Abstract
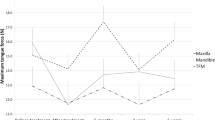
In oral cancer treatment, function loss such as speech and swallowing deterioration can be severe, mostly due to reduced lingual mobility. Until now, there is no standardized measurement tool for tongue mobility and pre-operative prediction of function loss is based on expert opinion instead of evidence based insight. The purpose of this study was to assess the reliability of a triple-camera setup for the measurement of tongue range of motion (ROM) in healthy adults and its feasibility in patients with partial glossectomy. A triple-camera setup was used, and 3D coordinates of the tongue in five standardized tongue positions were achieved in 15 healthy volunteers. Maximum distances between the tip of the tongue and the maxillary midline were calculated. Each participant was recorded twice, and each movie was analysed three times by two separate raters. Intrarater, interrater and test–retest reliability were the main outcome measures. Secondly, feasibility of the method was tested in ten patients treated for oral tongue carcinoma. Intrarater, interrater and test–retest reliability all showed high correlation coefficients of >0.9 in both study groups. All healthy subjects showed perfect symmetrical tongue ROM. In patients, significant differences in lateral tongue movements were found, due to restricted tongue mobility after surgery. This triple-camera setup is a reliable measurement tool to assess three-dimensional information of tongue ROM. It constitutes an accurate tool for objective grading of reduced tongue mobility after partial glossectomy.


Similar content being viewed by others
References
Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancer. Oral Oncol. 2008;45:309–16.
www.cijfersoverkanker.nl. Accessed 12 July 2014.
Sessions DG, Spector GJ, Lenox J, Haughey B, Chao C, Marks J. Analysis of treatment results for oral tongue cancer. Laryngoscope. 2002;112:616–25.
Konstantinović V, Dimić N. Articulatory function and tongue mobility after surgery followed by radiotherapy for tongue and floor of the mouth cancer patients. Br J Plast Surg. 1998;51:589–93.
Bressmann T, Sader R, Whitehill TL, Samman N. Consonant intelligibility and tongue motility in patients with partial glossectomy. J Oral Maxillofac Surg. 2004;62:298–303.
Matsui Y, Ohno K, Yamashita Y, Takahashi K. Factors influencing postoperative speech function of tongue cancer patients following reconstruction with fasciocutaneous/myocutaneous flaps–a multicenter study. Int J Oral Maxillofac Surg. 2007;36:601–9.
Lazarus CL, Husaini H, Jacobson AS, Mojica JK, Buchbinder D, Okay D, et al. Development of a new lingual range-of-motion assessment scale: normative data in surgically treated oral cancer patients. Dysphagia. 2014;29:489–99.
Husaini H, Krisciunas GP, Langmore S, Mojica JK, Urken ML, Jacobson AS, et al. A survey of variables used by speech-language pathologists to assess function and predict functional recovery in oral cancer patients. Dysphagia. 2014;29:376–86.
Kreeft MA, Tan IB, Leemans CR, Balm JMA. The surgical dilemma in advanced oral and oropharyngeal cancer: how we do it. Clin Otolaryngol. 2011;36:260–6.
Kreeft AM, Rasch CRN, Muller SH, Pameijer FA, Hallo E, Balm AJM. Cine MRI of swallowing in patients with advanced oral or oropharyngeal carcinoma: a feasibility study. Eur Arch Otorhinolaryngol. 2012;269:1703–11.
Rastadmehr O, Bressmann T, Smyth R, Irish JC. Increased midsagittal tongue velocity as indication of articulatory compensation in patients with lateral partial glossectomies. Head Neck. 2008;30:718–27.
Lazarus CL, Logemann JA, Rademaker AW, Lurie TRH, Larson CR, Mittal BB. Swallowing and tongue function and oropharyngeal cancer. J Speech Lang Hear Res. 2000;43:1011–24.
www.oncoline.nl/mondholte-en-orofarynxcarcinoom. Accessed 17 July 2014.
Youmans SR, Youmans GL, Stierwalt JAG. Differences in tongue strength across age and gender: is there a diminished strength reserve? Dysphagia. 2009;24:57–65.
Van der Molen L, van Rossum MA, Ackerstaff AH, Smeele LE, Rasch CRN, Hilgers FJM. Pretreatment organ function in patients with advanced head and neck cancer: clinical outcome measures and patients’ views. BMC Ear Nose Throat Disord. 2009;9:10.
Chepeha DB, Teknos TN, Shargorodsky J, Sacco AG, Lyden T, Prince ME, et al. Rectangle tongue template for reconstruction of the hemiglossectomy defect. Arch Otolaryngol Head Neck Surg. 2008;134:993–8.
Van Alphen MJA, Eskes M, LE Smeele, van der Heijden F. In vivo intraoperative hypoglossal nerve stimulation for quantitative tongue motion analysis. Comput Methods Biomech Biomed Eng imaging Vis. 2015;. doi:10.1080/21681163.2015.1072056.
Acknowledgments
This research project was supported by private funding from Mr D. van den Brink and Mrs A. van den Brink. The 3D camera setup was funded by the Maurits and Anna de Kock Foundation. The authors thank Lisette van der Molen for her contribution in completion of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
van Dijk, S., van Alphen, M.J.A., Jacobi, I. et al. A New Accurate 3D Measurement Tool to Assess the Range of Motion of the Tongue in Oral Cancer Patients: A Standardized Model. Dysphagia 31, 97–103 (2016). https://doi.org/10.1007/s00455-015-9665-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-015-9665-7