Abstract
Purpose
Nebulization represents one strategy to achieve pulmonary deposition of biodegradable nanoparticles. Besides stability as a key requirement to maintain functionality, the output of nanoparticles from the nebulizer needs to be considered to facilitate an efficient pulmonary therapy.
Methods
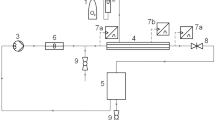
Formulations nebulized by air-jet and vibrating-membrane technology were analyzed for their aerodynamic characteristics by laser diffraction. The nebulization stability of poly(D,L-lactide-co-glycolide) nanoparticles was assessed by dynamic light scattering. Moreover, several methods were employed to account for the shift in solute and NP reservoir concentration during nebulization.
Results
Regardless of the formulation or nebulizer used generated aerosols all showed aerodynamic characteristics suitable for deep lung deposition. However, nanoparticles were prone to aggregation and concentrated during air-jet nebulization. The particle concentration effect was significantly pronounced in comparison to molecular solutes under the same nebulization conditions, due to nanoparticle aggregation and subsequent particle remainder in the reservoir. In contrast, vibrating-membrane technology did not affect nanoparticle integrity and reservoir concentration during nebulization, as the unaffected submicron particles passed through the tapered holes of the actuated plate.
Conclusions
Aggregation and concentration effects during air-jet nebulization emphasize that nanosuspensions should preferably be delivered with a suitable vibrating-membrane device in order to ensure an effective pulmonary application.




Similar content being viewed by others
Abbreviations
- CF:
-
5(6)-carboxyfluorescein
- DLS:
-
dynamic light scattering
- DMSO:
-
dimethyl sulfoxide
- FPF:
-
fine particle fraction
- GSD:
-
geometric standard deviation
- LDA:
-
laser Doppler anemometry
- MWCO:
-
molecular weight cut-off
- NP:
-
nanoparticles
- PDI:
-
polydispersity index
- PLGA:
-
poly(D,L-lactide-co-glycolide)
- S.D.:
-
standard deviation
- TEM:
-
transmission electron microscopy
- THF:
-
tetrahydrofuran
- UV/Vis:
-
ultra violet/visible
- VMD:
-
volume median diameter
References
Olschewski H, Simonneau G, Galie N, Higenbottam T, Naeije R, Rubin LJ, et al. Inhaled iloprost for severe pulmonary hypertension. N Engl J Med. 2002;347:322–9.
Patton JS, Byron PR. Inhaling medicines: Delivering drugs to the body through the lungs. Nat Rev Drug Discov. 2007;6:67–74.
van der Schans CP. Bronchial mucus transport. Respir Care. 2007;52:1150–8.
Geiser M. Update on macrophage clearance of inhaled micro- and nanoparticles. J Aerosol Med. 2010;23:207–17.
Gessler T, Seeger W, Schmehl T. The potential for inhaled treprostinil in the treatment of pulmonary arterial hypertension. Ther Adv Respir Dis. 2011;5:195–206.
Beck-Broichsitter M, Gauss J, Packhaeuser CB, Lahnstein K, Schmehl T, Seeger W, et al. Pulmonary drug delivery with aerosolizable nanoparticles in an ex vivo lung model. Int J Pharm. 2009;367:169–78.
Beck-Broichsitter M, Gauss J, Gessler T, Seeger W, Kissel T, Schmehl T. Pulmonary targeting with biodegradable salbutamol-loaded nanoparticles. J Aerosol Med. 2010;23:47–57.
Nielsen EJB, Nielsen JM, Becker D, Karlas A, Prakash H, Glud SZ, et al. Pulmonary gene silencing in transgenic EGFP mice using aerosolised chitosan/siRNA nanoparticles. Pharm Res. 2010;27:2520–7.
Rytting E, Bur M, Cartier R, Bouyssou T, Wang X, Krueger M, et al. In vitro and in vivo performance of biocompatible negatively-charged salbutamol-loaded nanoparticles. J Controlled Release. 2010;141:101–7.
Beck-Broichsitter M, Merkel OM, Kissel T. Controlled pulmonary drug and gene delivery using polymeric nano-carriers. J Controlled Release. 2011:doi:10.1016/j.jconrel.2011.1012.1004.
Dolovich MB, Dhand R. Aerosol drug delivery: developments in device design and clinical use. Lancet. 2011;377:1032–45.
Steckel H, Eskandar F. Factors affecting aerosol performance during nebulization with jet and ultrasonic nebulizers. Eur J Pharm Sci. 2003;19:443–55.
Watts AB, McConville JT, Williams III RO. Current therapies and technological advances in aqueous aerosol drug delivery. Drug Dev Ind Pharm. 2008;34:913–22.
Lass JS, Sant A, Knoch M. New advances in aerosolised drug delivery: vibrating membrane nebuliser technology. Expert Opin Drug Delivery. 2006;3:693–702.
Waldrep JC, Dhand R. Advanced nebulizer designs employing vibrating mesh/aperture plate technologies for aerosol generation. Curr Drug Delivery. 2008;5:114–9.
Chow AHL, Tong HHY, Chattopadhyay P, Shekunov BY. Particle engineering for pulmonary drug delivery. Pharm Res. 2007;24:411–37.
Sung JC, Padilla DJ, Garcia-Contreras L, VerBerkmoes JL, Durbin D, Peloquin CA, et al. Formulation and pharmacokinetics of self-assembled rifampicin nanoparticle systems for pulmonary delivery. Pharm Res. 2009;26:1847–55.
Lebhardt T, Roesler S, Uusitalo HP, Kissel T. Surfactant-free redispersible nanoparticles in fast-dissolving composite microcarriers for dry-powder inhalation. Eur J Pharm Biopharm. 2011;78:90–6.
Beck-Broichsitter M, Schweiger C, Schmehl T, Gessler T, Seeger W, Kissel T. Characterization of novel spray-dried polymeric particles for controlled pulmonary drug delivery. J Controlled Release. 2012;158:329–35.
Dailey LA, Kleemann E, Wittmar M, Gessler T, Schmehl T, Roberts C, et al. Surfactant-free, biodegradable nanoparticles for aerosol therapy based on the branched polyesters, DEAPA-PVAL-g-PLGA. Pharm Res. 2003;20:2011–20.
Dailey LA, Schmehl T, Gessler T, Wittmar M, Grimminger F, Seeger W, et al. Nebulization of biodegradable nanoparticles: Impact of nebulizer technology and nanoparticle characteristics on aerosol features. J Controlled Release. 2003;86:131–44.
Packhäuser CB, Lahnstein K, Sitterberg J, Schmehl T, Gessler T, Bakowsky U, et al. Stabilization of aerosolizable nano-carriers by freeze-drying. Pharm Res. 2009;26:129–38.
Beck-Broichsitter M, Kleimann P, Gessler T, Seeger W, Kissel T, Schmehl T. Nebulization performance of biodegradable sildenafil-loaded nanoparticles using the Aeroneb® Pro: Formulation aspects and nanoparticle stability to nebulization. Int J Pharm. 2012;422:398–408.
Hureaux J, Lagarce F, Gagnadoux F, Vecellio L, Clavreul A, Roger E, et al. Lipid nanocapsules: Ready-to-use nanovectors for the aerosol delivery of paclitaxel. Eur J Pharm Biopharm. 2009;73:239–46.
McCallion ONM, Taylor KMG, Thomas M, Taylor AJ. Nebulisation of monodisperse latex sphere suspensions in air-jet and ultrasonic nebulisers. Int J Pharm. 1996;133:203–14.
Beck-Broichsitter M, Rytting E, Lebhardt T, Wang X, Kissel T. Preparation of nanoparticles by solvent displacement for drug delivery: A shift in the “ouzo region” upon drug loading. Eur J Pharm Sci. 2010;41:244–53.
Mitchell JP, Nagel MW, Nichols S, Nerbrink O. Laser diffractometry as a technique for the rapid assessment of aerosol particle size from inhalers. J Aerosol Med. 2006;19:409–33.
Hinds WC. Aerosol technology: properties, behavior, and measurements of airborne particles. New York: Wiley; 1998.
Beck-Broichsitter M, Thieme M, Nguyen J, Schmehl T, Gessler T, Seeger W, et al. Novel’nano in nano’ composites for sustained drug delivery: Biodegradable nanoparticles encapsulated into nanofiber non-wovens. Macromol Biosci. 2010;10:1527–35.
Groneberg DA, Witt C, Wagner U, Chung KF, Fischer A. Fundamentals of pulmonary drug delivery. Respir Med. 2003;97:382–7.
Carvalho TC, Peters JI, Williams III RO. Influence of particle size on regional lung deposition: what evidence is there? Int J Pharm. 2011;406:1–10.
Fink JB, Power J. Comparison of a novel aerosol generator with a standard ultrasonic nebulizer designed for use during mechanical ventilation (Abstract). Am J Respir Crit Care Med. 2001;163:A127.
LaVan DA, Lynn DM, Langer R. Moving smaller in drug discovery and delivery. Nat Rev Drug Discov. 2002;1:77–84.
Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3:16–20.
Couvreur P, Vauthier C. Nanotechnology: Intelligent design to treat complex disease. Pharm Res. 2006;23:1417–50.
Vauthier C, Bouchemal K. Methods for the preparation and manufacture of polymeric nanoparticles. Pharm Res. 2009;26:1025–58.
Acknowledgments AND DISCLOSURES
The authors would like to thank Michael Hellwig and Andreas K. Schaper (Department of Geosciences and Materials Science Center, University of Marburg) for their support with TEM. This study was supported by the German Research Foundation (DFG). We want to express our sincere thanks for this grant.
The authors disclose that no conflicting interests associated with the manuscript exist.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Beck-Broichsitter, M., Knuedeler, MC., Schmehl, T. et al. Following the Concentration of Polymeric Nanoparticles During Nebulization. Pharm Res 30, 16–24 (2013). https://doi.org/10.1007/s11095-012-0819-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-012-0819-0