Abstract
Background
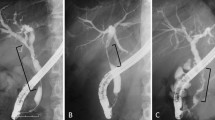
The aim of this study was to retrospectively validate a new system to predict perihilar cholangiocarcinoma (PHC) resectability. We hypothesized that when the left lateral section (segments II–III) duct confluence (LLC) is free, the left lateral section might be preserved for curative resection. When the LLC is invaded, vascular invasion is frequent and radical resection might often be impossible without complex vascular reconstruction.
Method
Radiological files of patients operated for PHC at our institution were reviewed and PHC was classified depending on whether LLC was invaded (type X) or free (type Y). Peroperative findings and follow-up were then matched with our XY classification.
Results
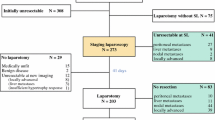
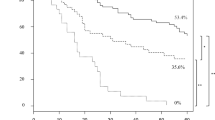
Thirty-seven patients were included, 28 (78 %) type Y and nine (22 %) type X PHCs. Hepatic artery (HA) invasion was present in 14 % of type Y and 100 % of type X PHCs (P < 0.001). Left HA was never involved in type Y and always involved in type X. Portal vein invasion was present in 25 and 78 % of type Y and type X PHC, respectively (P = 0.014). Complete resection rates without HA in type Y and X patients were 89 % (84 % R0 and 16 % R1) and 33 % (37.5 % R0 and 12.5 % R1), respectively (P = 0.01). Sensitivity, specificity, and precision of the XY classification to predict resectability were 84, 67, and 84 %, respectively.
Conclusion
XY classification for PHCs suggests that in type Y (free LLC), the tumor is most often resectable, while in type X (LLC involved), the tumor is only resectable using complex vascular reconstructions.




Similar content being viewed by others
Abbreviations
- BC:
-
Bismuth–Corlette
- RRC:
-
Right anterior and right posterior duct confluence
- RLC:
-
Right and left hepatic duct confluence
- LLC:
-
Segments II and III (left lateral section) duct confluence
- LHD:
-
Left hepatic duct
- CHD:
-
Common hepatic duct
- MRI:
-
Magnetic resonance imaging
- MRC:
-
Magnetic resonance cholangiography
- MDCT:
-
Multidetector computed tomography
References
Nakeeb A, Pitt HA, Sohn TA et al. Cholangiocarcinoma, a spectrum of intrahepatic, perihilar and distal tumors. Ann Surg 1996;224 :463–473.
Ebata T, Kamiya J, Nishio H, Nagasaka T, Nimura Y, Nagino M. The concept of perihilar cholangiocarcinoma is valid. Brit J Surg 2009;96:926–34.
Launois B, Campion JP, Brissot P, Gosselin M. Carcinoma of the hepatic hilus. Surgical management and the case for resection. Ann Surg 1979; 190:151–157.
Jarnagin WR, Fong Y, DeMatteo RP et al. Staging, resectability, and outcome in 225 patients with hilar cholangiocarcinoma. Ann Surg 2001;234:507–19.
Neuhaus P, Jonas S, Bechstein WO et al. Extended resections for hilar cholangiocarcinoma. Ann Surg 1999;230:808–18.
Ito F, Cho CS, Rikkers LF et al. Hilar cholangiocarcinoma: current management. Ann Surg 2009;250:210–8.
Paik WH, Park YS, Hwang JH et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc 2009;69:55–62.
Hemming AW, Reed AI, Fujita S et al. Surgical management of hilar cholangiocarcinoma. Ann Surg 2005;241:693–9.
Bismuth H, Corlette MB. Intrahepatic cholangioenteric anastomosis in carcinoma of the hilus of the liver. Surg Gynecol Obstet 1975;140:170–8.
Paul A, Kaiser GM, Molmenti EP et al. Klatskin tumors and the accuracy of the Bismuth–Corlette classification. Am Surg. 2011;77:1695–9.
Launois B, Terblanche J, Lakehal M et al. Proximal bile duct cancer: high resectability rate and 5-year survival. Ann Surg 1999;230:266–75.
Grandadam S, Compagnon P, Arnaud A et al. Role of preoperative optimization of the liver for resection in patients with hilar cholangiocarcinoma type III. Ann Surg Oncol 2010;17:3155–61.
Shimizu H, Kimura F, Yoshidome H et al. Aggressive surgical resection for hilar cholangiocarcinoma of the left-side predominance: radicality and safety of left-sided hepatectomy. Ann Surg 2010;251:281–6.
Lee SG, Song GW, Hwang S et al. Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci 2010;17:476–89.
Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg. 2005;12:351–5.
Kim MJ, Mitchell DG, Ito K et al. Biliary dilatation: differentiation of benign from malignant causes—value of adding conventional MR imaging to MR cholangiopancreatography. Radiology 2000; 214:173–81.
Lu DSK, Reber HA, Krasny RM, et al. Local staging of pancreatic cancer: criteria for unresectability of major vessels as revealed by pancreatic phase thin-section helical CT. Am J Roentgenol 1997;168:1439–43.
Miyazaki M, Kato A, Ito H et al. Combined vascular resection in operative resection for hilar cholangiocarcinoma: does it work or not? Surgery 2007;141: 581–88.
Shingu Y Ebata T, Nishio H et al. Clinical value of additional resection of a margin-positive proximal bile duct in hilar cholangiocarcinoma. Surgery 2010;147:50–57.
Okazaki Y, Horimi T, Kotaka M et al. Study of the intrahepatic surgical margin of hilar bile duct carcinoma. Hepatogastroenterology 2002;49:625–627.
Ikeyama T, Nagino M, Oda K et al. Surgical approach to Bismuth type I and II hilar cholangiocarcinomas. Ann Surg 2007;246:1052–57.
Couinaud C. Tell me more about liver anatomy. Paris: Karger;1999.
Hiatt JR, Gabbay J, Busuttil R. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 1994;220:50–52.
Natsume S, Ebata T, Yokoyama Y et al. Clinical significance of left trisectionectomy for perihilar cholangiocarcinoma: an appraisal and comparaison with left hepatectomy. Ann Surg 2012;255:754–62.
Neuhaus P, Thelen A, Jonas A et al. Oncological superiority of hilar en bloc resection for the treatment of hilar cholangiocarcinoma. Ann Surg Oncol 2012;19:1602–8.
Schnitzbauer AA, Lang SA, Goessmann H, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg 2012;255:405–14.
Acknowledgments
The authors thank Peter Tucker for his help in reviewing the manuscript.
Conflict of Interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Boudjema, K., Sulpice, L., Garnier, S. et al. A Simple System to Predict Perihilar Cholangiocarcinoma Resectability. J Gastrointest Surg 17, 1247–1256 (2013). https://doi.org/10.1007/s11605-013-2215-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-013-2215-4