Abstract
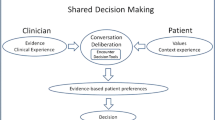
Advances in shared decision making (SDM) have not successfully translated to practice. We describe our experience and lessons learned in translating an SDM process for primary care cardiovascular disease management. The SDM process operationalized recognized SDM elements using workflow modifications, a computerized patient questionnaire, an automated risk calculator to identify at-risk patients, a web-based tool for patients to choose interventions, automated feedback on the personalized benefits of choices, and a web-based tool for providers to view patient risk, patient choice, and expert advice. Although medication was typically the intervention resulting in the greatest risk reduction, the majority of patients preferred dietary and other lifestyle changes. Patients generally favored the opportunity to make and communicate choices. However, providers only viewed patient choice data in 20% of the encounters. Translation of the SDM process was successful for patients and the difference between patient choice and optimal risk reduction points to the importance of engaging in an SDM process. Lack of engagement by providers may be due to “alert fatigue” or to the failure of the SDM process to improve efficiency in the office visit.




Similar content being viewed by others
References
Coulter, A., Entwistle, V., & Gilbert, D. (1999). Sharing decisions with patients: is the information good enough? British Medical Journal, 318(7179), 318–322.
Institute of Medicine, & Committee on Quality of Health Care in America. (2001). Crossing the quality chasm: a new health system for the 21st century. Washington, D.C.: National Academy Press.
Charles, C., Gafni, A., & Whelan, T. (1997). Shared decision-making in the medical encounter: what does it mean? (or it takes at least two to tango). Social Science & Medicine, 44(5), 681–692.
Gravel, K., Légaré, F., Graham, I. D. (2006). Barriers and facilitators to implementing shared decision-making in clinical practice: a systematic review of health professionals’ perceptions. Implementation science: IS.;1:16. http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1586024&tool=pmcentrez&rendertype=abstract; file:///Users/JB/Documents/Papers/2006/Gravel, L√©gar√©, Graham_2006_perceptions.pdf.
Légaré, F,, Ratté, S., Gravel, K., & Graham, I. D. (2008). Barriers and facilitators to implementing shared decision-making in clinical practice: update of a systematic review of health professionals’ perceptions. Patient Educ Couns, 73(3), 526–535. http://www.ncbi.nlm.nih.gov/pubmed/18752915; file:///Users/JB/Documents/Papers/2008/L√©gar√© et al._2008_Barriers and facilitators to implementing shared decision-making in clinical practice update of a systematic review of health professionals’ perceptions.pdf.
McNutt, R. A. (2004). Shared medical decision making: problems, process, progress. JAMA, 292(20), 2516–2518.
Holmes-Rovner, M., Llewellyn-Thomas, H., Entwistle, V., Coulter, A., O’Connor, A., & Rovner, D. R. (2001). Patient choice modules for summaries of clinical effectiveness: a proposal. British Medical Journal, 322(7287), 664.
Makoul, G., & Clayman, M. L. (2006). An integrative model of shared decision making in medical encounters. Patient Education and Counseling, 60(3), 301–312. doi:10.1016/j.pec.2005.06.010.
Jones, J. B., Snyder, C. F., & Wu, A. W. (2007). Issues in the design of Internet-based systems for collecting patient-reported outcomes. Quality of Life Research, 16(8), 1407–1417. doi:10.1007/s11136-007-9235-z.
Cabana, M. D., Rand, C. S., Powe, N. R., et al. (1999). Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA, 282(15), 1458.
Follow, A. (2005). JNC 7 guidelines. American Journal of Management Care, 11, S215–S219.
Grundy, S. M., Cleeman, J. I., Bairey Merz, C. N., et al. (2004). Implications of recent clinical trials for the national cholesterol education program adult treatment panel III guidelines. Journal of the American College of Cardiology, 44(3), 720–732.
O’Connor, A. M., Wennberg, J. E., Legare, F., et al. (2007). Toward the ‘tipping point’: decision aids and informed patient choice. Health Aff (Millwood), 26(3), 716–725. http://www.ncbi.nlm.nih.gov/pubmed/17485749; file:///Users/JB/Documents/Papers/2007/Connor et al._2007_Toward The ‚ÄòTipping Point‚Äô Decision Aids And Informed Patient Choice.pdf.
Gramling, R., Klein, W., Roberts, M., Waring, M. E., Gramling, D., & Eaton, C. B. (2008). Self-rated cardiovascular risk and 15-year cardiovascular mortality. Annals of Family Medicine, 6(4), 302–306.
van der Sijs, H., Aarts, J., Vulto, A., & Berg, M. (2006). Overriding of drug safety alerts in computerized physician order entry. Journal of the American Medical Informatics Association, 13(2), 138–147. doi:10.1197/jamia.M1809.
Abookire, S. A., Teich, J. M., Sandige, H., et al. (2000). Improving allergy alerting in a computerized physician order entry system. Proc AMIA Symp, 2–6.
Bates, D. W., Kuperman, G. J., Wang, S., et al. (2003). Ten commandments for effective clinical decision support: making the practice of evidence-based medicine a reality. Journal of the American Medical Informatics Association, 10(6), 523–530. doi:10.1197/jamia.M1370.
Acknowledgments
The authors would like to acknowledge AstraZeneca for funding provided for this project. The authors would also like to acknowledge editorial assistance provided by Ilene Ladd, project coordinator.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice: Key elements of shared decision making (e.g., defining the problem, presenting options, eliciting treatment preferences) can be efficiently integrated into the clinical workflow using web-based tools that improve patient satisfaction, quality of care, and productivity.
Policy: The meaningful use of health information technology for improving care quality and efficiency and for engaging patients in their healthcare will likely be enhanced by using efficient means of obtaining digital data directly from patients on risks, preferences, needs, and outcomes.
Research: There continues to be a significant gap in devising a care model that seamlessly and efficiently integrates shared decision making into the workflow in a manner that is easy for clinical practices to adopt.
About this article
Cite this article
Jones, J.B., Bruce, C.A., Shah, N.R. et al. Shared decision making: using health information technology to integrate patient choice into primary care. Behav. Med. Pract. Policy Res. 1, 123–133 (2011). https://doi.org/10.1007/s13142-011-0023-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-011-0023-5