and ratios. Ann Intern Med. 1994;121:641–7.
Assmann G, Schulte H, Funke H, Eckardstein A, Seedorf U. The prospective cardiovascular Munster (PROCAM) study: identification of high-risk individuals for myocardial infarction and the role of high-density lipoprotein. In: Miller N, ed. High Density Lipoproteins and Atherosclerosis II. Amsterdam: Excerpta Medica;1989; ICS 826:51–6.
Allain C, Poon L, Chan C, Richmond W, Fu P. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–5.
Megraw R. Dunn D, Biggs H. Manual and continuous-flow colorimetry of triacylglycerols by a fully enzymic method. Clin Chem. 1979;25:273–8.
Assmann G, Schriewer H, Schmitz G, Hagele E. Quantification of high-density-lipoprotein cholesterol by precipitation with phosphotungstic acid/MgC12. Clin Chem. 1983;29:2026–30.
Friedewald W, Levy R, Fredrickson D. Estimation of the concentration of low density lipoprotein cholesterol in plasma, without the use of the preparative centrifuge. Clin Chem. 1972;18:499–502.
Rothman K. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1:43–6.
Giles W, Anda R, Jones D, Serdula M, Merritt R, DeStefano F. Recent trends in the identification and treatment of high blood cholesterol by physicians. Progress and missed opportunities. JAMA. 1993;269:1133–8.
Fix KN, Oberman A. Barriers to following National Cholesterol Educational Program guidelines. An appraisal of poor physician compliance [editorial; comment]. Arch Intern Med. 1992;152:2385–7.
Maiman L, Greenland P. Patterns of physicians’ treatments for referral patients from public cholesterol screening. Am J Prev Med. 1991;7:273–9.
Hunninghake D, Stein E, Dujovne C, et al. The efficacy of intensive dietary therapy alone or combined with lovastatin in outpatients with hypercholesterolemia. N Engl J Med. 1993;328:1213–9.
Henkin Y, Garber D, Osterlund L, Darnell B. Saturated fats, cholesterol, and dietary compliance. Arch Intern Med. 1992;152:1167–74.
Illingworth D, Stein W, Mitchel Y, et al. Comparative effects of lovastatin and niacin in primary hypercholesterolemia: a prospective trial. Arch Intern Med. 1994;154:1586–95.
Schectman G, Hiatt J, Hartz A. Evaluation of the effectiveness of lipid-lowering therapy (bile acid sequestrants, niacin, psyllium and lovastatin) for treating hypercholesterolemia in veterans. Am J Cardiol. 1993;71:759–65.
Andrade S, Walker A, Gottlieb L, et al. Discontinuation of antihy-perlipidemic drugs. Do rates reported in clinical trials reflect rates in primary care settings? N Engl J Med. 1995;332:1125–31.
Heudebert G, Ruiswyk JV, Hiatt J, Schectman G. Combination drug therapy for hypercholesterolemia: the trade-off between cost and simplicity. Arch Intern Med. 1993;153:1828–37.
The Lipid Research Clinics Program. The Lipid Research Clinics Primary Prevention Trial results, I: reduction in the incidence of coronary heart disease. JAMA. 1984;251:351–64.
Shear C. Franklin F, Stinnett S, et al. Expanded Clinical Evaluation of Lovastatin (EXCEL) study results. Effect of patient characteristics on lovastatin-induced changes in plasma concentrations of lipids and lipoproteins. Circulation. 1992;85:1293–303.
Author information
Authors and Affiliations
Additional information
Supported by Health Services Research and Delivery grant 88-127, Department of Veterans Affairs.
Rights and permissions
About this article
Cite this article
Schectman, G., Wolff, N., Byrd, J.C. et al. Physician extenders for cost-effective management of hypercholesterolemia. J Gen Intern Med 11, 277–286 (1996). https://doi.org/10.1007/BF02598268
Issue Date:
DOI: https://doi.org/10.1007/BF02598268