Abstract
Purpose
Meningiomas in children are rare, especially those located at the skull base. In this study, we report our experience of meningioma surgery in the pediatric population and compare our findings of skull base (SB) versus non-skull base (NSB) meningiomas.
Methods
From our database of 724 surgically treated meningioma patients at the University Hospital, Zurich between 1995 and 2010, 12 patients under 18 years of age were identified. Data for those patients was retrospectively collected through chart review. A descriptive comparison between SB and NSB meningiomas was undertaken to determine statistical significance.
Results
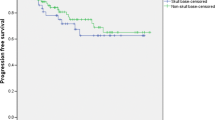
In all 12 children (seven males, five females; mean age 12.2 ± 4.3 years), surgical removal of the meningioma was performed microsurgically with a mean follow-up of 53 months (range 12–137 months). Of the 12 tumors, six were located in the SB and six in the NSB. Comparing SB to NSB lesions, the mean age was 11 ± 3.8 versus 14 ± 4.6 years, male/female gender distribution was 5:1 compared to 1:5, mean tumor size was 7.5 ± 6.2 versus 26 ± 15.8 cm2 (p = 0.03), and mean surgery time was 347 versus 214 min. While WHO grade was similar for both groups, the Simpson grade revealed more extensive resection for NSB meningiomas. The Glasgow Outcome Scale at last follow-up was favorable for both groups.
Conclusions
Meningioma surgery was safe with favorable outcomes. SB meningiomas were significantly smaller in size, were less likely to undergo complete resection, and had a predilection for younger, male patients.

Similar content being viewed by others
References
Burkhardt JK, Zinn PO, Graenicher M, Santillan A, Bozinov O, Kasper EM, Krayenbuhl N (2011) Predicting postoperative hydrocephalus in 227 patients with skull base meningioma. Neurosurg Focus 30:E9
Chen CM, Huang AP, Kuo LT, Tu YK (2011) Contemporary surgical outcome for skull base meningiomas. Neurosurg Rev 34:281–296, discussion 296
Erdincler P, Lena G, Sarioglu AC, Kuday C, Choux M (1998) Intracranial meningiomas in children: review of 29 cases. Surg Neurol 49:136–140, discussion 131–140
Gao X, Zhang R, Mao Y, Wang Y (2009) Childhood and juvenile meningiomas. Childs Nerv Syst 25:1571–1580
Kotecha RS, Junckerstorff RC, Lee S, Cole CH, Gottardo NG (2011) Pediatric meningioma: current approaches and future direction. J Neurooncol 104:1–10
Kotecha RS, Pascoe EM, Rushing EJ, Rorke-Adams LB, Zwerdling T, Gao X, Li X, Greene S, Amirjamshidi A, Kim SK, Lima MA, Hung PC, Lakhdar F, Mehta N, Liu Y, Devi BI, Sudhir BJ, Lund-Johansen M, Gjerris F, Cole CH, Gottardo NG (2011) Meningiomas in children and adolescents: a meta-analysis of individual patient data. Lancet Oncol 12:1229–1239
Lakhdar F, Arkha Y, El Ouahabi A, Melhaoui A, Rifi L, Derraz S, El Khamlichi A (2010) Intracranial meningioma in children: different from adult forms? A series of 21 cases. Neurochirurgie 56:309–314
Li X, Zhao J (2009) Intracranial meningiomas of childhood and adolescence: report of 34 cases with follow-up. Childs Nerv Syst 25:1411–1417
Marosi C, Hassler M, Roessler K, Reni M, Sant M, Mazza E, Vecht C (2008) Meningioma. Crit Rev Oncol Hematol 67:153–171
Mawrin C, Perry A (2010) Pathological classification and molecular genetics of meningiomas. J Neurooncol 99:379–391
Mehta N, Bhagwati S, Parulekar G (2009) Meningiomas in children: a study of 18 cases. J Pediatr Neurosci 4:61–65
Menon G, Nair S, Sudhir J, Rao BR, Mathew A, Bahuleyan B (2009) Childhood and adolescent meningiomas: a report of 38 cases and review of literature. Acta Neurochir 151:239–244, discussion 244
Santos MV, Furlanetti L, Valera ET, Brassesco MS, Tone LG, de Oliveira RS (2012) Pediatric meningiomas: a single-center experience with 15 consecutive cases and review of the literature. Childs Nerv Syst. doi:10.1007/s00381-012-1823-8
Shah MV, Haines SJ (1992) Pediatric skull, skull base, and meningeal tumors. Neurosurg Clin N Am 3:893–924
Thuijs NB, Uitdehaag BM, Van Ouwerkerk WJ, van der Valk P, Vandertop WP, Peerdeman SM (2012) Pediatric meningiomas in The Netherlands 1974–2010: a descriptive epidemiological case study. Childs Nerv Syst 28:1009–1015
Tufan K, Dogulu F, Kurt G, Emmez H, Ceviker N, Baykaner MK (2005) Intracranial meningiomas of childhood and adolescence. Pediatr Neurosurg 41:1–7
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Burkhardt, JK., Neidert, M.C., Grotzer, M.A. et al. Surgical resection of pediatric skull base meningiomas. Childs Nerv Syst 29, 83–87 (2013). https://doi.org/10.1007/s00381-012-1906-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-012-1906-6