Abstract
Purpose
Whether alendronate treatment has a residual effect on bone ingrowth into porous biomaterial in humans or experimental animals after treatment withdrawal is still unknown. The purpose of this study was to investigate bone ingrowth into porous tantalum and carbon fiber interbody implants after discontinuing alendronate treatment in experimental spinal fusion in pigs.
Methods
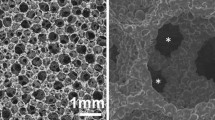
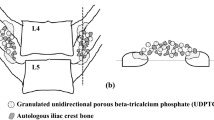
Twenty-four pigs were randomly divided into two groups of each 12 pigs. The pigs underwent anterior intervertebral lumbar arthrodeses at L2–3, L4–5 and L6–7. Each level was randomly allocated to one of the three implants: a porous tantalum ring with pedicle screw fixation, a porous tantalum ring or a carbon fiber cage with anterior staple fixation. The central hole of implants was packed with an autograft. Alendronate was given orally for the first 3 months to one of the two groups. The pigs were observed for 6 months postoperatively. Histology and micro-CT scans were done at the endpoint.
Results
The spinal fusion rates of each implant showed no differences between two treatment groups. Furthermore, no differences were found between two groups as for bone ingrowth into the central holes of implants and bone–implant interface in each implant, or as for the pores of tantalum implants. Trabecular bone microarchitecture in the central hole of the carbon fiber cage did not differ between two treatment groups.
Conclusion
The application of ALN, with a dose equivalent to that given to humans during the first 3 months after surgery, does not maintain a residual effect on spinal fusion with porous tantalum ring and autograft after treatment withdrawal in a porcine ALIF model.





Similar content being viewed by others
References
Liberman UA, Weiss SR, Broll J et al (1995) Effect of oral alendronate on bone mineral density and the incidence of fractures in postmenopausal osteoporosis. The Alendronate phase III osteoporosis treatment study group. N Engl J Med 333:1437–1443
Zou X, Xue Q, Li H et al (2003) Effect of alendronate on bone ingrowth into porous tantalum and carbon fiber interbody devices: an experimental study on spinal fusion in pigs. Acta Orthop Scand 74:596–603
Nakao SI, Minamide A, Kawakami M et al (2011) The influence of alendronate on spine fusion in an osteoporotic animal model. Spine (Phila Pa 1976) 36:1446–1452
Huang RC, Khan SN, Sandhu HS et al (2005) Alendronate inhibits spine fusion in a rat model. Spine (Phila Pa 1976) 30:2516–2522
Lehman RA Jr, Kuklo TR, Freedman BA et al (2004) The effect of alendronate sodium on spinal fusion: a rabbit model. Spine J 4:36–43
Sama AA, Khan SN, Myers ER et al (2004) High-dose alendronate uncouples osteoclast and osteoblast function: a study in a rat spine pseudarthrosis model. Clin Orthop Relat Res 425:135–142
Peter CP, Cook WO, Nunamaker DM et al (1996) Effect of alendronate on fracture healing and bone remodeling in dogs. J Orthop Res 14:74–79
Lenart BA, Lorich DG, Lane JM (2008) Atypical fractures of the femoral diaphysis in postmenopausal women taking alendronate. N Engl J Med 358:1304–1306
Lin JH, Russell G, Gertz B (1999) Pharmacokinetics of alendronate: an overview. Int J Clin Pract Suppl 101:18–26
Bagger YZ, Tanko LB, Alexandersen P et al (2003) Alendronate has a residual effect on bone mass in postmenopausal Danish women up to 7 years after treatment withdrawal. Bone 33:301–307
Bobyn JD, Stackpool GJ, Hacking SA et al (1999) Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br 81:907–914
Bobyn JD, Toh KK, Hacking SA et al (1999) Tissue response to porous tantalum acetabular cups: a canine model. J Arthroplasty 14:347–354
Zou X, Li H, Bünger M et al (2004) Bone ingrowth characteristics of porous tantalum and carbon fiber interbody devices: an experimental study in pigs. Spine J 4:99–105
Bünger MH, Foss M, Erlacher K et al (2006) Bone nanostructure near titanium and porous tantalum implants studied by scanning small angle X-ray scattering. Eur Cell Mater 12:81–91
Xue Q, Li H, Zou X et al (2010) Alendronate treatment improves bone-pedicle screw interface fixation in posterior lateral spine fusion: an experimental study in a porcine model. Int Orthop 34:447–451
Ding M, Odgaard A, Hvid I (1999) Accuracy of cancellous bone volume fraction measured by micro-CT scanning. J Biomech 32:323–326
Nagahama K, Kanayama M, Togawa D et al (2011) Does alendronate disturb the healing process of posterior lumbar interbody fusion? A prospective randomized trial. J Neurosurg Spine 14:500–507
Duarte PM, de Vasconcelos Gurgel BC, Sallum AW et al (2005) Alendronate therapy may be effective in the prevention of bone loss around titanium implants inserted in estrogen-deficient rats. J Periodontol 76:107–114
Nishitani K, Shirai T, Kobayashi M et al (2009) Positive effect of alendronate on subchondral bone healing and subsequent cartilage repair in a rabbit osteochondral defect model. Am J Sports Med 37:139S–147S
Lund T, Oxland TR, Jost B et al (1998) Interbody cage stabilisation in the lumbar spine: biomechanical evaluation of cage design, posterior instrumentation and bone density. J Bone Joint Surg Br 80:351–359
Sagomonyants KB, Hakim-Zargar M, Jhaveri A et al (2011) Porous tantalum stimulates the proliferation and osteogenesis of osteoblasts from elderly female patients. J Orthop Res 29(4):609–616
Schenk RK, Felix R, Hofstetter W (1993) Morphology of connective tissue: bone. In Royce, PM, Steinmann B (eds) Connective Tissue and Its Heritable Disorders. Molecular, genetic, and medical aspects, Wiley-Liss, New York, pp 85–101
Acknowledgments
The authors thank Anette Milton for technical assistance in histology, Bruce Robie, PhD, for excellent help in revising of the manuscript, and the Danish Institute of Agricultural Sciences, Research Center Foulum, for excellent cooperation. The Danish Rheumatism Association, the Institute of Experimental Clinical Research, University of Aarhus, and the Aarhus Spine Research Foundation in Denmark provided financial supports. This work was also supported by the Danish Council for Strategic Research project IMR: “Individualized musculoskeletal regeneration and reconstruction” (2101-07-0120), 973 Program (No. 2012CB619100), the NSFC (No. u0732001), and the S&T project of Guangdong Province (2010B010800019). Hedrocel ALIF devices (Porous Tantalum Implants) was kindly supplied by Implex Corp., Allendale, NJ, USA, for the study. The experiments complied with the Danish Law on Animal Experiments and were approved by the Danish Ministry of Justice, J. No. 1998-561-67.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, B., Zou, X., Li, H. et al. Short-term alendronate treatment does not maintain a residual effect on spinal fusion with interbody devices and bone graft after treatment withdrawal: an experimental study on spinal fusion in pigs. Eur Spine J 22, 287–295 (2013). https://doi.org/10.1007/s00586-012-2513-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2513-7