Abstract
Background
Thrombocytopenia is defined as a platelet count of less than 150 × 103 μl. It is commonly diagnosed and has attracted more interest from the researchers in pregnant women during the last 20 years, especially in hypertensive pregnant women.
Aim
To assess the incidence of thrombocytopenia in hypertensive pregnant women during the third trimester of pregnancy.
Methods
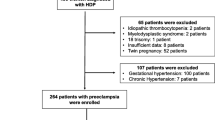
Five hundred forty-four pregnant women were included in this study from a total of 10,272 admitted at the Obstetrics and Gynecology Department at Tripoli Medical Center during January–August 2007. Frequent blood pressure monitorings and full blood counts were performed in several medical follow ups. They were not known to be HBV, HCV, or HIV positive women before pregnancy, and none was reported to have evidence of HBV, HCV, or HIV upon performing HBs-Ag, anti-HCV antibody, or HIV-antigen positive tests. Data were arranged in Excel Microsoft program version 2010, and statistically analyzed by SPSS windows program version 17.
Results
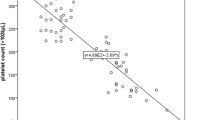
Five hundred and forty-four women were hypertensive according to WHO hypertension definition criteria. Sixty-seven women had only one reading of high blood pressure, while 39 women fulfilled HELP syndrome criteria (hemolysis elevated liver enzymes low platelet). These 39 women were excluded from the study. Therefore, only 438 pregnant women remained eligible for the study. The mean age was (32.56 ± 1.5), with their ages ranging between 18 and 49 years. Most of the included women were primigravida 179 (39 %), gravid 2, para one were 72 (16.4 %), and the rest were gravid 3 or more (42.6 %). The blood pressure was 140-160/90-110 mmHg in 365 women (83.4 %), and 73 women (16.7 %) had blood pressure readings more than 160/110 mmHg. Mean platelets count was (206.49 × 103/μl ± 3.35), and ranged between (41.0 - 449.0 × 103/μl). Thrombocytopenia (less than 150 × 103/μl) was recorded in 103 women (23.5 %). All pregnancy cases were delivered safely with no fetal complications.
Conclusion
Gestational thrombocytopenia (GT) is recognized as a major cause of thrombocytopenia particularly in hypertensive pregnant women during the third trimester. Careful follow up during and after pregnancy for those women is recommended.




Similar content being viewed by others
References
Matthews JH, Benjamin S, Gill DS, et al. Pregnancy-associated thrombocytopenia: Definition, incidence and natural history. Acta Haematol. 1990;84:24.
Boehlen F, Hohlfeld P, Extermann P, et al. Platelet count at term pregnancy: a reappraisal of the threshold. Obstet Gynecol. 2000;95:29–33.
George JN, Woolf SH, Raskob GE, et al. Idiopathic thrombocytopenic purpura: A practice guideline developed by explicit methods for the American society of haematology. Blood. 1996;88:3–10.
Burrows RF, Kelton JG. Thrombocytopenia at delivery: A prospective survey of 6175 deliveries. Am J Obstet Gynecol. 1990;162:731–4.
Burrows RF, Kelton JG. Fetal thrombocytopenia and its relation to maternal thrombocytopenia. N Engl J Med. 1993;329:1463.
Kaplan C, Forestier F, Dreyfus M, et al. Maternal thrombocytopenia during pregnancy: Diagnosis and etiology. Semin Thromb Hemost. 1995;21:85.
Tsunoda T, Ohkuchi A, Izumi A, et al. Antithrombin III activity and platelet count are more likely to decrease in twin pregnancies than in singleton pregnancies. Acta Obstet Gynecol Scand. 2002;81:840.
Letsky EA, Greaves M. Guidelines on the investigation and management of thrombocytopenia in pregnancy and neonatal alloimmune thrombocytopenia. Br J Haematol. 1996;95:21.
Moise KJ. Autoimmune thrombocytopenic purpura in pregnancy. Clin Obstet Gynecol. 1991;34:51.
Burrows RF, Kelton JG. Pregnancy in patients with idiopathic thrombocytopenic purpura: Assessing the risks for the infant at delivery. Obstet Gynecol Surv. 1993;48:781.
Saftlas AF, Olson DR, Franks AL, et al. Epidemiology of preeclampsia and eclampsia in the United States, 1979–1986. Am J Obstet Gynecol. 1990;163:460.
Sibai BM, Ramadan MK, Chari RS, et al. Pregnancies complicated by HELLP syndrome (hemolysis, elevated liver enzymes, and low platelets): Subsequent pregnancy outcome and long-term prognosis. Am J Obstet Gynecol. 1995;172:125.
Magann EF, Martin JN Jr. Twelve steps to optimal management of HELLP syndrome. Clin Obstet Gynecol. 1999;42:532–50.
Jeffrey AL, Lance DM. Thrombocytopenia in pregnancy. J Am Board Fam Pract. 2002;15:290–7.
Ajzenberg N, Dreyfus M, Kaplan C, et al. Pregnancy-associated thrombocytopenia revisited: assessment and follow-up of 50 cases. Blood. 1998;92(12):4573–80.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Habas, E., Rayani, A. & Ganterie, R. Thrombocytopenia in Hypertensive Disease of Pregnancy. J Obstet Gynecol India 63, 96–100 (2013). https://doi.org/10.1007/s13224-012-0257-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-012-0257-2