Abstract
Aim
Surgical site infection is commonly caused by Staphylococcus aureus. The multiresistant strains (MRSA) are resistant to most antibiotic prophylaxis regimens. Our aim was to explore whether there is a threshold of MRSA prevalence at which switching to routine glycopeptide-based antibiotic prophylaxis becomes cost-effective.
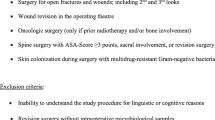
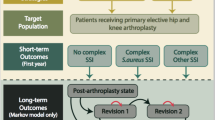
Methods
An indicative model was designed to explore the cost-effectiveness of vancomycin, cephalosporin or a combination, in patients undergoing primary hip arthroplasty.
Results
If the MRSA infection rate is equal to or above 0.25% and the rate of other infections with cephalosporin prophylaxis is equal to or above 0.2%, use of the combination antibiotic prophylaxis is optimal.
Discussion
Modelling the cost-effectiveness of interventions for MRSA prevention is complex due to uncertainty around resistance and effectiveness of glycopeptides.
Conclusions
The indicative model provides a framework for evaluation. More work is needed to understand the impact of antibiotic resistance over time in these currently effective antibiotics.

Similar content being viewed by others
References
National Institute for Health and Clinical Excellence (NICE): Costing statement: surgical site infection: prevention and treatment of surgical site infection. http://www.nice.org.uk/nicemedia/pdf/CG74CostStatement2.pdf (2008). Accessed 1 Mar 2009
Coello, R., Charlett, A., Wilson, J., Ward, V., Pearson, A., Borriello, P.: Adverse impact of surgical site infections in English hospitals. J Hosp Infect 60(2), 93–103 (2005). doi:10.1016/j.jhin.2004.10.019
Scottish Intercollegiate Guidelines Network: Antibiotic prophylaxis in surgery. Scottish Intercollegiate Guidelines Network, editor. http://www.sign.ac.uk/guidelines/fulltext/45/index.html (2000). Edinburgh. Accessed 27 Jun 2007
Nosocomial Infection National Surveillance Service: Surveillance of surgical site infection in English hospitals 1997–2002. http://www.hpa.org.uk/infections/topics_az/hai/SSIreport.pdf (2002). London: Public Health Laboratory Service. Accessed 27 Jun 2007
Gemmell, C.G., Edwards, D.I., Fraise, A.P. et al.: Guidelines for the prophylaxis and treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections in the UK. J. Antimicrob. Chemother. 57(589), 608 (2006)
Struelens, M.J.: The epidemiology of antimicrobial resistance in hospital acquired infections: problems and possible solutions. BMJ 317, 652–654 (1998)
Gemmell, C.G., Edwards, D.I., Fraise, A.P. et al.: Guidelines for the prophylaxis and treatment of meticillin (methicillin)-resistant Staphylococcus aureus (MRSA) infections in the United Kingdom. http://www.bsac.org.uk/_db/_documents/MRSA_treatment_consultation.pdf Accessed 1 Mar 2005
Chang, S., Sievert, D.M., Hageman, J.C., Boulton, M.L., Tenover, F.C., Downes, F.P.: Infection with vancomycin-resistant Staphylococcus aureus containing the vanA resistance gene. N Engl J Med 348, 1342–1347 (2003). doi:10.1056/NEJMoa025025
Tenover, F.C., Biddle, J.W., Lancaster, M.V.: Increasing resistance to vancomycin and other glycopeptides in Staphylococcus aureus. Emerg Infect Dis 7, 327–332 (2001)
Aucken, H.M., Ganner, M., Murchan, S., Cookson, B.D., Johnson, A.P.: A new UK strain of epidemic methicillin-resistant Staphylococcus aureus (EMRSA-17) resistant to multiple antibiotics. J Antimicrob Chemother 50, 171–175 (2002). doi:10.1093/jac/dkf117
Bertrand, X., Hocquet, D., Thouverez, M., Plesiat, P., Talon, D.: Characterisation of methicillin-resistant Staphylococcus aureus with reduced susceptibility to teicoplanin in Eastern France. Eur J Clin Microbiol Infect Dis 22, 504–506 (2003). doi:10.1007/s10096-003-0966-7
Mohaved, M.R., Kasravi, B., Bryan, C.S.: Prophylactic use of vancomycin in adult cardiology and cardiac surgery. J Cardiovasc Pharmacol Ther 9, 13–20 (2004). doi:10.1177/107424840400900i103
Drummond, M., Sculpher, M.J., Torrance, G., O’Brien, B.J., Stoddart, G.L.: Methods for the economic evaluation of health care programmes, 3rd edn. Oxford University Press, Oxford (2005)
Cranny, G., Elliott, R.A., Weatherly, H., et al.: A systematic review and economic model of switching from non-glycopeptide to glycopeptide antibiotic prophylaxis for surgery. Health Technol Assess 12, 1–200 (2008)
Zanetti, G., Goldie, S.J., Platt, R.: Clinical consequences and cost of limiting use of vancomycin for perioperative prophylaxis: example of coronary artery bypass surgery. Emerg Infect Dis 7, 820–827 (2001)
Rahman, M.H., Anson, J.: Peri-operative antibacterial prophylaxis. Pharm J 272, 743–745 (2004)
British Orthopaedic Association: Total hip replacement: a guide to best practice. British Orthopaedic Association, London (1999)
Department of Health: Bacteraemia surveillance scheme, MRSA bacteraemia by NHS Trust: table 2 data for each 6 months, 2001–2005. http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsStatistics/PublicationsStatisticsArticle/fs/en?CONTENT_ID=4085951&chk=HBt2QD (2005). Accessed 7 Nov 2005
Ridgeway, S., Wilson, J., Charlet, A., Kafatos, G., Pearson, A., Coello, R.: Infection of the surgical site after arthroplasty of the hip. J Bone Joint Surg Br 87-B(6), 844–850 (2005). doi:10.1302/0301-620X.87B6.15121
Finkelstein, R., Rabino, G., Mashiah, T., Bar-El, Y., Adler, Z., Kertzman, V.: Vancomycin versus cefazolin prophylaxis for cardiac surgery in the setting of a high prevalence of methicillin-resistant staphylococcal infections. J Thorac Cardiovasc Surg 123, 326–332 (2002). doi:10.1067/mtc.2002.119698
Kitzis, M., Branger, C., Andreassian, B.: Antimicrobial prophylaxis with vancomycin a comparative study in vascular surgery. Interscience Conference on Antimicrobial Agents and Chemotherapy. Program and abstracts of the Thirty-First Interscience Conference on Antimicrobial Agents and Chemotherapy, 254. (1991)
Niederman, M.S.: Impact of antibiotic resistance on clinical outcomes and the cost of care. Crit. Care. Med. 29 Suppl (4), N114–N120 (2001). doi:10.1097/00003246-200104001-00011
Tengs, T.O., Wallace, A.: One thousand health-related quality-of-life estimates. Med Care 38, 583–637 (2000). doi:10.1097/00005650-200006000-00004
National Institute for Clinical Excellence: Guide to the methods of technology appraisal. http://www.nice.org.uk/pdf/TAP_Methods.pdf (2004). Accessed 15 May 2006
Blom, A.W., Taylor, A.H., Pattison, G., Whitehouse, S., Bannister, G.C.: Infection after total hip arthroplasty: the Avon experience. J. Bone Joint. Surg. 85-B, 956–959 (2003)
Kunori, T., Cookson, B., Roberts, J.A., Stone, S., Kibbler, C.: Cost-effectiveness of different MRSA screening methods. J Hosp. Infect. 51, 189–200 (2002). doi:10.1053/jhin.2002.1247
Briggs, A., Goeree, R., Blackhouse, G., O’Brien, B.J.: Probabilistic analysis of cost-effectiveness models: choosing between treatment strategies for gastroesophageal reflux disease. Med. Decis. Making 22, 290–308 (2002)
Lodise, T.P., McKinnon, P.S., Rybak, M.: Prediction model to identify patients with Staphylococcus aureus bacteremia at risk for methicillin resistance. Infect. Control Hosp. Epidemiol 24, 655–661 (2003). doi:10.1086/502269
NHS Centre for Reviews and Dissemination: Antimicrobial prophylaxis in colorectal surgery. Eff. Health Care Bull. 4, 1–8 (1998)
Brisson, M., Edmunds, W.J.: Economic evaluation of vaccination programs: the impact of herd-immunity. Med. Decis. Making 23, 76–82 (2003). doi:10.1177/0272989X02239651
Edmunds, W.J., Medley, G.F., Nokes, D.J.: Evaluating the cost-effectiveness of vaccination programmes: a dynamic perspective. Stat. Med. 18, 3263–3282 (1999). doi:10.1002/(SICI)1097-0258(19991215)18:23<3263::AID-SIM315>3.0.CO;2-3
Smith, R.D., Yago, M., Millar, M., Coast, J.: Assessing the macroeconomic impact of a healthcare problem: the application of computable general equilibrium analysis to antimicrobial resistance. J. Health Econ. 24, 1055–1075 (2005). doi:10.1016/j.jhealeco.2005.02.003
Netten, A., Dennett, J.: Unit costs of community care. ISBN 1092671406. Personal Social Services Research Unit, Kent (2005)
British Medical Association and Royal Pharmaceutical Society of Great Britain: British National Formulary, 50th edn. (2005)
Acknowledgment
This project was funded by the NIHR Health Technology Assessment Programme (project number 05/36/01) (http://www.ncchta.org).
Author information
Authors and Affiliations
Corresponding author
Additional information
The full version of this project is available for download at http://www.ncchta.org/project/1505.asp
Rights and permissions
About this article
Cite this article
Elliott, R.A., Weatherly, H.L.A., Hawkins, N.S. et al. An economic model for the prevention of MRSA infections after surgery: non-glycopeptide or glycopeptide antibiotic prophylaxis?. Eur J Health Econ 11, 57–66 (2010). https://doi.org/10.1007/s10198-009-0175-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-009-0175-0
Keywords
- Economic model
- Surgical site infection
- Antimicrobial prophylaxis
- Glycopeptide
- Methicillin-resistant Staphylococcus aureus