Abstract
Ten percent of all strokes occurring in the USA are caused by intracranial arterial stenosis (IAS). Symptomatic IAS carries one of the highest rates of recurrent stroke despite intensive medical therapy (25 % in high-risk groups). Clinical results for endovascular angioplasty and stenting have been disappointing. The objectives of this study were to review the contemporary understanding of symptomatic IAS and present potential alternative treatments to resolve factors not addressed by current therapies. We performed a literature review on IAS pathophysiology, natural history, and current treatment. We present an evaluation of the currently deficient aspects in its treatment and explore the role of alternative surgical approaches. There is a well-documented interrelation between hemodynamic and embolic factors in cerebral ischemia caused by IAS. Despite the effectiveness of medical therapy, hemodynamic factors are not addressed satisfactorily by medications alone. Collateral circulation and severity of stenosis are the strongest predictors of risk for stroke and death. Indirect revascularization techniques, such as encephaloduroarteriosynangiosis, offer an alternative treatment to enhance collateral circulation while minimizing risk of hemorrhage associated with hyperemia and endovascular manipulation, with promising results in preliminary studies on chronic cerebrovascular occlusive disease. Despite improvements in medical management for IAS, relevant aspects of its pathophysiology are not resolved by medical treatment alone, such as poor collateral circulation. Surgical indirect revascularization can improve collateral circulation and play a role in the treatment of this condition. Further formal evaluation of indirect revascularization for IAS is a logical and worthy step in the development of intracranial atherosclerosis treatment strategies.




Similar content being viewed by others
References
Adelson PD, Scott RM (1995) Pial synangiosis for moyamoya syndrome in children. Pediatr Neurosurg 23(1):26–33
Amin-Hanjani S, Du X, Zhao M, Walsh K, Malisch TW, Charbel FT (2005) Use of quantitative magnetic resonance angiography to stratify stroke risk in symptomatic vertebrobasilar disease. Stroke 36(6):1140
Arenillas J, Molina C, Chacon P, Rovira A, Montaner J, Coscojuela P, Sanchez E, Quintana M, Alvarez-Sabin J (2004) High lipoprotein (a), diabetes, and the extent of symptomatic intracranial atherosclerosis. Neurology 63(1):27
Arenillas JF, Alvarez-Sabin J (2005) Basic mechanisms in intracranial large-artery atherosclerosis: advances and challenges. Cerebrovasc Dis 20(2):75–83
Arenillas JF, Alvarez-Sabin J, Molina CA, Chacon P, Montaner J, Rovira A, Ibarra B, Quintana M (2003) C-reactive protein predicts further ischemic events in first-ever transient ischemic attack or stroke patients with intracranial large-artery occlusive disease. Stroke 34(10):2463
Arenillas JF, Alvarez-Sabin J, Montaner J, Rosell A, Molina CA, Rovira A, Ribo M, Sanchez E, Quintana M (2005) Angiogenesis in symptomatic intracranial atherosclerosis. Stroke 36(1):92–97
Awad I, Furlan AJ, Little JR (1984) Changes in intracranial stenotic lesions after extracranial–intracranial bypass surgery. J Neurosurg 60(4):771–776
Baker A, Flora G, Resch J, Loewenson R (1967) The geographic pathology of atherosclerosis: a review of the literature with some personal observations on cerebral atherosclerosis. Journal of Chronic Diseases 20(9):685–706
Caplan LR, Hennerici M (1998) Impaired clearance of emboli (washout) is an important link between hypoperfusion, embolism, and ischemic stroke. Arch Neurol 55(11):1475
Celletti FL, Waugh JM, Amabile PG, Brendolan A, Hilfiker PR, Dake MD (2001) Vascular endothelial growth factor enhances atherosclerotic plaque progression. Nature medicine 7(4):425–429
Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF et al (2011) Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 365(11):993–1003
Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, Levine SR, Chaturvedi S, Kasner SE, Benesch CG, Sila CA, Jovin TG, Romano JG (2005) Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med 352(13):1305–1316
Chimowitz MI, Lynn MJ, Turan TN, Fiorella D, Lane BF, Janis S et al (2011) Design of the stenting and aggressive medical management for preventing recurrent stroke in intracranial stenosis trial. J Stroke Cerebrovasc Dis 20(4):357–368. doi:10.1016/j.jstrokecerebrovasdis.2011.05.001
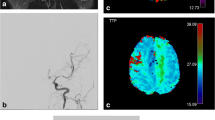
Choi JW, Kim JK, Choi BS, Lim HK, Kim SJ, Kim JS, Suh DC (2010) Angiographic pattern of symptomatic severe M1 stenosis: comparison with presenting symptoms, infarct patterns, perfusion status, and outcome after recanalization. Cerebrovasc Dis 29(3):297–303
Coyle P, Heistad D (1991) Development of collaterals in the cerebral circulation. J Vasc Res 28(1–3):183–189
Derdeyn CP (2007) Mechanisms of ischemic stroke secondary to large artery atherosclerotic disease. Neuroimaging Clinics of North America 17(3):303–311
Dusick J, Gonzalez NR, Martin NA (2011) Clinical and angiographic outcomes from indirect revascularization surgery for Moyamoya disease in adults and children: a review of 63 procedures. Neurosurgery 68(1):34–43, discussion 43
Elmore EM, Mosquera A, Weinberger J (2003) The prevalence of asymptomatic intracranial large vessel occlusive disease: the role of diabetes. J Neuroimaging 13(3):224–227
Famakin BM, Chimowitz MI, Lynn MJ, Stern BJ, George MG (2009) Causes and severity of ischemic stroke in patients with symptomatic intracranial arterial stenosis. Stroke 40(6):1999–2003
Fuster V, Moreno PR, Fayad ZA, Corti R, Badimon JJ (2005) Atherothrombosis and high-risk plaque: part I: evolving concepts. J Am Coll Cardiol 46(6):937–954
Galassi A, Reynolds K, He J (2006) Metabolic syndrome and risk of cardiovascular disease: a meta-analysis. Am J Med 119(10):812–819
Gomez CR, Misra VK, Campbell MS, Soto RD (2000) Elective stenting of symptomatic middle cerebral artery stenosis. Am J Neuroradiol 21(5):971
Gress DR, Smith WS, Dowd CF, Halbach VV, Finley RJ, Higashida RT (2002) Angioplasty for intracranial symptomatic vertebrobasilar ischemia. Neurosurgery 51(1):23
Investigator E-IB (1985) Failure of extracranial–intracranial arterial bypass to reduce the risk of ischemic stroke. Results of an international randomized trial. The EC/IC Bypass Study Group. N Engl J Med 313(19):1191–1200
Kasner SE, Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, Frankel MR, Levine SR, Chaturvedi S, Benesch CG (2006) Predictors of ischemic stroke in the territory of a symptomatic intracranial arterial stenosis. Circulation 113(4):555
Kim DJ, Lee BH, Kim DI, Shim WH, Jeon P, Lee TH (2005) Stent-assisted angioplasty of symptomatic intracranial vertebrobasilar artery stenosis: feasibility and follow-up results. Am J Neuroradiol 26(6):1381
Komotar RJ, Starke RM, Otten ML, Merkow MB, Garrett MC, Marshall RS, Elkind MS, Connolly ES (2009) The role of indirect extracranial–intracranial bypass in the treatment of symptomatic intracranial atheroocclusive disease. J Neurosurg 110(5):896–904
Kono S, Oka K, Sueishi K, Sonobe M (1997) Histopathological studies on spontaneous vault moyamoya and revascularized collaterals formed by encephalomyosynangiosis. Clin Neurol Neurosurg 99:S204–S207
Lee DK, Kim JS, Kwon SU, Yoo SH, Kang DW (2005) Lesion patterns and stroke mechanism in atherosclerotic middle cerebral artery disease: early diffusion-weighted imaging study. Stroke 36(12):2583
Liebeskind DS (2003) Collateral circulation. Stroke 34(9):2279–2284
Liebeskind DS, Cotsonis GA, Saver JL, Lynn MJ, Turan TN, Cloft HJ, Chimowitz MI (2011) Collaterals dramatically alter stroke risk in intracranial atherosclerosis. Ann Neurol 69(6):963–974. doi:10.1002/ana.22354
Malek AM, Alper SL, Izumo S (1999) Hemodynamic shear stress and its role in atherosclerosis. JAMA: the journal of the American Medical Association 282(21):2035
Manoonkitiwongsa PS, Jackson-Friedman C, McMillan PJ, Schultz RL, Lyden PD (2001) Angiogenesis after stroke is correlated with increased numbers of macrophages: the clean-up hypothesis. J Cereb Blood Flow Metab 21(10):1223–1231
Marti H, Risau W (1999) Angiogenesis in ischemic disease. Thrombosis and haemostasis 82:44
Matsushima T, Inoue T, Ikezaki K, Matsukado K, Natori Y, Inamura T, Fukui M (1998) Multiple combined indirect procedure for the surgical treatment of children with moyamoya disease. A comparison with single indirect anastomosis with direct anastomosis. Neurosurg Focus 5(5):6
Meyer JS, Denny-Brown D (1957) The cerebral collateral circulation. I. Factors influencing collateral blood flow. Neurology 7(7):447
Nakamura M, Imai H, Konno K, Kubota C, Seki K, Puentes S, Faried A, Yokoo H, Hata H, Yoshimoto Y (2009) Experimental investigation of encephalomyosynangiosis using gyrencephalic brain of the miniature pig: histopathological evaluation of dynamic reconstruction of vessels for functional anastomosis. Journal of Neurosurgery: Pediatrics 3(6):488–495
Navarro-Sobrino M, Rosell A, Hernández-Guillamon M, Penalba A, Boada C, Domingues-Montanari S, Ribó M, Alvarez-SabÌn J, Montaner J (2011) A large screening of angiogenesis biomarkers and their association with neurological outcome after ischemic stroke. Atherosclerosis 216(1):205–211
Piao R, Oku N, Kitagawa K, Imaizumi M, Matsushita K, Yoshikawa T, Takasawa M, Osaki Y, Kimura Y, Kajimoto K (2004) Cerebral hemodynamics and metabolism in adult moyamoya disease: comparison of angiographic collateral circulation. Ann Nucl Med 18(2):115–121
Qureshi AI, Suri MFK, Ziai WC, Yahia AM, Mohammad Y, Sen S, Agarwal P, Zaidat OO, Suarez JI, Wityk RJ (2003) Stroke-free survival and its determinants in patients with symptomatic vertebrobasilar stenosis: a multicenter study. Neurosurgery 52(5):1033
Reaven GM (1988) Banting lecture 1988. Role of insulin resistance in human disease. Diabetes 37(12):1595
Rosell-Novel A, Montaner J, Alvarez-SabÌn J (2004) Angiogenesis in human cerebral ischemia]. Rev Neurol 38(11):1076
Ross R (1999) Atherosclerosis ‚Äî An Inflammatory Disease. N Engl J Med 340(2):115–126. doi:10.1056/NEJM199901143400207
Sacco RL, Kargman D, Gu Q, Zamanillo M (1995) Race-ethnicity and determinants of intracranial atherosclerotic cerebral infarction: the Northern Manhattan Stroke Study. Stroke 26(1):14–20
Sainte-Rose C, Oliveira R, Puget S, Beni-Adani L, Boddaert N, Thorne J, Wray A, Zerah M, Bourgeois M (2006) Multiple bur hole surgery for the treatment of moyamoya disease in children. Journal of Neurosurgery: Pediatrics 105(6):437–443
Savopoulos C, Michalakis K, Apostolopoulou M, Miras A, Hatzitolios A (2011) Adipokines and stroke: A review of the literature. Maturitas 70(4):322–327
Saz-Saucedo P, Maestre-Moreno JF, Arenillas-Lara JF (2008) Ateromatosis intracraneal. Medicina clÌnica 131(4):141–152
Scanu AM, Lawn RM, Berg K (1991) Lipoprotein(a) and atherosclerosis. Ann Intern Med 115(3):209
Schreiber S, Serdaroglu M, Schreiber F, Skalej M, Heinze HJ, Goertler M (2009) Simultaneous occurrence and interaction of hypoperfusion and embolism in a patient with severe middle cerebral artery stenosis. Stroke 40(7):e478–e480
Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA (2004) Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg 100(2 Suppl Pediatrics):142–149. doi:10.3171/ped.2004.100.2.0142
Starke RM, Komotar RJ, Connolly ES (2009) Optimal surgical treatment for moyamoya disease in adults: direct versus indirect bypass. Neurosurg Focus 26(4):E8. doi:10.3171/2009.01.FOCUS08309
Sundt TM, Smith H, Campbell J, Vlietstra R, Cucchiara R, Stanson A (1980) Transluminal angioplasty for atherosclerosis disease of the vertebral and basilar arteries. Mayo Clin Proc 55:673–680
Takahashi W, Ohnuki T, Ohnuki Y, Kawada S, Takagi S (2008) The role of high-sensitivity C-reactive protein in asymptomatic intra-and extracranial large artery diseases. Cerebrovasc Dis 26(5):549–555
Williams JE, Chimowitz MI, Cotsonis GA, Lynn MJ, Waddy SP (2007) Gender differences in outcomes among patients with symptomatic intracranial arterial stenosis. Stroke 38(7):2055–2062
Wityk R, Lehman D, Klag M, Coresh J, Ahn H, Litt B (1996) Race and sex differences in the distribution of cerebral atherosclerosis. Stroke 27(11):1974
Wong KSL, Chen C, Fu J, Chang HM, Suwanwela NC, Huang YN, Han Z, Tan KS, Ratanakorn D, Chollate P (2010) Clopidogrel plus aspirin versus aspirin alone for reducing embolisation in patients with acute symptomatic cerebral or carotid artery stenosis (CLAIR study): a randomised, open-label, blinded-endpoint trial. Lancet Neurol 9(5):489–497
Yamauchi H, Fukuyama H, Nagahama Y, Nabatame H, Ueno M, Nishizawa S, Konishi J, Shio H (1999) Significance of increased oxygen extraction fraction in five-year prognosis of major cerebral arterial occlusive diseases. J Nucl Med 40(12):1992
Acknowledgments
This study received funding from the American Heart Association Science Innovation Award (NRG) and the Ruth and Raymond Stotter Chair Endowment (NRG).
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Jan-Karl Burkhardt, Zurich, Switzerland
In this review article entitled “Intracranial arterial stenoses: current viewpoints, novel approaches, and surgical perspectives”, Gonzalez et al. provide an overview of intracranial arterial stenosis and report about their experiences with encephaloduroarteriosynangiosis (EDAS) as an indirect revascularization technique. Despite the results of the Carotid Occlusion Surgery Study (COSS), which were not able to show a risk reduction of ischemic stroke in patients with symptomatic atherosclerotic internal carotid artery occlusion and hemodynamic cerebral ischemia after bypass surgery compared to medical therapy alone, surgical revascularization is still indicated in highly selected cases [1, 2]. Besides the optimization of direct revascularization surgery (bypass) to decrease the operative complication rate, which was higher than expected in the COSS study, and to ensure that the entire area of hypoperfused brain tissue has been adequately revascularized, indirect techniques such as EDAS can be useful to improve revascularization (e.g., by increasing collateral formation). However, this technique needs further investigation in patients with symptomatic atherosclerotic internal carotid artery occlusion to assess the benefit as an adjacent to direct revascularization surgery or to medical treatment only.
Refernces
(1) Powers WJ, Clarke WR, Grubb RL Jr, Videen TO, Adams HP Jr, Derdeyn CP; COSS Investigators: Extracranial–intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA 306:1983-92, 2011
(2) Amin-Hanjani S, Barker FG 2nd, Charbel FT, Connolly ES Jr, Morcos JJ, Thompson BG: EC-IC bypass for stroke—is this the end of the line or a bump in the road? Neurosurgery. 2012 71(3):557–561
William W. Ashley and Christopher M. Loftus, Chicago, USA
In the paper entitled “Intracranial arterial stenoses: current viewpoints, novel approaches, and surgical perspectives”, the authors offer a well-written and basic review of intracranial arterial stenosis (IAS). They discuss its etiology as well as the underlying pathophysiology. They pay special attention to the relationship of angiogenesis and collateral circulation to intracranial arterial stenosis and subsequent stroke. Finally, they discuss the current treatment of symptomatic intracranial arterial stenosis in the shadow of the recent publication of the Carotid Occlusion Surgery Study (COSS) [1] and the Stenting and Aggressive Medical Management for Prevention of Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) [2] trial data. They suggest that encephaloduroarteriosynangiosis (EDAS) and other adjunctive indirect revascularization procedures may offer a safe and effective alternative to direct and endovascular techniques.
Gonzalez et al. did an excellent job of providing an overview of IAS. They correctly indicate the multifactorial nature of the process. They also highlight the importance of hemodynamic factors in the development of the disease. Unfortunately, we still do not have a reliable way to predict which patients will ultimately go on to become symptomatic. Indeed, it may be that they are many subsets of patients with important, but yet unknown hemodynamic, genetic, or other factors that predispose them to certain disease phenotypes. There has been some promising work on biomarkers related to IAS and ischemia, but our understanding of the cell and molecular biology that leads to symptomatic IAS is still in its infancy. However, our ability to study flow and hemodynamic alteration is advancing rapidly and, in our opinion, offers an excellent opportunity to study and understand IAS. Moreover, careful case-by-case hemodynamic analysis is our best hope to correctly select patients for revascularization procedures.
That being said, there is still a great deal that we do not know, and more than anything else, this submission asks us to continue searching for a way to help IAS patients. We agree with the underlying premise that symptomatic IAS is a serious problem and medical therapy alone has unacceptably high rates of recurrent stroke and associated morbidity and mortality. Therefore, alternatives to medical therapy alone must be defined. The review suggests that EDAS may be useful for the treatment of IAS based on a small retrospective pilot study by most of the same authors [3]. In this study, 13 patients underwent unilateral EDAS plus or minus burr holes for symptomatic unilateral stenosis. There were no serious complications, 10 out of 13 total patients had angiographic evidence of increased vascularity and/or direct anastomosis after EDAS, there were no strokes in the follow-up period, and all but two had durable resolution of symptoms by 3 months. These are encouraging results and are on par with data from some other groups who have used EDAS for the treatment of intracranial steno-occlusive disease that is not classically defined as moyamoya disease [4, 5] and better than that seen when used for complete intracranial arterial occlusion [5].
This calls into question our implicit assumptions about IAS itself. Intracranial steno-occlusive disease is difficult to divide into clean boxes. As mentioned, it is multifactorial and usually overlapping. Moyamoya disease is classically defined as bilateral, progressive, idiopathic steno-occlusive disease affecting basal intracranial arteries. Moyamoya phenomenon has a much broader definition and can include unilateral findings and finding that are associated with other pathologies including atherosclerotic disease [4, 6]. Indeed as the authors themselves point out, “in only three patients could a definitive etiology of intracranial atherosclerosis be determined” [3]. It is possible that the patients mentioned in the study by Dusick et al. did have a phenotype of moyamoya. Indeed, Hallemeier et al. suggest that moyamoya phenomenon in North American adults is quite different from the classic Asian phenotype, is often unilateral, and can present like many of the patients in the pilot study by Dusick et al. Therefore, we still may not really know whether EDAS is really useful for atherosclerotic disease. But it is still very exciting to think that a procedure like EDAS may hold some promise. In order to further delineate the underlying pathologic process and better inform possible treatments, it may be beneficial to utilize advanced imaging techniques such as direct evaluation of the blood vessel wall using high field strength MRI [7] in addition to perfusion studies, PET, or quantitative MRI.
This is a timely submission that in light of the “disappointing results” of the recent COSS and SAMMPRISS data, forces us to think carefully about intracranial steno-occlusive disease and how we decide who will benefit from the treatment. Based on the SAMMPRIS and COSS data, some could take the pessimistic and, in our opinion, premature view, that direct surgical and endovascular cerebral revascularization should not be offered as treatment for symptomatic intracranial atherosclerosis disease. SAMMPRIS and COSS were both well done studies that required a great deal of hard work by a great many. But the data must be interpreted with the underlying assumptions in mind. Multiple groups have opined on the meaning of both studies and cited many valid reasons why they are not definitive [8–10]. One concept that most will agree upon is that medical therapy is more efficacious than expected and we as practitioners have a much higher procedural standard to uphold if we hope to see any benefit from intervention for this difficult disease. Thus, instead of wholesale abandonment of direct bypass and stenting, we must re-evaluate and refine our patient selection techniques and improve our procedural outcomes. So we applaud the author’s efforts to offer an alternative efficacious means of bypass that potentially addresses some of the pathophysiologic downfalls of direct bypass and stenting, while at the same time having a more favorable complication profile. We agree that further study must be done to elucidate whether EDAS can actually be useful for patients with symptomatic intracranial atherosclerotic stenosis. This will require careful consideration of clinical, hemodynamic, and imaging characteristics in order to select the right patients. We along with others in the cerebrovascular community look forward to the challenge. We are hopeful that EDAS along with other tools including direct bypass and intracranial stenting will offer some hope for the unfortunate group of patients with IAS that fail modern medical therapy.
References
1. Powers, W.J., et al., Extracranial–intracranial bypass surgery for stroke prevention in hemodynamic cerebral ischemia: the Carotid Occlusion Surgery Study randomized trial. JAMA, 2011. 306(18): p. 1983-92.
2. Chimowitz, M.I., et al., Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med, 2011. 365(11): p. 993-1003.
3. Dusick, J.R., Liebeskind, D.S., Saver, J.L, Martin, N.A, Gonzalez, N.R. Unpublished data.
4. Hallemeier, C.L., et al., Clinical features and outcome in North American adults with moyamoya phenomenon. Stroke, 2006. 37(6): p. 1490-6.
5. Komotar, R.J., et al., The role of indirect extracranial–intracranial bypass in the treatment of symptomatic intracranial atheroocclusive disease. J Neurosurg, 2009. 110(5): p. 896-904.
6. Goyal, M.S., et al., Clinical features and outcome in North American adults with idiopathic basal arterial occlusive disease without moyamoya collaterals. Neurosurgery, 2010. 67(2): p. 278-85.
7. Ashley, W.W., Jr., et al., Moyamoya phenomenon secondary to intracranial atherosclerotic disease: diagnosis by 3 T magnetic resonance imaging. J Neuroimaging, 2009. 19(4): p. 381-4.
8. Amin-Hanjani, S., et al., Extracranial–intracranial bypass for stroke—is this the end of the line or a bump in the road? Neurosurgery, 2012. 71(3): p. 557-561.
9. Qureshi, A.I., Interpretation and implications of the prematurely terminated Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in the Intracranial Stenosis (SAMMPRIS) trial. Neurosurgery, 2012. 70(1): p. E264-8.
10. Wong, G.K. and W.S. Poon, Time to reflect on surgery and neuro-intervention for intracranial atherosclerotic diseases. J Clin Neurosci, 2012. 19(2): p. 222-3.
Rights and permissions
About this article
Cite this article
Gonzalez, N.R., Liebeskind, D.S., Dusick, J.R. et al. Intracranial arterial stenoses: current viewpoints, novel approaches, and surgical perspectives. Neurosurg Rev 36, 175–185 (2013). https://doi.org/10.1007/s10143-012-0432-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0432-z