Abstract
Purpose
A wide variety of hydrophilic imaging and therapeutic agents are unable to gain access to the central nervous system (CNS) due to the blood-brain barrier (BBB). In particular, unless a particular transporter exists that may transport the agent across the BBB, most agents that are larger than 500 Da or that are hydrophilic will be excluded by the BBB. Glutamate carboxypeptidase II (GCPII), also known as the prostate-specific membrane antigen (PSMA) in the periphery, has been implicated in various neuropsychiatric conditions. As all agents that target GCPII are hydrophilic and thereby excluded from the CNS, we used GCPII as a platform for demonstrating our MR-guided focused ultrasound (MRgFUS) technique for delivery of GCPII/PSMA-specific imaging agents to the brain.
Procedures
Female rats underwent MRgFUS-mediated opening of the BBB. After opening of the BBB, either a radio- or fluorescently labeled ureido-based ligand for GCPII/PSMA was administered intravenously. Brain uptake was assessed for 2-(3-{1-carboxy-5-[(6-[18F]fluoro-pyridine-3-carbonyl)-amino]-pentyl}-ureido)-pentanedioic acid ([18F]DCFPyL) and YC-27, two compounds known to bind GCPII/PSMA with high affinity, using positron emission tomography (PET) and near-infrared fluorescence (NIRF) imaging, respectively. Specificity of ligand binding to GCPII/PSMA in the brain was determined with co-administration of a molar excess of ZJ-43, a compound of the same chemical class but different structure from either [18F]DCFPyL or YC-27, which competes for GCPII/PSMA binding.
Results
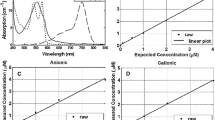
Dynamic PET imaging using [18F]DCFPyL demonstrated that target uptake reached a plateau by ∼1 h after radiotracer administration, with target/background ratios continuing to increase throughout the course of imaging, from a ratio of ∼4:1 at 45 min to ∼7:1 by 80 min. NIRF imaging likewise demonstrated delivery of YC-27 to the brain, with clear visualization of tracer in the brain at 24 h. Tissue uptake of both ligands was greatly diminished by ZJ-43 co-administration, establishing specificity of binding of each to GCPII/PSMA. On gross and histological examination, animals showed no evidence for hemorrhage or other deleterious consequences of MRgFUS.
Conclusions
MRgFUS provided safe opening of the BBB to enable specific delivery of two hydrophilic agents to target tissues within the brain. This platform might facilitate imaging and therapy using a variety of agents that have heretofore been excluded from the CNS.




Similar content being viewed by others
References
Parrish KE, Sarkaria JN, Elmquist WF (2015) Improving drug delivery to primary and metastatic brain tumors: strategies to overcome the blood-brain barrier. Clin Pharmacol Ther 97:336–346
Wernicke AG, Edgar MA, Lavi E, et al. (2011) Prostate-specific membrane antigen as a potential novel vascular target for treatment of glioblastoma multiforme. Arch Pathol Lab Med 135:1486–1489
Kim M-J, Chae SS, Koh YH, et al. (2010) Glutamate carboxypeptidase II: an amyloid peptide-degrading enzyme with physiological function in the brain. FASEB J 24:4491–4502
Bařinka C, Rojas C, Slusher B, Pomper M (2012) Glutamate carboxypeptidase II in diagnosis and treatment of neurologic disorders and prostate cancer. Curr Med Chem 19:856–870
Szabo Z, Mena E, Rowe SP, et al. (2015) Initial evaluation of [(18)F]DCFPyL for prostate-specific membrane antigen (PSMA)-targeted PET imaging of prostate cancer. Mol Imaging Biol 17:565–574
Eiber M, Weirich G, Holzapfel K, et al. (2016) Simultaneous (68)Ga-PSMA HBED-CC PET/MRI improves the localization of primary prostate cancer. Eur Urol. doi:10.1016/j.eururo.2015.12.053
Rai BP, Baum R, Patel A, et al. (2016) The role PET with (68)gallium (Ga)-labelled prostate-specific membrane antigen (PSMA) in the Management of Patient with organ confined and locally advanced prostate cancer prior to radical treatment and after radical prostatectomy. Urology. doi:10.1016/j.urology.2015.12.048
Haberkorn U, Eder M, Kopka K, et al. (2016) New strategies in prostate cancer: prostate-specific membrane antigen (PSMA) ligands for diagnosis and therapy. Clin Cancer Res 22:9–15
Lütje S, Heskamp S, Cornelissen AS, et al. (2015) PSMA ligands for radionuclide imaging and therapy of prostate cancer: clinical status. Theranostics 5:1388–1401
Chen Y, Pullambhatla M, Foss CA, et al. (2011) 2-(3-{1-Carboxy-5-[(6-[18F]fluoro-pyridine-3-carbonyl)-amino]-pentyl}-ureido)-pentanedioic acid, [18F]DCFPyL, a PSMA-based PET imaging agent for prostate cancer. Clin Cancer Res 17:7645–7653
Wroblewska B, Santi MR, Neale JH (1998) N-acetylaspartylglutamate activates cyclic AMP-coupled metabotropic glutamate receptors in cerebellar astrocytes. Glia 24:172–179
Berger UV, Luthi-Carter R, Passani LA, et al. (1999) Glutamate carboxypeptidase II is expressed by astrocytes in the adult rat nervous system. J Comp Neurol 415:52–64
Sácha P, Zámecník J, Barinka C, et al. (2007) Expression of glutamate carboxypeptidase II in human brain. Neuroscience 144:1361–1372
Wang H, Byun Y, Barinka C, et al. (2010) Bioisosterism of urea-based GCPII inhibitors: synthesis and structure-activity relationship studies. Bioorg Med Chem Lett 20:392–397
Ferraris DV, Majer P, Ni C, et al. (2014) δ-Thiolactones as prodrugs of thiol-based glutamate carboxypeptidase II (GCPII) inhibitors. J Med Chem 57:243–247
Nance E, Timbie K, Miller GW, et al. (2014) Non-invasive delivery of stealth, brain-penetrating nanoparticles across the blood-brain barrier using MRI-guided focused ultrasound. J Control Release 189:123–132
Huang Y, Hynynen K (2010) MR-guided focused ultrasound for brain ablation and blood-brain barrier disruption. Methods Mol Biol 711:579–593
McDannold N, Vykhodtseva N, Raymond S, et al. (2005) MRI-guided targeted blood-brain barrier disruption with focused ultrasound: histological findings in rabbits. Ultrasound Med Biol 31:1527–1537
Downs ME, Buch A, Sierra C, et al. (2015) Long-term safety of repeated blood-brain barrier opening via focused ultrasound with microbubbles in non-human primates performing a cognitive task. PLoS One 10:e0125911
InSightec, Mainprize T (2015) Blood-brain barrier disruption using transcranial MRI-guided focused ultrasound. In: Clin. Natl. Libr. Med. https://clinicaltrials.gov/ct2/show/NCT02343991.
Burgess A, Hynynen K (2013) Noninvasive and targeted drug delivery to the brain using focused ultrasound. ACS Chem Neurosci 4:519–526
Kinoshita M, McDannold N, Jolesz FA, Hynynen K (2006) Noninvasive localized delivery of Herceptin to the mouse brain by MRI-guided focused ultrasound-induced blood-brain barrier disruption. Proc Natl Acad Sci U S A 103:11719–11723
Hsu P-H, Wei K-C, Huang C-Y, et al. (2013) Noninvasive and targeted gene delivery into the brain using microbubble-facilitated focused ultrasound. PLoS One 8:e57682
Burgess A, Ayala-Grosso CA, Ganguly M, et al. (2011) Targeted delivery of neural stem cells to the brain using MRI-guided focused ultrasound to disrupt the blood-brain barrier. PLoS One 6:e27877
Mullin L, Gessner R, Kwan J, et al. Effect of anesthesia carrier gas on in vivo circulation times of ultrasound microbubble contrast agents in rats. Contrast Media Mol Imaging 6:126–131
O’Reilly MA, Muller A, Hynynen K (2011) Ultrasound insertion loss of rat parietal bone appears to be proportional to animal mass at submegahertz frequencies. Ultrasound Med Biol 37:1930–1937
Song J, Klibanov AL, Hossack JA, Price RJ (2008) Acoustic attenuation by contrast agent microbubbles in superficial tissue markedly diminishes petechiae bioeffects in deep tissue. Investig Radiol 43:322–329
Alkins R, Burgess A, Ganguly M, et al. (2013) Focused ultrasound delivers targeted immune cells to metastatic brain tumors. Cancer Res 73:1892–1899
Paefgen V, Doleschel D, Kiessling F (2015) Evolution of contrast agents for ultrasound imaging and ultrasound-mediated drug delivery. Front Pharmacol 6:197
Bayer-Healthcare (2016) Magnevist Package Insert. http://labeling.bayerhealthcare.com/html/products/pi/Magnevist_PI.pdf.
Jacobson M, Levkovitz R, Ben-Tal A, et al. (2000) Enhanced 3D PET OSEM reconstruction using inter-update Metz filtering. Phys Med Biol 45:2417–2439
Chen Y, Dhara S, Banerjee SR, et al. (2009) A low molecular weight PSMA-based fluorescent imaging agent for cancer. Biochem Biophys Res Commun 390:624–629
McDannold N, Arvanitis CD, Vykhodtseva N, Livingstone MS (2012) Temporary disruption of the blood-brain barrier by use of ultrasound and microbubbles: safety and efficacy evaluation in rhesus macaques. Cancer Res 72:3652–3663
Burgess A, Shah K, Hough O, Hynynen K (2015) Focused ultrasound-mediated drug delivery through the blood–brain barrier. Expert Rev Neurother 15:477–491
Yamamoto T, Hirasawa S, Wroblewska B, et al. (2004) Antinociceptive effects of N-acetylaspartylglutamate (NAAG) peptidase inhibitors ZJ-11, ZJ-17 and ZJ-43 in the rat formalin test and in the rat neuropathic pain model. Eur J Neurosci 20:483–494
Pardridge WM (1997) Drug delivery to the brain. J Cereb Blood Flow Metab 17:713–731
Calias P, Banks WA, Begley D, et al. (2014) Intrathecal delivery of protein therapeutics to the brain: a critical reassessment. Pharmacol Ther 144:114–122
Airan RD, Clement GT, Partanen A, et al. (2015) Expanding the treatment envelope for transcranial MR-guided focused ultrasound with a 256-element clinical transducer. ISMRM Conf. Proc.
Acknowledgments
The authors are grateful for grant and in-kind support for this research from Philips Healthcare, the Walter and Mary Ciceric Foundation, and the National Institutes of Health (grant numbers: CA134675, CA184228). The authors also wish to acknowledge the Johns Hopkins Cyclotron Lab for the provision of surplus cGMP [18F]DCFPyL during these studies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors (RDA, NPKE, KF, MGP) received limited grant funding and support in kind for this work from Philips Healthcare. Under a licensing agreement between Progenics and the Johns Hopkins University, Dr. Pomper is entitled to royalties on an invention described in this article. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies.
Rights and permissions
About this article
Cite this article
Airan, R.D., Foss, C.A., Ellens, N.P.K. et al. MR-Guided Delivery of Hydrophilic Molecular Imaging Agents Across the Blood-Brain Barrier Through Focused Ultrasound. Mol Imaging Biol 19, 24–30 (2017). https://doi.org/10.1007/s11307-016-0985-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-016-0985-2