Abstract
Purpose
The heparin dose–response (HDR) technique is based on activated clotting time (ACT) response to a fixed-dose heparin bolus, which varies substantially among patients. It is unclear, however, whether hemodilution-associated reductions in coagulation and anticoagulation factors affect the HDR slope.
Methods
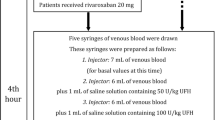
For in vitro hemodilution, aliquots of whole blood from healthy volunteers were diluted 9:1 and 8:2 v/v with normal saline. For in vivo hemodilution, a prospective observational study was performed on 46 patients who underwent elective cardiovascular surgery with or without cardiopulmonary bypass. HDR slope, antithrombin (AT) activity, complete blood count, and other coagulation parameters were compared after induction of anesthesia and after hemodilution with 500 ml of intravenous fluid.
Results
In vitro 10 and 20 % hemodilution significantly increased the HDR slope relative to baseline, reducing the heparin requirement. Hemodilution of heparinized samples significantly prolonged ACT, whereas there was no significant change in non-heparinized blood. The percent changes in fibrinogen and AT activity were significantly greater at 20 % than those of the other coagulation variables. In vivo, hemodilution significantly increased the HDR slope and reduced heparin requirement. The percent change in fibrinogen due to hemodilution was significantly greater than the change in AT activity. Target ACTs of 300 and 450 s were not achieved in 83.3 and 53.8 % of patients, respectively.
Conclusion
In vitro and in vivo hemodilution significantly increased the HDR slope and reduced the requirement for heparin. In vitro, the HDR slope did not change in parallel but became steeper, depending on the degree of hemodilution.

Similar content being viewed by others
References
Hattersley PG. Activated coagulation time of whole blood. JAMA. 1966;196:436–40.
Bull BS, Huse WM, Brauer FS, Korpman RA. Heparin therapy during extracorporeal circulation. II. The use of a dose-response curve to individualize heparin and protamine dosage. J Thorac Cardiovasc Surg. 1975;69:685–9.
Akl BF, Vargas GM, Neal J, Robillard J, Kelly P. Clinical experience with the activated clotting time for the control of heparin and protamine therapy during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1980;79:97–102.
Raymond PD, Ray MJ, Callen SN, Marsh NA. Heparin monitoring during cardiac surgery. Part 1: Validation of whole-blood heparin concentration and activated clotting time. Perfusion. 2003;18:269–76.
Despotis GJ, Joist JH, Hogue CW Jr, Alsoufiev A, Kater K, Goodnough LT, Santoro SA, Spitznagel E, Rosenblum M, Lappas DG. The impact of heparin concentration and activated clotting time monitoring on blood conservation. A prospective, randomized evaluation in patients undergoing cardiac operation. J Thorac Cardiovasc Surg. 1995;110:46–54.
Jobes DR, Aitken GL, Shaffer GW. Increased accuracy and precision of heparin and protamine dosing reduces blood loss and transfusion in patients undergoing primary cardiac operations. J Thorac Cardiovasc Surg. 1995;110:36–45.
Culliford AT, Gitel SN, Starr N, Thomas ST, Baumann FG, Wessler S, Spencer FC. Lack of correlation between activated clotting time and plasma heparin during cardiopulmonary bypass. Ann Surg. 1981;193:105–11.
Huyzen RJ, Harder MP, Huet RC, Boonstra PW, Brenken U, van Oeveren W. Alternative perioperative anticoagulation monitoring during cardiopulmonary bypass in aprotinin-treated patients. J Cardiothorac Vasc Anesth. 1994;8:153–6.
Cohen EJ, Camerlengo LJ, Dearing JP. Activated clotting times and cardiopulmonary bypass I: the effect of hemodilution and hypothermia upon activated clotting time. J Extracorporeal Technol. 1980;12:139–41.
Murano G, Williams L, Miller-Andersson M, Aronson DL, King C. Some properties of antithrombin-III and its concentration in human plasma. Thromb Res. 1980;18:259–62.
Srivastava AR, Banerjee A, Misra BB, Minhas H, Virmani S. Does hemodilution by the crystalloid priming solution derange the efficacy of anticoagulation during cardiopulmonary bypass? J Card Surg. 2008;23:239–45.
Ng KF, Lo JW. The development of hypercoagulability state, as measured by thrombelastography, associated with intraoperative surgical blood loss. Anaesth Intensive Care. 1996;24:20–5.
Ruttmann TG, James MF, Viljoen JF. Haemodilution induces a hypercoagulable state. Br J Anaesth. 1996;76:412–4.
Jamnicki M, Zollinger A, Seifert B, Popovic D, Pasch T, Spahn DR. The effect of potato starch derived and corn starch derived hydroxyethyl starch on in vitro blood coagulation. Anesthesiology. 1998;53:638–44.
Huyzen RJ, van Oeveren W, Wei F, Stellingwerf P, Boonstra PW, Gu YJ. In vitro effect of hemodilution on activated clotting time and high-dose thrombin time during cardiopulmonary bypass. Ann Thorac Surg. 1996;62:533–7.
Dietrich W, Spannagl M, Schramm W, Vogt W, Barankay A, Richter JA. The influence of preoperative anticoagulation on heparin response during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1991;102:505–14.
Dalbert S, Ganter MT, Furrer L, Klaghofer R, Zollinger A, Hofer CK. Effects of heparin, haemodilution and aprotinin on kaolin-based activated clotting time: in vitro comparison of two different point of care devices. Acta Anaesthesiol Scand. 2006;50:461–8.
Monkhouse FC. Relationship between antithrombin and thrombin levels in plasma and serum. Am J Physiol. 1959;197:984–8.
Darlington DN, Delgado AV, Kheirabadi BS, Fedyk CG, Scherer MR, Pusateri AE, Wade CE, Cap AP, Holcomb JB, Dubick MA. Effect of hemodilution on coagulation and recombinant factor VIIa efficacy in human blood in vitro. J Trauma. 2011;71:1152–63.
Ruttmann TG, James MF, Aronson I. In vivo investigation into the effects of haemodilution with hydroxyethyl starch (200/0.5) and normal saline on coagulation. Br J Anaesth. 1998;80:612–6.
Jesty J, Beltrami E, Willems G. Mathematical analysis of a proteolytic positive-feedback loop: dependence of lag time and enzyme yields on the initial conditions and kinetic parameters. Biochemistry. 1993;32:6266–74.
Linden MD, Gibbs NM, Bremner M, Schneider M, Erber WN. The effect of haemodilution on antithrombin concentration during cardiac surgery. Anaesth Intensive Care. 2004;32:219–23.
Olson ST, Bjork I, Sheffer R, Craig PA, Shore JD, Choay J. Role of the antithrombin-binding pentasaccharide in heparin acceleration of antithrombin-proteinase reactions. Resolution of the antithrombin conformational change contribution to heparin rate enhancement. J Biol Chem. 1992;267:12528–38.
Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, Granger C, Ohman EM, Dalen JE. Heparin and low-molecular-weight heparin: mechanisms of action, pharmacokinetics, dosing, monitoring, efficacy, and safety. Chest. 2001;119:64S–94S.
Freedman MD. Pharmacodynamics, clinical indications, and adverse effects of heparin. J Clin Pharmacol. 1992;32:584–96.
Tollefsen DM, Majerus DW, Blank MK. Heparin cofactor II. Purification and properties of a heparin-dependent inhibitor of thrombin in human plasma. J Biol Chem. 1982;257:2162–9.
Vicente CP, He L, Pavão MS, Tollefsen DM. Antithrombotic activity of dermatan sulfate in heparin cofactor II-deficient mice. Blood. 2004;104:3965–70.
Maaroufi RM, Jozefowicz M, Tapon-Bretaudière J, Fischer AM. Mechanism of thrombin inhibition by antithrombin and heparin cofactor II in the presence of heparin. Biomaterials. 1997;18:203–11.
Abildgaard U. Heparin/low molecular weight heparin and tissue factor pathway inhibitor. Haemostasis. 1993;23(Suppl 1):103–6.
Koster A, Fischer T, Praus M, Haberzettl H, Kuebler WM, Hetzer R, Kuppe H. Hemostatic activation and inflammatory response during cardiopulmonary bypass: impact of heparin management. Anesthesiology. 2002;97:837–41.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Ichikawa, J., Hagihira, S., Mori, T. et al. In vitro and in vivo effects of hemodilution on kaolin-based activated clotting time predicted heparin requirement using a heparin dose–response technique . J Anesth 30, 923–928 (2016). https://doi.org/10.1007/s00540-016-2227-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00540-016-2227-9