Abstract
Background
Although incidental hernias frequently are found and repaired during laparoscopic cholecystectomy (LC), the outcomes of simultaneous LC and laparoscopic ventral hernia repair (LVHR) have not been scrutinized. In this study we evaluated short-term outcome data comparing simultaneous LC and LVHR against LC alone.
Methods
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) database (2005–2009) was queried using primary procedure and secondary current procedural terminology (CPT®) codes for LC and LVHR. Outcomes analyzed included separate LC and LVHR and simultaneous laparoscopic cholecystectomy and ventral hernia repair (LC/LVHR). The 30 day clinical outcomes along with postoperative hospital length of stay (LOS) were assessed using the χ2 test and analysis-of-variance test with p values < 0.01 set as significant. We also performed forward stepwise multivariable regression taking in to consideration over 50 ACS NSQIP risk factors to adjust for patient risk.
Results
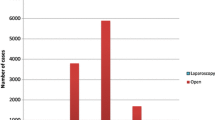
A total of 82,837 patients underwent LC and/or LVHR of which 357 (0.4 %) underwent simultaneous LC/LVHR. Patients who underwent LC/LVHR were more likely to have surgical site infections, suffer sepsis or septic shock, and have pulmonary complications, including pneumonia, reintubation or prolonged ventilator requirements, than LC-alone patients. No difference was noted in 30 day mortality, rates of deep vein thrombosis/pulmonary embolism (DVT/PE), renal insufficiency, or stroke. After multivariable adjustment for over 50 ACS NSQIP risk factors, concurrent LC/LVHR continued to pose a higher risk for these outcomes relative to LC only.
Conclusions
Simultaneous LC/LVHR results in greater postoperative morbidity in terms of surgical site infections, sepsis, and pulmonary complications when compared to LC alone. In light of this increased short-term morbidity, consideration should be given toward performing LC and LVHR independently in patients requiring both procedures. Prospective studies with long-term follow-up are required to better understand the implications of simultaneous LC/LVHR.
Similar content being viewed by others
References
Jani K, Rajan PS, Sendhilkumar K, Palanivelu C (2006) Twenty years after Erich Muhe: persisting controversies with the gold standard of laparoscopic cholecystectomy. J Minim Access Surg 2:49–58
Ingraham AM, Cohen ME, Ko CY, Hall B (2010) A current profile and assessment of North American cholecystectomy: results from the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 211:176–186
Yamagishi S, Watanabe T (2000) Concomitant laparoscopic splenectomy and cholecystectomy for management of hereditary spherocytosis associated with gallstones. J Clin Gastroenterol 30:447
Wang Q, Deng S, Li E (1997) Combined laparoscopic surgery. Zhonghua Wai Ke Za Zhi 35:84–88
Warren JL, Penberthy LT, Addiss DG, McBean AM (1993) Appendectomy incidental to cholecystectomy among elderly Medicare beneficiaries. Surg Gynecol Obstet 177:288–294
Ghidirim GHP, Gladun EV, Danch AV, Mishina E (1996) Combined laparoscopic treatment of polycystic ovary disease and gallstones. J Am Assoc Gynecol Laparosc 3(4 Suppl):S15
Patton ML, Moss BE, Haith LR Jr, Shotwell BA, Milliner DH, Simeone MR, Kraut JD, Patton JN (1997) Concomitant laparoscopic cholecystectomy and splenectomy for surgical management of hereditary spherocytosis. Am Surg 63:536–539
Suh SW, Park JM, Lee SE, Choi YS (2012) Accidental gallbladder perforation during laparoscopic cholecystectomy: does it have an effect on the clinical outcomes? J Laparoendosc Adv Surg Tech A 22:40–45
Barrat C, Champault A, Matthyssens L, Champault G (2004) Iatrogenic perforation of the gallbladder during laparoscopic cholecystectomy does not influence the prognosis. Prospective study. Ann Chir 129:25–29
Rice DC, Memon MA, Jamison RL, Agnessi T, Ilstrup D, Bannon MB, Farnell MB, Grant CS, Sarr MG, Thompson GB, van Heerden JA, Zietlow SP, Donohue JH (1997) Long-term consequences of intraoperative spillage of bile and gallstones during laparoscopic cholecystectomy. J Gastrointest Surg 1:85–90; discussion 90–91
Assaff Y, Matter I, Sabo E, Mogilner JG, Nash E, Abrahamson J, Eldar S (1998) Laparoscopic cholecystectomy for acute cholecystitis and the consequences of gallbladder perforation, bile spillage, and “loss” of stones. Eur J Surg 164:425–431
Hart D, Postlethwait RW, Brown IW Jr, Smith WW, Johnson PA (1968) Postoperative wound infections: a further report on ultraviolet irradiation with comments on the recent (1964) National Research Council Cooperative Study Report. Ann Surg 167:728–743
Culver DH, Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG, Banerjee SN, Edwards JR et al (1991) Surgical wound infection rates by wound class, operative procedure, and patient risk index. National Nosocomial Infections Surveillance System. Am J Med 91:152S–157S
Cruse PJ, Foord R (1980) The epidemiology of wound infection. A 10-year prospective study of 62,939 wounds. Surg Clin North Am 60:27–40
Choi JJ, Palaniappa NC, Dallas KB, Rudich TB, Colon MJ, Divino CM (2012) Use of mesh during ventral hernia repair in clean-contaminated and contaminated cases: outcomes of 33,832 cases. Ann Surg 255:176–180
Savita K, Khedkar I, Bhartia VK (2010) Combined procedures with laparoscopic cholecystectomy. Indian J Surg 72:377–380
Wadhwa A, Chowbey PK, Sharma A, Khullar R, Soni V, Baijal M (2003) Combined procedures in laparoscopic surgery. Surg Laparosc Endosc Percutan Tech 13:382–386
Sauerland S, Korenkov M, Kleinen T, Arndt M, Paul A (2004) Obesity is a risk factor for recurrence after incisional hernia repair. Hernia 8:42–46
Anthony T, Bergen PC, Kim LT, Henderson M, Fahey T, Rege RV, Turnage RH (2000) Factors affecting recurrence following incisional herniorrhaphy. World J Surg 24:95–100; discussion 101
Bordon A, Bokhari R, Sperry J, Testa D 4th, Feinstein A, Ghaemmaghami V (2011) Swallowing dysfunction after prolonged intubation: analysis of risk factors in trauma patients. Am J Surg 202:679–682; discussion 682–683
Nesek-Adam V, Mrsić V, Oberhofer D, Grizelj-Stojcić E, Kosuta D, Rasić Z (2010) Post-intubation long-segment tracheal stenosis of the posterior wall: a case report and review of the literature. J Anesth 24:621–625
Penuelas O, Frutos-Vivar F, Fernández C, Anzueto A, Epstein SK, Apezteguía C, González M, Nin N, Raymondos K, Tomicic V, Desmery P, Arabi Y, Pelosi P, Kuiper M, Jibaja M, Matamis D, Ferguson ND, Esteban A, Ventila Group (2011) Characteristics and outcomes of ventilated patients according to time to liberation from mechanical ventilation. Am J Respir Crit Care Med 184:430–437
Acknowledgment
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Disclosure
Dr. J. Scott Roth is a consultant for C.R. Bard, Inc. Drs. Orr and Davenport have no conflicts of interest or financial ties to disclose.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
See Table 4
Rights and permissions
About this article
Cite this article
Orr, N.T., Davenport, D.L. & Roth, J.S. Outcomes of simultaneous laparoscopic cholecystectomy and ventral hernia repair compared to that of laparoscopic cholecystectomy alone. Surg Endosc 27, 67–73 (2013). https://doi.org/10.1007/s00464-012-2408-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-012-2408-z