Abstract
Purpose
The epidemiology of infections caused by methicillin-resistant Staphylococcus aureus (MRSA) is changing. Temporal trends and differences between healthcare settings must be described in order to better predict future risk factors associated with this dangerous bacterial infection.
Methods
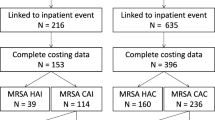
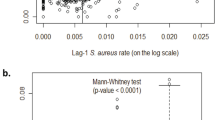
A national MRSA-infected cohort was identified from 2002 to 2009 in the Veterans Affairs Healthcare System of the United States: hospital (HOS), long-term care (LTC), and outpatient (OPT). We analyzed within-setting time trends using generalized linear mixed models and between-setting differences with χ2 and Wilcoxon rank-sum tests.
Results
The incidence of S. aureus, methicillin-susceptible S. aureus (MSSA), and MRSA infections increased significantly over time in all three settings based on modeled annual percentage changes (P < 0.001). MRSA incidence rates rose by 14, 10, and 37% per year in the HOS, LTC, and OPT settings, respectively. Among 56,345 MRSA-infected patients, the comorbidity burden was highest among LTC inpatients (n = 4,427) and lowest among outpatients (n = 7,250), with an average absolute difference in specific comorbidities of +2 and −7%, respectively, compared to HOS inpatients (n = 44,668). Over time, there was a significant (P ≤ 0.02) decrease in previous inpatient admissions and surgeries (all settings); diabetes with complications and surgical site infections (HOS, OPT); and median length of stay and inpatient mortality (HOS, LTC). Alternatively, obesity, chronic renal disease, and depression were more common between 2002 and 2009 (P ≤ 0.02).
Conclusions
Over the past 8 years, we observed significant changes in the epidemiology of MRSA infections, including decreases in traditional MRSA risk factors, improvements in clinical outcomes, and increases in other patient characteristics that may affect risk.

Similar content being viewed by others
References
Seybold U, Kourbatova EV, Johnson JG, Halvosa SJ, Wang YF, King MD, et al. Emergence of community-associated methicillin-resistant Staphylococcus aureus USA300 genotype as a major cause of health care-associated blood stream infections. Clin Infect Dis. 2006;42:647–56.
Van De Griend P, Herwaldt LA, Alvis B, DeMartino M, Heilmann K, Doern G, et al. Community-associated methicillin-resistant Staphylococcus aureus, Iowa, USA. Emerg Infect Dis. 2009;15:1582–9.
Limbago B, Fosheim GE, Schoonover V, Crane CE, Nadle J, Petit S, et al. Characterization of methicillin-resistant Staphylococcus aureus isolates collected in 2005 and 2006 from patients with invasive disease: a population-based analysis. J Clin Microbiol. 2009;47:1344–51.
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–71.
Kallen AJ, Mu Y, Bulens S, Reingold A, Petit S, Gershman K, et al. Health care-associated invasive MRSA infections, 2005–2008. JAMA. 2010;304:641–8.
Simor AE, Gilbert NL, Gravel D, Mulvey MR, Bryce E, Loeb M, et al. Methicillin-resistant Staphylococcus aureus colonization or infection in Canada: National Surveillance and Changing Epidemiology, 1995–2007. Infect Control Hosp Epidemiol. 2010;31:348–56.
McCarthy NL, Sullivan PS, Gaynes R, Rimland D. Risk factors associated with methicillin resistance among Staphylococcus aureus infections in veterans. Infect Control Hosp Epidemiol. 2010;31:36–41.
Hersh AL, Chambers HF, Maselli JH, Gonzales R. National trends in ambulatory visits and antibiotic prescribing for skin and soft-tissue infections. Arch Intern Med. 2008;168:1585–91.
Edelsberg J, Taneja C, Zervos M, Haque N, Moore C, Reyes K, et al. Trends in US hospital admissions for skin and soft tissue infections. Emerg Infect Dis. 2009;15:1516–8.
Gerber JS, Coffin SE, Smathers SA, Zaoutis TE. Trends in the incidence of methicillin-resistant Staphylococcus aureus infection in children’s hospitals in the United States. Clin Infect Dis. 2009;49:65–71.
Meyer E, Ziegler R, Mattner F, Schwab F, Gastmeier P, Martin M. Increase of patients co-colonised or co-infected with methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus faecium or extended-spectrum beta-lactamase-producing Enterobacteriaceae. Infection. 2011;39:501–6.
Rosenthal VD, Maki DG, Jamulitrat S, Medeiros EA, Todi SK, Gomez DY et al (2010) International Nosocomial Infection Control Consortium (INICC) report, data summary for 2003–2008, issued June 2009. Am J Infect Control 38:95–104 e2.
Maynard C, Chapko MK. Data resources in the Department of Veterans Affairs. Diabetes Care. 2004;27(Suppl 2):B22–6.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9.
Agency for Healthcare Research and Quality (AHRQ). Clinical classifications software (CCS), Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2010.
Klein E, Smith DL, Laxminarayan R. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999–2005. Emerg Infect Dis. 2007;13:1840–6.
US Department of Veterans Affairs, Veterans Health Administration. Methicillin-resistant Staphylococcus aureus (MRSA) initiative, VHA Directive 2007–002. Washington, DC: US Department of Veterans Affairs, Veterans Health Administration; 2007.
Garcia-Williams AG, Miller LJ, Burkitt KH, Cuerdon T, Jain R, Fine MJ, et al. Beyond beta: lessons learned from implementation of the Department of Veterans Affairs methicillin-resistant Staphylococcus aureus prevention initiative. Infect Control Hosp Epidemiol. 2010;31:763–5.
Laupland KB, Ross T, Gregson DB. Staphylococcus aureus bloodstream infections: risk factors, outcomes, and the influence of methicillin resistance in Calgary, Canada, 2000–2006. J Infect Dis. 2008;198:336–43.
Stenstrom R, Grafstein E, Romney M, Fahimi J, Harris D, Hunte G, et al. Prevalence of and risk factors for methicillin-resistant Staphylococcus aureus skin and soft tissue infection in a Canadian emergency department. CJEM. 2009;11:430–8.
Salangsang JA, Harrison LH, Brooks MM, Shutt KA, Saul MI, Muto CA. Patient-associated risk factors for acquisition of methicillin-resistant Staphylococcus aureus in a tertiary care hospital. Infect Control Hosp Epidemiol. 2010;31:1139–47.
Shorr AF, Zilberberg MD, Micek ST, Kollef MH. Prediction of infection due to antibiotic-resistant bacteria by select risk factors for health care-associated pneumonia. Arch Intern Med. 2008;168:2205–10.
Maclayton DO, Suda KJ, Coval KA, York CB, Garey KW. Case–control study of the relationship between MRSA bacteremia with a vancomycin MIC of 2 microg/mL and risk factors, costs, and outcomes in inpatients undergoing hemodialysis. Clin Ther. 2006;28:1208–16.
Crum NF, Lee RU, Thornton SA, Stine OC, Wallace MR, Barrozo C, et al. Fifteen-year study of the changing epidemiology of methicillin-resistant Staphylococcus aureus. Am J Med. 2006;119:943–51.
Sircar KD, Bancroft E, Nguyen DM, Mascola L. Hospitalization of paediatric patients for methicillin-resistant Staphylococcus aureus skin and soft-tissue infection, 1998–2006. Epidemiol Infect. 2010;138:677–82.
Kuehnert MJ, Hill HA, Kupronis BA, Tokars JI, Solomon SL, Jernigan DB. Methicillin-resistant-Staphylococcus aureus hospitalizations, United States. Emerg Infect Dis. 2005;11:868–72.
Schaefer MK, Ellingson K, Conover C, Genisca AE, Currie D, Esposito T, et al. Evaluation of International Classification of Diseases, Ninth Revision, Clinical Modification Codes for reporting methicillin-resistant Staphylococcus aureus infections at a hospital in Illinois. Infect Control Hosp Epidemiol. 2010;31:463–8.
Schweizer ML, Eber MR, Laxminarayan R, Furuno JP, Popovich KJ, Hota B, et al. Validity of ICD-9-CM coding for identifying incident methicillin-resistant Staphylococcus aureus (MRSA) infections: is MRSA infection coded as a chronic disease? Infect Control Hosp Epidemiol. 2011;32:148–54.
Singh JA, Holmgren AR, Noorbaloochi S. Accuracy of Veterans Administration databases for a diagnosis of rheumatoid arthritis. Arthritis Rheum. 2004;51:952–7.
Kern EF, Maney M, Miller DR, Tseng CL, Tiwari A, Rajan M, et al. Failure of ICD-9-CM codes to identify patients with comorbid chronic kidney disease in diabetes. Health Serv Res. 2006;41:564–80.
Acknowledgments
We gratefully acknowledge the Center on Systems, Outcomes and Quality in Chronic Disease and Rehabilitation, a Research Enhancement Award Program of the Health Services Research and Development Service, and Providence Veterans Affairs Medical Center Research Service for the data storage and software assistance. The views expressed are those of the authors and do not necessarily reflect the position or policy of the United States Department of Veterans Affairs. A.R.C. is supported by a Department of Veterans Affairs Career Development Award.
Conflict of interest
A.R. Caffrey: Pfizer research funding; K.L. LaPlante: Astellas, Cubist, Forest, Ortho-McNeil, and Pfizer research funding, advisory board, speakers bureau, and/or consultancy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Caffrey, A.R., LaPlante, K.L. Changing epidemiology of methicillin-resistant Staphylococcus aureus in the Veterans Affairs Healthcare System, 2002–2009. Infection 40, 291–297 (2012). https://doi.org/10.1007/s15010-011-0232-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-011-0232-3